Obesity hypoventilation syndrome (OHS) is a clinical entity characterized by the coexistence of obesity and hypercapnia during waking hours. However, the lack of a universally accepted definition creates confusion, since no distinctions are made between patients with different grades of severity and forms associated, or not associated, with sleep apnea-hypopnea syndrome (SAHS).1–3 Cabrera et al. proposed a severity stratification for OHS based on daytime PaO2, PaCO2, the apnea-hypopnea index (AHI), body mass index, and comorbidities, but this classification has not been associated with differences in prognosis. An earlier study published by our group in patients with a severe form of OHS, in which global respiratory failure was detected at diagnosis, found a 5-year mortality rate of 15.5%, and a 2-fold risk of death compared to patients with SAHS without diurnal hypoventilation.4 Similarly to other studies,5–7 the main cause of death was cardiovascular disease (CVD).
Masa et al. classified OHS patients in tertiles according to the number of desaturations of ≥3% per hour of recording (oxygen desaturation index, ODI). Although it differs from the AHI, the ODI should reflect the severity of the underlying SAHS, and a higher prevalence of CVD could be expected among patients with more severe SAHS, but the authors found exactly the opposite.8 They speculated that this may be because patients with more severe disease might seek medical intervention earlier, and so would receive earlier treatment for their cardiovascular risk factors. They also referred to a mechanism called “ischemic preconditioning”, in which repeated episodes of subclinical ischemia, triggered by nocturnal hypoxemia, may lead to angiogenic stimulation and the development of collateral circulation. Aside from this, the study shows that the stratification of OHS is associated with significant clinical consequences. However, no difference was made between patients with and without SAHS, who could constitute different phenotypes. Ojeda et al.,9 in contrast, did distinguish between OHS with and without SAHS, and identified more OHS patients without SAHS (OHS-nonSAHS) than with SAHS (OHS-SAHS). This study found no differences in mortality between the 2 groups (about 28% at 5 years), but a trend toward improved survival in OHS-SAHS was identified. The study was criticized for not reporting cardiovascular comorbidities in both groups before and after treatment, since this might explain the improved (but non-significant) survival among the OHS-SAHS group.
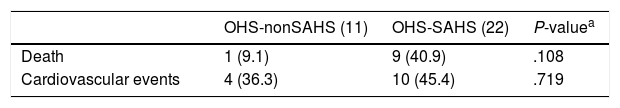
Our group designed a retrospective chart review to compare the prognosis of OHS-SAHS and OHS-nonSAHS patients (approved by the Ethics Committee of Galicia: Reg. No. 2017/079). We reviewed the medical records of 124 patients diagnosed with OHS between 1995 and 2017 using restrictive criteria: global respiratory failure at time of diagnosis and pH ≥ 7.34. Patient were matched 1:2 by date of diagnosis ±3 years, sex, and an age range of ±10 years. A total of 11 patients with OHS-nonSAHS (AHI<5) and 22 with OHS-SAHS were finally included. At baseline, there were no significant differences between patients with OHS-nonSAHS and OHS-SAHS in mean age (67 vs 68.5 years; P=.88), female sex (77.7% vs 77.1%; P=.1), average body mass index (43kg/m2 vs 42.5kg/m2; P=.81), FVC (59.5% vs 49% predicted; P=.96), baseline PaO2 (51.5±9.5mmHg vs 48±7.6mmHg; P=.25) and baseline PaCO2 (54.7±9.1mmHg vs 60.6±13.2mmHg; P=.38). Obviously, AHI was greater in OHS-SAHS patients with in OHS-nonSAHS individuals (4 vs 30; P<.001), as was the desaturation index ≥4% per hour of nighttime recording (14 vs 41; P<.001). There were no differences in time with SaO2<90% (95.5% vs 89%; P=.162). No significant differences were found in the prevalence of hypertension (72.7% in OHS-nonSAHS vs 95.4% in OHS-nonSAHS), diabetes (27.2% vs 36.3%), dyslipidemia (38.3% vs 50%), smoking (9.1% vs 13.6%), ischemic heart disease (9.1% vs 13.6%), heart failure (9.1% vs 22.7%), arrhythmias (0% vs 31.8%), cerebrovascular accidents (0% vs 4.55%) and atheromatosis (0% vs 4.5%) at the time of diagnosis, although there was a greater history of CVD in the OHS-SAHS group, which in a larger sample might have reached statistical significance. Mean follow-up was 5.4±1.5 years. All patients in the OHS-nonSAHS group received non-invasive mechanical ventilation (BiPAP, with additional oxygen in 7/11 cases), as did the majority of the OHS-SAHS patients (BiPAP initially in all, and after titration: BiPAP in 16/22, with additional oxygen in 15 and CPAP in 6 cases). There were no significant differences between OHS-nonSAHS and OHS-SAHS in the final determination of arterial blood gases: PaO2: 65±9.6mmHg vs and 72±11.6mmHg, respectively (P=.10); PaCO2: 44.3±2.5mmHg vs 43.2±3.3mmHg (P=.328). No significant differences were observed in mortality and cardiovascular events during follow-up, but there was a clear trend toward a higher incidence of both in the OHS-SAHS group (Table 1). Causes of death were CVD (6 in OHS-SAHS), cancer (1 in OHS-nonSAHS and 2 in OHS-SAHS), and sepsis (1 in OHS-SAHS). The main limitations of this study are its retrospective nature and small sample size (although all large series reflect the difficulty of finding patients with OHS without SAHS, so 11 patients constitute a reasonable sample).4,10–12 Given the trend observed in our results, a larger sample would perhaps have demonstrated significant differences in mortality and CVD events, which could be explained by greater cardiovascular comorbidities in OHS-SAHS: no patient died of respiratory failure. These results diverge clearly from those of Masa8 and Ojeda,9 although they make sense if we consider that SAHS on its own is associated with significant endothelial dysfunction, CVD, and a greater risk of risk of cardiovascular death.13–15 OHS-SAHS and OHS-nonSAHS appear to be 2 different phenotypes of the disease, and only a multicenter prospective study, which may have to be international due to the above-mentioned difficulty in recruiting nonSAHS patients, will be able to identify differences in prognoses between the two.
Number of Deaths and Cardiovascular Events by Groups.
| OHS-nonSAHS (11) | OHS-SAHS (22) | P-valuea | |
|---|---|---|---|
| Death | 1 (9.1) | 9 (40.9) | .108 |
| Cardiovascular events | 4 (36.3) | 10 (45.4) | .719 |
OHS: obesity hypoventilation syndrome; SAHS: sleep apnea-hyponea syndrome.
Data expressed in absolute frequencies and percentages.
Please cite this article as: Rodriguez Alvarez A, Méndez Marote L, Castro Añón O, Golpe Gómez R, Pérez de Llano LA. Pronóstico del síndrome de hipoventilación-obesidad con y sin síndrome de apnea obstructiva asociado. Arch Bronconeumol. 2018;54:230–231.