The prevalence of chronic obstructive pulmonary disease (COPD) varies significantly among the different geographical areas reported. In Spain, two epidemiological studies have shown a prevalence of 9–10% in the population aged over 40. However, neither of these studies included the Canary Islands, which are of interest due to their climatic conditions and high incidence of smoking.
Materials and methodsA random group of 1353 subjects aged between 40 and 70years was selected from a sample population of 596478 individuals. Participants completed a questionnaire and then performed spirometry with bronchodilator testing if obstruction was observed. COPD was diagnosed when the post-bronchodilator FEV1/FVC ratio was less than 0.70.
ResultsThe prevalence of COPD was 7.3% (95%CI: 5.5–9.5) and was higher in males than in females (8.7% vs 6.3%, P=.134). The incidence of smoking was 29.4% (95%CI: 25.4–33.1) and was also higher in males than in females (35.1% vs 25.4%, P<.001). The prevalence of COPD stratified by severity of obstruction, according to the GOLD criteria, was 16% in group I, 69.9% in group II, 10.4% in group III and 3.3% in group IV. 71.6% of the subjects were underdiagnosed and 63.5% undertreated.
ConclusionsDespite having one of the highest rates of smoking in Spain, the prevalence of COPD in the Canary Islands is lower than in most of the Spanish regions studied.
La prevalencia de la enfermedad pulmonar obstructiva crónica (EPOC) varía considerablemente entre las diferentes áreas geográficas estudiadas. En España hay 2estudios epidemiológicos que muestran una prevalencia entre el 9 y el 10% en población mayor de 40años. No obstante, ninguno de ellos ha incluido a las Islas Canarias, región de interés por sus características climáticas y su alta prevalencia de tabaquismo.
Material y métodosA partir de una muestra poblacional de 596.478 personas se seleccionó una muestra aleatorizada de 1.353 individuos entre 40 y 70años. Los participantes rellenaron un cuestionario y posteriormente realizaron una espirometría con test de broncodilatación si existía obstrucción. Se diagnosticó EPOC cuando el cociente FEV1/FVC después de la broncodilatación era menor de 0,70.
ResultadosLa prevalencia de EPOC fue del 7.3% (IC95%: 5,5–9,5), siendo mayor en varones que en mujeres (8,7% vs 6,3%, p=0,134). La tasa de tabaquismo fue del 29.4% (IC95%: 25,4–33,1), también mayor en los varones que en las mujeres (35.1% vs 25.4%, p<0,001). La prevalencia de EPOC estratificada según la gravedad de la obstrucción, en base a los criterios GOLD, fue del 16% en el grupoi, del 69,9% en elii, del 10,4% en eliii y del 3,3% en eliv. El infradiagnóstico fue del 71,6% y el infratratamiento, del 63,5%.
ConclusionesA pesar de tener una de las tasas de tabaquismo más altas de España, la prevalencia de EPOC en las Islas Canarias es menor que en la mayoría de las zonas españolas estudiadas.
Chronic obstructive pulmonary disease (COPD) is a worldwide health problem causing high morbidity and mortality in the adult population. However, COPD is frequently underdiagnosed and undertreated, and its impact on the healthcare system is difficult to quantify.1 Moreover, the worldwide prevalence of this disease continues to grow, and it is expected to become the third most common cause of death by 2020.2 Despite numerous studies in the area, the prevalence of COPD has not been fully defined and estimates vary widely depending on the geographical regions under study.3–5 Validated tools have been developed in recent years allowing reliable and reproducible epidemiological studies to be carried out, irrespective of the geographical region and available financial resources.3,4 These studies were carried out according to the consensus paper of the American Thoracic Society (ATS) in association with the European Respiratory Society (ERS) and the Global initiative for chronic Obstructive Lung Disease (GOLD) guidelines (2010).6,7 Two epidemiological studies on EPOC have been carried out in Spain: IBERPOC and EPISCAN (revealing a prevalence of 9.1 and 10.2%, respectively).8–10 Notwithstanding, neither of these studies included prevalence rates in the Canary Islands, a region that may be of interest due to its high smoking rates (around 30%) and its particular climatic characteristics.11 The aim of this study was to determine the prevalence of COPD in the Canary Islands, and to stratify the data according to the various variables of interest, risk factors and percentages of underdiagnosis and undertreatment.
