The aims of this study were to estimate the prevalence of smoking among SEPAR members, and their approach to smoking cessation in their patients.
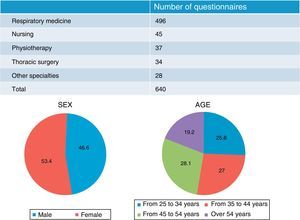
An online survey was completed by 640 members (496 pulmonologists, 45 nurses, 34 thoracic surgeons, 37 physiotherapists, and 28 other specialists). Of the members interviewed, 5% confessed that they were smokers: 3.5% pulmonologists; 8.9% nurses; 8.8% thoracic surgeons, and 13.5% physiotherapists.
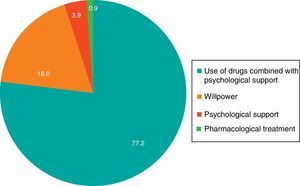
A total of 96% of members assign a lot or quite a lot of importance to setting an example; 98% of members always or often ask their patients about their smoking habit. The most effective anti-smoking intervention, according to 77% of members, is a combination of drugs and psychological support.
These results are an indicator of the awareness and commitment of SEPAR members to smoking and its cessation.
Los objetivos del estudio son estimar la prevalencia del hábito tabáquico entre los socios y las actitudes e intervenciones sobre tabaquismo que realizan los miembros SEPAR ante sus pacientes.
Se realizó una encuesta on line, a la que respondieron 640 socios (496 neumólogos, 45 enfermeras, 34 cirujanos torácicos, 37 fisioterapeutas y 28 profesionales de otras especialidades). El 5% de los socios encuestados confiesan ser fumadores: neumólogos 3,4%; enfermería 8,9%; cirujanos torácicos 8,8%; fisioterapeutas 13,5%.
El 96% de los socios dan mucha o bastante importancia a la función modélica. El 98% de los socios preguntan siempre o a menudo a sus pacientes sobre el consumo de tabaco. La intervención más eficaz para tratar el tabaquismo para un 77% de los socios es el uso de fármacos, combinado con soporte psicológico.
Estos resultados son un exponente de la firme sensibilización e implicación que los miembros SEPAR tienen frente al tabaquismo.
Worldwide, there are currently more than 1 billion tobacco smokers, and more than 6 million die every year because of their habit. Tobacco use continues to rise in developing countries, due to the steady growth of the population and aggressive marketing campaigns by the tobacco industry (TI).1 In Spain, according to data from the National Health Survey,2 24% of the population aged 15 years and over stated that they smoked on a daily basis (28% males, 20% females), Smoking, then, is the main public health issue for which prevention is a reasonable strategy.
Scientific evidence suggests that healthcare professionals (HP) can help smokers to give up their tobacco habit, thus helping to reduce the incidence of smoking-related diseases.3
Health-related behavior of HPs impacts significantly, both negatively and positively, on the adoption of healthy habits by the general population. It seems logical then that all HPs in general should appreciate the importance of their role as examples or models in the promotion of health and healthy habits, and should commit personally to adopting and demonstrating their commitment to an anti-smoking stance.4
In general, the involvement of HPs in the control and prevention of smoking has increased as prevalence of the habit in the medical profession has decreased, although there was a time in which prevalence of smoking among HPs was higher than the mean of the Spanish population (49% vs. 39%).5
In 2000, a study was conducted to determine the prevalence of smoking among members of the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) and to evaluate their characteristics and attitudes toward smoking.6 The authors found that 39.5% were former smokers, 15.1% habitual smokers, and 8.1% occasional smokers. These percentages were much lower than reported in previous studies, which found a prevalence of 47% in this group.7 Sixteen years later, the Smoking Area of our society felt that it was time to update data on the prevalence of smoking and attitudes toward this habit among SEPAR members, and accordingly designed this study. The main aims were to estimate the prevalence of smoking among our members and to characterize attitudes toward smoking and healthcare interventions for stopping smoking provided by SEPAR members to their patients.
