Sarcoidosis is a multisystem disease that generally affects young and middle-aged adults3 and is characterized by the existence of caseifying granulomas.1 The lung is the most frequently affected organ and is associated with most cases of morbidity and mortality.2 The most typical radiological findings are bilateral hilar lymphadenopathies, with or without right paratracheal lymphadenopathies, followed by a pulmonary interstitial pattern.1 Cavitation is an unusual finding in pulmonary sarcoidosis.2,3
We report the case of a 38-year-old Caucasian man, with a history of bronchial asthma in childhood, who had given up smoking 4 months previously. He consulted due to a 2-month history of morning cough, triggered by changes in environment and exercise, with mucous expectoration and occasional vomiting. Lung auscultation and lung function tests, including a walk test, were normal.
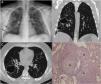
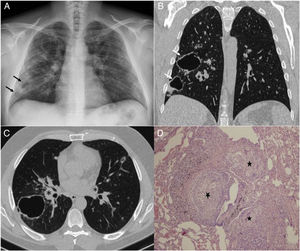
Chest X-ray revealed a bilateral diffuse interstitial pattern with no apicobasal gradient, consisting of micronodules and at least 2 cavitary lesions in the right lung base (Fig. 1A). Chest high-resolution computed tomography (HRCT) confirmed the existence of a micronodular interstitial pattern with perilymphatic distribution, in addition to multiple nodules, many of which were cavitary with a thick, smooth wall, with no signs of malignancy. These nodules were more numerous in the upper fields and larger in the right lung base, and bilateral hilar lymphadenopathies were observed (Fig. 1B and C). On the basis of the radiological findings, the differential diagnoses proposed were Langerhans cell histiocytosis, sarcoidosis, and, though less likely due to the clinical setting, tuberculous or fungal infection. Bronchial aspirate culture was negative for mycobacteria and fungi. A transbronchial biopsy was performed, and the pathology study of the samples obtained from the right upper lobe and right lower lobe showed non-necrotizing granulomatous pneumonitis, consistent with sarcoidosis (Fig. 1D).
(A) Standard chest X-ray: bilateral diffuse interstitial pattern, consisting of patchy images of increased density, predominantly in the right lung field (arrows). Chest high-resolution computed tomography (HRCT). (B) Coronal reconstruction. (C) Axial image, both with lung window: interstitial micronodular pattern with perilymphatic distribution, cavitary nodules with a thick, smooth wall (arrows) and bilateral hilar lymphadenopathies (asterisks). (D) Photomicrograph of transbronchial biopsy: lung parenchyma with numerous non-necrotizing granulomas (stars) with peribronchial distribution, consisting of epithelioid cells and multinucleated giant cells (hematoxylin-eosin, ×40).
Cavitary lung lesions are an unusual finding in sarcoidosis. Although they are found in 10% of patients at an advanced stage, along with signs of fibrosis with distortion of the lung architecture and traction bronchiectasis, they are encountered as a form of presentation in less than 0.8% of cases,1 generally in young individuals with acinar or nodular disease.1 This, then, is a diagnostic dilemma that may be underdiagnosed,2 since it requires the right clinical correlation and histologic confirmation.3 The clinical course is less symptomatic than that of other cavitary diseases.2 For diagnosis, the bacterial and fungal cultures must be negative, there must be no pleural effusion, and radiologically similar lesions such as bullae or bronchiectasis must be ruled out.2 Histologically, the cavities consist of an area of central necrosis coated with a wall of converging conglomerated sarcoid granulomas.1,2 The cavities may be present from onset, or develop months or years later. They can remain stable for a time, but they can also disappear and new cavities can form.3
Please cite this article as: Guerra ABG, Pedreira MRL, Sánchez PC, Velasco PS. Sarcoidosis cavitaria primaria, una forma extremadamente rara de presentación. Arch Bronconeumol. 2018;54:483–484.