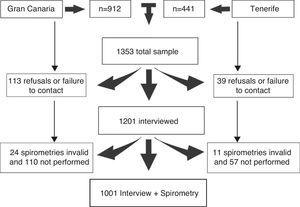
Materials and MethodsSampleThis was a cross-sectional study conducted in urban populations in the 2 largest islands of the archipelago: Gran Canaria and Tenerife (Hospital Universitario de Gran Canaria Dr. Negrín and Hospital Universitario de Canarias). The participating cities in Gran Canaria were Las Palmas de Gran Canaria, Arucas and Gáldar, with a population of 444526 inhabitants, while in Tenerife, the city studied was La Laguna (152222 inhabitants). The total sample comprised of 596478 subjects, representing 27.2% of the population of the Canary Islands (2118519 inhabitants).11 The sample size was calculated using an estimated COPD prevalence of 10%, with a sample error of ±1.91% (95% confidence interval [CI]) with an estimated non-response rate of 30%. The minimum number of subjects for inclusion was 947. The first sample unit was constructed from the randomized selection of census tracts from the above-mentioned urban municipalities or metropolitan areas. A total of 69 census tracts (36 in Gran Canaria and 22 in La Laguna, Tenerife) were selected. Since each census tract covers a limited geographical area, the second sampling unit was defined as randomized routes within the limits of each census tract, with a randomized starting point within each of the tracts. Finally, all subjects between 40 and 70 years of age residing in the dwelling and who met the inclusion criteria were selected. If the selected subject(s) were not at home at the time of the first visit, the visit was repeated up to 3 times. The exclusion criteria included mental illness, incapacity to complete the questionnaire or spirometry and institutionalization in healthcare facilities or prisons. The study was approved by the ethics committees of both the Hospital Universitario de Gran Canaria Dr. Negrín and the Hospital Universitario de Canarias, and all participants signed informed consent before starting the study.
Questionnaire and SpirometrySubjects who agreed to participate completed an extensive questionnaire in their homes. This questionnaire included questions on demography, smoking habit, biomass exposure, education, comorbidities, respiratory symptoms and quality of life. The same questionnaire was used in the PLATINO study (The Latin American Project for the Investigation of Obstructive Lung Disease) and is an amalgam of several previously validated questionnaires.12 Interviewers were trained professionals not involved in healthcare activities, and their activity was submitted to quality control checks by qualified inspectors who reviewed all the interviews carried out. Subjects who refused to participate in the study were asked to complete a short questionnaire that included questions on demography (age, sex) and smoking habit.
Subjects who completed the long questionnaire were given an appointment for spirometry within the next 15 days in one of the participating hospitals. If for any reason the subject could not attend the hospital, spirometry was performed at home. Spirometries were carried out by a pulmonologist or by nurses with over 15 years’ experience in performing lung function tests. The device used in both the hospital and in the patients’ homes was a portable spirometer (Easyone® NDD, Medical Technologies, Chelmsford, Massachusetts and Zurich, Switzerland). This same spirometer was used in both the PLATINO study and in the BOLD study (The Burden of Obstructive Lung Disease), and has been internationally validated.13,14 The ERS/ATS recommendations for standardized spirometry and the ATS/ERS 2004 recommendations (coinciding with those from the GOLD document)15,16 were used for the diagnosis and classification of the severity of obstruction. All spirometries were reviewed and interpreted by 2 pulmonologists participating in the study.
COPD was diagnosed when the FEV1/FVC ratio after the bronchodilator test was less than 0.7. The bronchodilator test was carried out with a spacer device administering 200μg salbutamol, and the spirometry was repeated after 15 minutes. COPD patients who had never been previously diagnosed with emphysema, chronic bronchitis or COPD were considered underdiagnosed. Undertreatment was defined as treatment for subjects with a diagnosis of COPD who had never been advised to quit smoking or given medication for their disease. An ex-smoker was defined as someone who had given up smoking at least 6 months before the interview, and never smokers were those who had smoked less than 0.1 pack years.
Statistical AnalysisCOPD prevalences were calculated as percentages with 95% CI and were standardized for age and sex with the reference Canary Island population.11 This was subsequently standardized with the world population.17 Calculations were adjusted taking into account that a lower percentage of smokers participated in the spirometry. Similarly, prevalence was estimated according to the categorical variables of sex, age groups, body mass index (BMI), smoking habit, geographical area, social stratum, respiratory diseases in childhood and adolescence, family history of respiratory diseases, educational level and environmental exposure (other than tobacco smoke). COPD risk factors were analyzed using a logistic regression model. A P-value of <.05 was considered significant. The SPSS 15.0 statistical software package was used (SPSS Inc., Chicago, U.S.).
ResultsDemographic SampleThe final sample included 1353 subjects, of whom 1001 completed the long questionnaire and performed spirometry correctly (Fig. 1). The total non-response rate was 26% (31% in Tenerife and 28.1% in Gran Canaria, P<.05). Regarding spirometries, 95% were carried out in the hospitals (52 tests were carried out in the home by the same nurses, using the same spirometer and the same technique). Of the 33 invalid study spirometries, only 5 were carried out at home. The mean age of the subjects who refused to participate in the study was lower than that of the subjects who performed the spirometry (53.5±8.5 vs 55.1±8.6 years, P<.05). The characteristics of the subjects who refused to participate and of those who completed the questionnaire and successfully performed spirometry are summarized in Table 1.