Materials and MethodsThis study was performed on the basis of a structured online survey addressed to all 3825 SEPAR members, of whom 16.7% responded: 640 members (496 pulmonologists, 45 nurses, 34 thoracic surgeons, 37 physiotherapists, and 28 professionals from other specialties). The sample size was estimated from overall SEPAR membership data, and a total of 350 responses were needed to ensure that it was representative of the study population and achieve a precision of 4.86. However, the number of responses actually received (640) superseded this estimate, which brought the sample error down to 3.53%. Participation in the study, consisting of an online structured questionnaire based on closed questions, was voluntary. Online methodology is the most appropriate in these cases: all members are easily reached; participation is more flexible, insofar as subjects can respond to the survey at a time that bests suits them; time can be taken for completion and reflection; and the report can be collected in real time so that the sample size can be monitored. Electronic mails were sent to all members, inviting them to participate in the study, and populational proportionality in terms of respiratory medicine, nursing and physiotherapy respondents was achieved. The maximum overall sample error was estimated at 3.53%; 3.95% for pulmonologists, and 7.66% for the other members in case of maximum uncertainty (p=q). The fieldwork was conducted between November 20, 2013 and January 30, 2014. Statistical analysis of the data obtained was performed using the SPSS program. For the descriptive analysis, categorical variables were analyzed using contingency tables (frequencies and percentages) and continuous variables were analyzed using summary statistics (mean and standard deviation). Comparative analyses were conducted using the chi-squared test for categorical variables and the Student t-test or ANOVA for continuous variables. In all analyses, statistical significance was considered when the P-value was <.05.
ResultsThe total sample size was 640 SEPAR members. The breakdown by professions and the profile of professionals polled is shown in Fig. 5.
Prevalence of SmokingA total of 5% of the members successfully polled are current smokers; of these, 61% admit to being habitual smokers, while the others (39%) report that they are occasional smokers. In total, 3.4% of the pulmonologists smoke, 8.9% of nurses, and 8.8% of thoracic surgeons. The greatest percentage of smokers was found among the physiotherapists: 13.5% (P<.05). Most of the pulmonologists surveyed aged 25–34 years had never smoked: 89% (P<.05). Of the overall group of pulmonologists, 66% were never smokers.
With regard to history of smoking and sex, most female members (72%) had never smoked, while among the males, results showed that 48% had never smoked (P<.05).
With regard to age of starting smoking, 74% of respondents began to smoke at the age of between 16 and 20 years, and 7% began when they were over 25. The only professionals who began smoking after the age of 25 years were the pulmonologists (12%).
With regard to intensity of consumption, the members who were smokers reported smoking a mean of 6 cigarettes a day. Older smokers among the members interviewed were those who smoked more: around 10 cigarettes a day.
Tobacco DependenceA total of 41% of smokers lit their first cigarette within 1h of getting up. Another 59% lit up after more than 1h. Most (69%) pulmonologists interviewed waited for more than 1h before lighting their first cigarette of the day. Eleven percent of women smokers lit their first cigarette within 5min of getting up. Male pulmonologists showed less tobacco dependence than women: 83% lit their first cigarette after more than 1h of rising, compared to 60% of women.
A total of 31% of smokers successfully polled believed that the first cigarette of the day was the one they most needed and desired.
With regard to dependence associated with age, members aged 54 years and older lit their first cigarette within 5min of getting up. Respondents younger than 34 years were those that waited longest: 83% of this age group could wait for more than 1h. Smokers aged 45–54 years showed most physical dependence: 75% stated that the first cigarette of the morning was the one they needed most, much higher than the mean (P<.05). Fourteen percent of the respondents smoke more often during the initial hours after getting up.
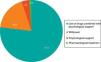
Respondents, in general, showed mild dependency, according the Fagerström test (Fig. 1).
Most of members polled (81%) never smoked at work. Three percent smoked anywhere, including inside their place of work.
Smoking Cessation: Importance and MotivationThe pulmonologists gave great importance to giving up smoking, with a score of 8.4 out of 10 points; however, their score in terms of motivation was intermediate (6.5). Smokers between 45 and 55 years of age gave more importance to giving up (9.3), and were the most motivated to do so (6.8 points out of 10).
Smoking Cessation: AttemptsA total of 35% of members who smoked had never tried to give up. Among those who had attempted, 26% had been influenced by current legislation.8 Pulmonologists formed the largest group (70%) of respondents who had attempted to give up.
Approximately 70% of women had tried to give up at some stage. Male participants were those whose decision to give up had been most influenced by current legislation (33%).8 Sixty-three percent of smokers aged between 45 and 54 years had tried to stop smoking, regardless of current legislation.
