Although patent foramen ovale is a relatively common disease, the presence of paradoxical embolism is a rare clinical condition, representing less than 2% of arterial ischemias. We report the case of a 55-year-old male diagnosed with massive pulmonary embolism and paradoxical embolism in the right arm, secondary to patent foramen ovale. We also highlight some uncertainties in the diagnosis and treatment of patients with paradoxical embolism.
Aunque la presencia de foramen oval permanente es una patología relativamente frecuente, la presencia de embolia paradójica es un cuadro clínico poco frecuente y constituye menos del 2% de las isquemias arteriales. Presentamos el caso de un varón de 55 años diagnosticado de tromboembolismo pulmonar masivo y embolia paradójica en el miembro superior derecho, secundario a foramen oval permeable. Además, pondremos de manifiesto algunas incertidumbres en cuanto al diagnóstico y tratamiento de los pacientes con embolia paradójica.
Patent foramen ovale (PFO) occurs in approximately 25% in the general population. It is usually a chance finding without clinical impact, although it has been associated with various medical events, some of them fatal.1
When pulmonary embolism (PE) appears concomitantly with PFO, the increased pressure in the right atrium may enlarge the opening, resulting in a more serious clinical situation due to the increased risk of systemic paradoxical embolization.1,2
Case ReportA 55-year-old male with no previous medical history was admitted with symptoms of sudden dyspnea and syncope, accompanied by pain in the right upper limb. During the previous week he had made long journeys (average of 6h per day). On physical examination, the only remarkable features were SatO2=91% (FiO2=21%) and coldness, pallor and lack of pulse in the upper right arm. The rest of the examination was normal.
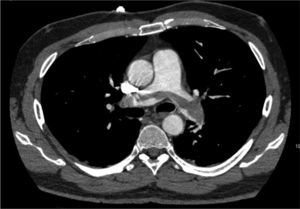
Blood test revealed a D-dimer level of 33,410 (normal<500). The electrocardiogram showed sinus rhythm at 80bpm, with a S1Q3T3 pattern. Arterial blood gas analysis revealed respiratory alkalosis and partial respiratory failure. PE was suspected, so a chest angio-CT scan was conducted (Fig. 1), in which direct evidence was observed of a massive PE that manifested as a partially recanalized thrombus straddling the two main branches, and bilateral thrombosis in segmental arteries, along with signs of right ventricular overload.
Lower limb compression ultrasonography showed deep venous thrombosis (DVT) in the left popliteal artery.
Since the findings on examination of the right upper limb were suggestive of arterial ischemia, Doppler ultrasound was performed, and the findings were consistent with significant arterial thrombosis of the right subclavian-axillary artery.
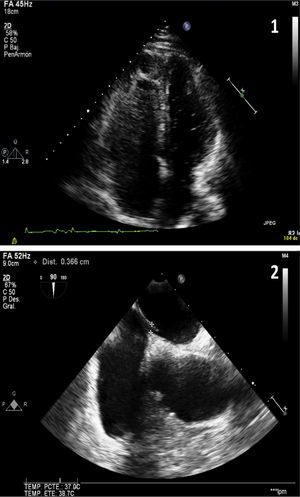
Given the suspected diagnosis of paradoxical embolism through a PFO, a transthoracic echocardiography and a subsequent transesophageal echocardiography were requested (Fig. 2). This revealed an aneurysm of the atrial septum with PFO, mild left ventricular hypertrophy and mild mitral regurgitation. Tricuspid regurgitation was not observed in any of the ultrasound examinations, so systolic pulmonary pressure could not be calculated. However, mild pulmonary insufficiency, with a mean pulmonary acceleration time of 140ms and normal mean pulmonary artery pressure of 20mmHg was detected. The diagnosis of left popliteal DVT and massive PE secondary to long traveling hours was established, with paradoxical embolism in the right arm due to PFO.
Image 1 (apical view of the four chambers obtained by transthoracic ultrasound): baseline image after injection of contrast material (agitated saline). Higher echogenicity is seen in the right ventricle and right atrium (more grayish color due to microbubbles) and, without the need of Valsalva maneuver, passive passage of microbubbles to the left heart occurs (small hyperechoic spheres). Image 2 (cross-sectional bicaval plane on transesophageal ultrasound): fossa ovalis membrane detachment of up to 3mm.
Treatment with heparin sodium was initiated, and a trans-humeral embolectomy was performed, followed by medical treatment with enoxaparin 1mg/kg every 12h. There were no complications.
The patient was discharged, and has been examined in outpatient consultation, where he underwent a thrombophilia screening that showed a heterozygous prothrombin G20210A mutation.
DiscussionPE occurs after an episode of DVT of the lower limbs when a detached thrombus reaches the pulmonary vessels. In such cases, right ventricular pressure increases where, if there is a PFO, an arterial right–left shunt may occur, favoring the onset of paradoxical embolism. In this case, there was no tricuspid regurgitation, although this would not prevent a thrombus from passing through the PFO. Different maneuvers or situations that increase the pressure level in the right cavities may favor passage. This would include the Valsalva maneuver, as was the case in this patient.
Paradoxical embolism is uncommon and causes less than 2% of arterial embolizations. PFO has been described in 30% of patients with paradoxical embolism, and several studies suggest that PFO is a risk factor for paradoxical embolism.3
For this reason, the presence of PFO should be investigated during diagnosis. The gold-standard diagnostic test is transesophageal echocardiography, since this is the most sensitive, but sometimes Doppler transthoracic echocardiography, in color or with peripheral injection of echocardiographic contrast material, is enough. An early passage of bubbles to the left side of the heart should be observed to confirm diagnosis.
Treatment is controversial. Therapeutic options include anticoagulation therapy, thrombolysis, thrombectomy, inferior vena cava filter and PFO closure. According to the clinical guidelines, PE in hemodynamically stable patients should be treated with systemic anticoagulation therapy. Low molecular weight heparins (LMWH) have been shown to be as effective and safe as unfractionated heparin (UFH). Thrombolysis should be reserved for high-risk patients with increased morbidity and mortality. Vena cava filter is indicated when systemic anticoagulation is absolutely contraindicated, or when severe bleeding secondary to anticoagulation occurs.4
With regard to PFO treatment, some authors recommend performing PFO closure. However, in a recently published multicenter study of 909 patients with a diagnosis cryptogenic ischemic stroke and PFO, in which 50.8% received solely medical treatment and the rest underwent percutaneous PFO closure followed by antiplatelet therapy, no significant differences between groups were found in the first two years of follow-up.5
Please cite this article as: Abad-Arranz M, Jara-Palomares L, Martos-Maine JL, Carrasco-Hernandez L, Ortega-Ruiz F, Otero-Candelera R. Tromboembolismo pulmonar y embolia paradójica concomitante. A propósito de un caso. Arch Bronconeumol. 2014;50:120–122.