Pulmonary tumor thrombotic microangiopathy (PTTM) is a rare and generally fatal form of pulmonary tumor embolism that generally presents with rapidly progressing dyspnea in patients with disseminated malignant disease. Clinical diagnosis is difficult, and unfortunately PTTM is generally only confirmed post mortem.1,2
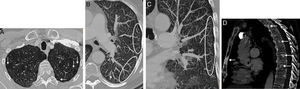
We report the case of a 58-year-old man, former smoker (20 pack-years), who presented with a 2-week history of progressive dyspnea and dry cough. Significant clinical history included prostate adenocarcinoma (Gleason score 6), treated with radiation therapy with curative intent 6 years previously, with no biochemical evidence of tumor relapse. Clinical examination revealed tachypnea and fine crackles on auscultation. Basal oxygen saturation was 88% and laboratory test findings did not suggest infection, although D-dimer levels were elevated. A chest radiograph showed bilateral diffuse interstitial involvement and prominent lung hila. Chest CT angiogram ruled out embolism on the main pulmonary, lobar or segmentary arteries, although multiple mediastinal and hilar lymphadenopathies were detected, along with severe interstitial involvement consistent with thickening of the subpleural pulmonary interstitium (Fig. 1A) and the presence of numerous centrilobular nodules and “tree-in-bud” images (Fig. 1B and C). Multiple focal bone lesions, predominantly sclerotic, were also observed in the vertebrae and sternum, consistent with metastasis (Fig. 1D). Given these radiological findings, PTTM secondary to prostate adenocarcinoma was suggested as an initial diagnosis, although other possibilities such as sarcoidosis or infection with an unusual pathogen were not ruled out. Four days after admission, the patient developed rapidly progressing respiratory failure that required urgent intubation. A few hours later, he suffered an episode of cardiorespiratory arrest with asystole and died despite prolonged attempts at cardiopulmonary resuscitation. The diagnosis of PTTM was confirmed on autopsy, which revealed an unsuspected undifferentiated occult gastric “signet ring” adenocarcinoma, with extensive metastases and multiple tumor embolisms in the small-caliber peripheral pulmonary arteries.
(A) Axial image of chest CT (pulmonary parenchymal window) showing linear thickening of the subpleural lung interstitium (arrows). (B) Maximum intensity projection (MIP) axial reconstruction (pulmonary parenchymal window) of left lung, showing a peripheral “tree-in-bud” pattern consisting of linear opacities forming predominantly subpleural branches (circled). See also the presence of small centrilobular nodules (arrow). (C) MIP coronal reconstruction (pulmonary parenchymal window) of the left lung, also showing the “tree-in-bud” pattern (circled). (D) Chest CT sagittal image (bone window) revealing multiple focal bone lesions (arrows) in the sternum and several vertebrae, consistent with bone metastases.
PTTM is a rare form of pulmonary arterial tumor embolism, in which small tumor cell embolisms cause fibrocellular proliferation in the intima of small-caliber pulmonary arteries. These changes lead to stenosis/occlusion of the pulmonary arteries and a subsequent rise in pulmonary vascular resistance, which in turn leads to rapidly progressing precapillary pulmonary hypertension.1 Clinically, patients tend to develop acute/subacute cor pulmonale and respiratory failure. Most patients who develop PTTM have documented metastatic cancer, the most common tumor being gastric adenocarcinoma followed by lung cancer, but on occasions (as in our case) it can occur in patients with no diagnosis of metastatic disease.2 In a recent review, none of the 30 cases scrutinized was due to disseminated prostate cancer.3 Unfortunately, most PTTMs are diagnosed post mortem on autopsy, and only some isolated cases have been described in surgical biopsies ante mortem. Only a high clinical suspicion and consistent radiological findings will prompt the physician to make a clinical diagnosis of PTTM and to plan the appropriate treatment, which is generally based on a combination of chemotherapy, anti-coagulants and corticosteroids.4 Significant radiological signs of PTTM described on CT include the “tree-in-bud” pattern. This is practically the only vascular cause of this radiological pattern, and should be distinguished from the bronchial presentation that is generally observed in patients with infectious bronchiolitis.5
PTTM should be suspected in oncological patients with worsening respiratory function and/or who develop acute/subacute cor pulmonale, particularly in the absence of pulmonary artery embolisms on chest CT angiogram. Detection of a “tree-in-bud” pattern without clinical signs of respiratory infection should also alert to this diagnosis.
Please cite this article as: Gorospe Sarasúa L, Ureña-Vacas A, García-Santana E. Diagnóstico radiológico de microangiopatía trombótica tumoral pulmonar: una causa no bronquial de patrón de «árbol en brote» en tomografía computarizada. Arch Bronconeumol. 2016;52:621–622.