Attitudes and Aptitudes of SEPAR Members Toward SmokingA total of 79% of respondents believed that smoking is a chronic disease. The pulmonologists were the group with the greatest proportion of respondents (83%) who believed that smoking is a chronic disease. Among the active smokers, only 47% believed that smoking is a chronic disease (P<.05).
Obedience and Compliance With Current Legislation8The large majority of SEPAR members polled (99%) were in favor of banning smoking in all public places. Nearly all respondents (99%) were aware of smoking bans in public places imposed by currently applicable legislation. Among the physiotherapists, 11% of respondents were unaware that under current legislation smoking was banned in public places (P<.05).
Desire to Participate in Preventive StrategiesMost of the members polled (80%) were willing to participate in strategies aimed at preventing smoking. Among the pulmonologists, 82% were interested in participating in preventive strategies (P<.05). There were statistically significant differences in the responses from the other SEPAR member groups.
Women showed most interest in participating in strategies for preventing smoking: 84% stated their desire to participate compared to 76% of men. This difference was statistically significant (P<.05). Among the younger members (25–34 years), 87% wanted to participate in preventive strategies (P<.05).
Most of the members polled (78%) would collaborate in a “Smoke-Free Healthcare Center” program; however, 14% doubted they would do so. Among the pulmonologists, 80% would collaborate in such an initiative.
Setting an ExampleNinety-six percent of the members polled assigned a lot or quite a lot of importance to setting an example, while 3% thought it was of little importance. Among the respondents over 54 years of age, 78% assigned a lot of importance to setting an example, compared to 46% of members aged 25–34 years (P<.05).
Twenty-one percent of the habitual smokers assigned a lot of importance to setting an example (P<.05).
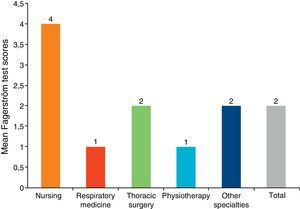
Anti-Smoking Interventions Provided by SEPAR MembersNinety-eight percent of respondents always or often ask their patients about their smoking habit (Fig. 2).
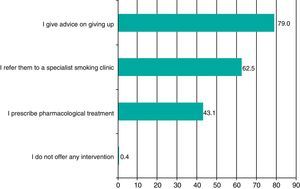
Pulmonologists are the group that most often ask their patients about tobacco use: 95% always do. Most (88%) respondents always give advice on stopping smoking to patients who present with symptoms, in contrast to 2% who only do so occasionally. Seventy-five percent of respondents assigned a lot of importance to giving advice on cessation to patients who smoke. Among pulmonologists, the most common strategy with a patient who states their desire to make a serious attempt to stop smoking is to give advice (79%). Forty-three percent also include the prescription of drug treatment in their intervention (Fig. 3).
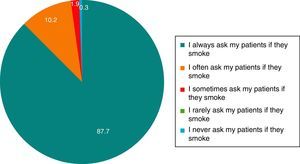
The most effective smoking cessation intervention, in the opinion of 77% of respondents, is the use of drugs combined with psychological support (Fig. 4). This option is considered the most effective by 82% of pulmonologists, and 86% of the former smokers support this option..
