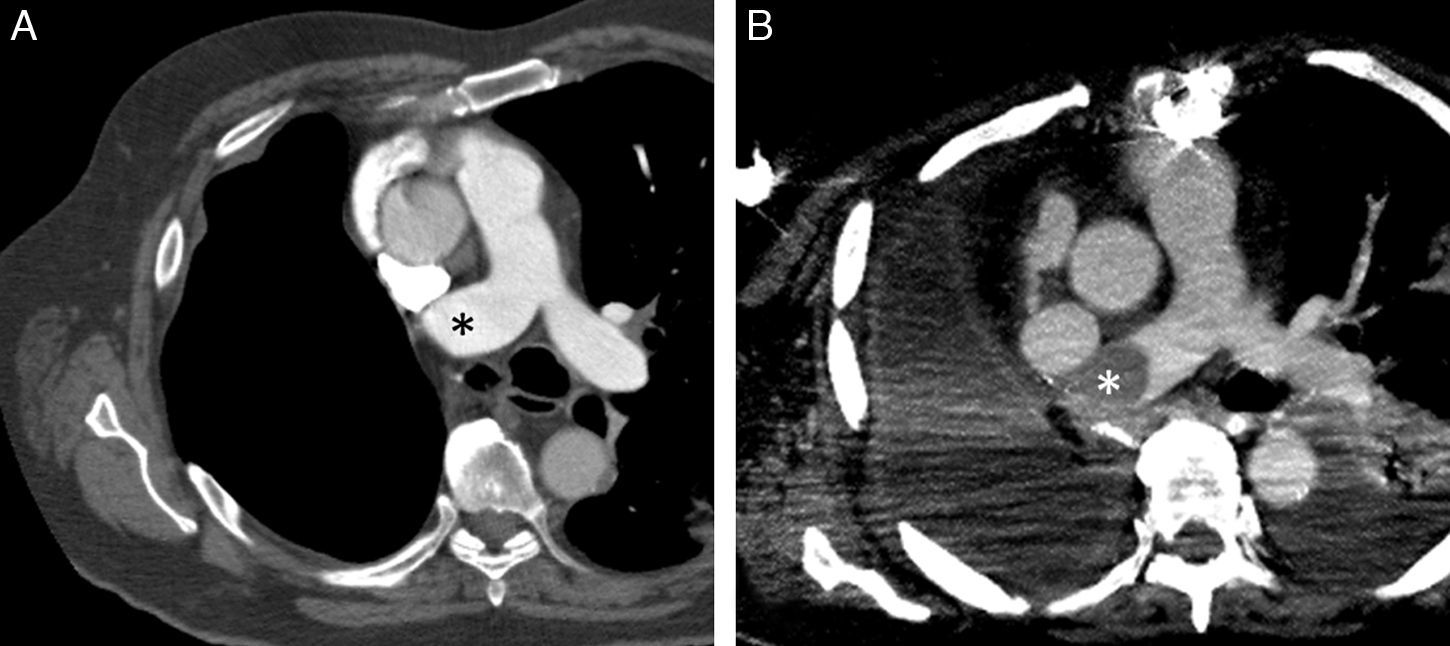
A 71-year-old man with a history of lung cancer treated by right pneumonectomy developed a bronchopleural fistula 3 months after surgery. The fistula was treated with antibiotics and chest tube drainage, while 2 attempts to seal it endoscopically with fibrin derivatives failed. Finally, we decided to close the fistula surgically with a pericardial fat pad via median sternotomy. None of the subsequent chest computed tomography studies showed evidence of thrombi on the stump of the right main pulmonary artery (Fig. 1A). However, 8 weeks after fistula repair, the patient was admitted with severe sepsis of respiratory origin, and a repeat CT revealed the appearance of a convex thrombus on the stump of the right main pulmonary artery, left pleural effusion, and opacities apparently of infectious origin in the left lung (Fig. 1B). The patient died some days later due to multiorgan failure.
(A) Axial image of chest computed tomography, 6 months after pneumonectomy, showing thrombus on main pulmonary artery stump (asterisk) with no internal filling defects. (B) Axial image of chest computed tomography, 8 weeks after bronchopleural fistula repair, showing a new convex filling defect (asterisk) in the stump of the right main pulmonary artery.
Pulmonary artery stump thrombus occurs in 12% of patients undergoing pneumonectomy, and the need for anticoagulation is a subject of debate.1 Our case is interesting because the complication appeared at a deferred stage, after a second surgical intervention to repair a bronchopleural fistula.
Please cite this article as: Gorospe Sarasúa L, Valdebenito-Montecino AP, Muñoz-Molina GM. Trombosis del muñón de la arteria pulmonar en paciente con neumonectomía derecha complicada con fístula broncopleural. Arch Bronconeumol. 2017;53:71.