DiscussionHealthcare professionals play an important role in interventions aimed at the prevention and treatment of smoking; however, due to limitations and poor training, patients are not receiving all the help they need.9
It is important to point out that only 5% of the members interviewed are current smokers. These results confirm that SEPAR members are fully aware and committed to the fight against smoking, particularly if these figures are compared with a similar study performed previously among personnel from the Spanish National Health System (INSALUD),10 of which 39% were smokers, 28% were former smokers, and 33% never smokers. Our smoking rates have fallen even lower if we compare them with another study in Spanish healthcare workers, performed by the Smoking Prevention Committee of SEPAR,5 which reported that 49% of medical staff were smokers, while 35% of pulmonologists – who already considered it important to set an example – were smokers. The results are even more encouraging if we compare them with those of another study of SEPAR members, in which 15% of respondents stated they were smokers, 11% of whom were pulmonologists.6 We have also achieved better results when our data are compared with a recent study of Spanish healthcare professionals conducted by the Smoking PII group, which reported a rate of smoking of 11.7% among participants.11
In this study, the number of cigarettes smoked per day was 6; this number has also fallen remarkably from the 15 cigarettes/day reported in the earlier study.6
In terms of tobacco dependence, over half of the smokers, i.e., 59%, light up their cigarette more than 1h after getting up, and respondents in general showed a low score in the Fagerström tests, all of which suggests a mild physical dependence on nicotine.12
Thirty-five percent of our smoking respondents have never tried to give up, while 70% of the group of pulmonologists had attempted on at least 1 occasion, and were also more motivated to do so. Current legislation seems to have impacted on these behaviors.8 According to 2 studies on active smoking among doctors and nurses in the Community of Madrid conducted in 1998 (doctors 43.1%; nurses 47.6%) and 2001 (doctors 43%; nurses 47%),13,14 before current anti-smoking legislation came into force, smoking figures were largely similar in both study periods. However, a more recent study15 aimed at estimating changes in tobacco use among healthcare professionals over a 10-year period (2001–2011) found that overall prevalence among doctors fell from 26% to 19% (P=.005), and among nurses from 35% to 26% (P=.007). The authors conclude that this reduction in tobacco use coincides with the measures introduced after changes were implemented following the approval of Law 28/2005 and current legislation.8
With regard to the perception of smoking, 83% of pulmonologists consider it a chronic disease. In contrast, this is the understanding of only 58% of healthcare professionals in Spain, and up to 35% consider it to be a bad habit.11
The large majority (99%) of respondents agree that smoking should be banned in public places and are aware of current legislation.
Eighty-two percent of pulmonologists would be willing to participate in preventive strategies (P<.05), and 78% would collaborate in a “Smoke-Free Healthcare Center” initiative, indicating that they are aware of strategies to prevent smoking.
A very large majority (96%) of our members who responded attributed a lot or quite a lot of importance to setting an example. This contrasts sharply with the findings of a study performed in hospital personnel, in which 40% believed that their function as a role model had limited influence, 27% thought they had no influence at all, and only 11% thought they had a lot of influence over the general population.16 It is remarkable that, in our study, when smokers responded to this question, they appeared to be less conscious of their role, with only 21% of them giving a lot of importance to setting an example (P<.05).
In terms of clinical interventions, pulmonologists are the group which most often asks their patients about tobacco use: 95% always do so, compared to 56% of Spanish healthcare professionals, as reported in the previously cited study.11 For 82% of pulmonologists, the most effective smoking cessation intervention is pharmacological therapy combined with psychological support. This shows that pulmonologists are very aware of this epidemic, are familiar with practical guidelines in the treatment of smoking, and put the recommendations into practice.9
One limitation of our study is the sample size. The study sample comprises 640 individuals, representing 16.7% of the total study population. However, it should be noted that the acceptable sampling error in this type of study with online methodology is 4.86%. The sample size finally obtained and analyzed in this study would only allow an error of 3.53%. This validates our results, as the sampling error is lower than that normally admitted in studies using similar methodology.
We conclude that the prevalence of smoking among SEPAR members is lower than that among other healthcare professionals in our country. It is interesting to point out mean consumption figures among the pulmonologists: 3.4% of them smoke, they are the group which smoked fewest cigarettes a day, and generally have low nicotine dependence. Pulmonologists represent the highest percentage of members who have tried to give up smoking. The majority of respondents expressed a marked willingness to participate in strategies to prevent individuals from taking up the habit, and they also attributed great importance to setting an example, that is, to hold themselves up as non-smokers in the eyes of the general public. The great majority of them ask their patients about their smoking habit and advise them to give up, while providing psychological support combined with specific pharmacological treatment, if indicated. The excellent attitude and approach of the members of SEPAR are indicators of their raising awareness, conscientiousness and commitment to promoting the control, prevention and treatment of smoking.
In the public health field, the detection of tobacco use and smoking cessation interventions are among the most cost-efficient of all clinical services. Planning and implementing training programs in smoking cessation intervention, and cessation by those professionals who do continue to smoke are, then, highly recommendable. Finally, we will end by pointing out that in countries where healthcare professionals have given up smoking, smoking among the general population falls significantly.
FundingWe thank Laboratorios Pfizer for sponsoring this study.
Conflict of InterestsThe authors state that they have no conflict of interests.
Please cite this article as: Solano Reina S, Jiménez Ruiz CA, de Higes Martinez E, Garcia Rueda M, Callejas González FJ, de Granda Orive JI, et al. Prevalencia, conocimiento y actitudes acerca del consumo de tabaco en los miembros de SEPAR. Arch Bronconeumol. 2016;52:605–610.