Characteristics of Subjects Who Refused to Participate, Who Completed the Questionnaire but did not Perform the Spirometry, and Who Completed the Study (Sex, Age and Smoking Status).
| Refusal to participate | Questionnaire without spirometry | Questionnaire with spirometry | P | |
| n=132 | n=200 | n=1001 | ||
| n (%) | n (%) | n (%) | ||
| Sex: male | 60 (45.5) | 92 (46) | 399 (39.9) | .22 |
| Age, years,amean±SD | 53.5±8.5 | 51.9±8.5 | 55.1±8.6 | .044 |
| 40–49 years | 50 (37.5) | 97 (48.5) | 322 (32.2) | |
| 50–59 years | 45 (34.2) | 56 (28) | 325 (32.5) | |
| 60–70 years | 37 (28.3) | 47 (23.5) | 354 (35.4) | |
| Smoking status | ||||
| Current smoker | 90 (68.2)b | 90 (45) | 294 (29.4) | .009 |
| Ex-smoker | 40 (20) | 269 (26.9) | ||
| Never smoker | 42 (31.8) | 70 (35.0) | 438 (43.8) | |
The proportion of smokers was 29.4% (95% CI: 25.4–33.1), while 26.9% of the subjects were ex-smokers (95% CI: 23.4–29.2) and 43.8% were never smokers (95% CI: 40.4–49.2). Significant differences between males and females were observed in all groups, whether smokers (35.1% vs 25.4%, P<.001) or ex-smokers and never smokers (P<.001). Of the subjects who refused to participate, 68.2% were smokers or ex-smokers, while 56.2% of smokers or ex-smokers finally carried out the spirometry.
Prevalence of Chronic Obstructive Pulmonary Disease and Risk FactorsThe raw prevalence of COPD was 7.4% (8.4% in Gran Canaria [95% CI: 6.4–10.6] and 6.1% in Tenerife [95% CI: 3.8–88], P=.162). Prevalence adjusted for age, sex and smoking status was 7.3% (95% CI: 5.5–9.5). The proportion of males diagnosed with COPD was greater than females (8.7% [95% CI: 5.8–12.7] vs 6.3% [95% CI: 4.7–8.4], P=.134), but no significant differences were observed when a logistic regression model analysis adjusted for age and smoking habit was made (Table 2). Prevalence adjusted to the world population was 6.4% (95% CI: 4.8–8.6). Of the 73 subjects with COPD, 16 had a positive bronchodilator test without full reversal of the obstruction (22% of those diagnosed). A previous diagnosis of asthma was found in 5% of the smoker/ex-smoker group and in 50% of the never smokers. Prevalence varied depending on smoking status, from 2.5% (95% CI: 1.2–5.2) in never smokers up to 14.3% (95% CI: 9.7–20.6) in current smokers; the prevalence also increased in line with increases in the pack year index (PYI): from 1.7% (95% CI: 0.9–3.2) in subjects with PYI<0.1 up to 20.5% (95% CI: 15.1–27.1) in those with PYI>30.
Diagnosis of COPD is clearly associated with age and prevalence increases in line with age, in both men and women, irrespective of smoking status. Among subjects with a diagnosis of COPD who had never smoked, only one was younger than 60 years. Most diagnosed subjects had grade iiobstruction according to the GOLD criteria (69.9%; 95% CI: 57.1–80.2), while the figures were lower for obstruction grades iii and iv (10.4%; 95% CI: 5.5–18.7, and 3.3%; 95% CI: 0.6–17.0, respectively). There were no non-smokers in this final group (Table 3). There is an inverse relation between prevalence of COPD and BMI (P=.001), irrespective of PYI, with the highest prevalence of COPD being observed in subjects with a BMI of between 20 and 24.9, and the lowest in those with a BMI greater than 30 (10.5%; 95% CI: 6.5–16.6 vs 3.0%; 95% CI: 1.5–5.9; P<.05). No subgroup analysis could be made in the subgroup with a BMI of less than 20 due to the small number of subjects. However, the trend clearly suggests that COPD is more prevalent in this group. Both age and PYI are significant risk factors (Table 4).
Prevalence of Chronic Obstructive Pulmonary Disease (COPD) With 95% Confidence Interval (CI): Total Prevalence in General Population, Prevalence Within the COPD Group and by Smoking Status, According to GOLD Obstruction Levels.
| Overall | % In COPD Group | Never smokers | Ex-smokers | Current smokers | |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Stage I | 1.2 (0.6–2.1) | 16.4 (8.5–29.4) | 0.4 (<0.01–1.7) | 1.2 (0.2–3.2) | 2.3 (0.9–4.7) |
| Stage II | 5.1 (3.8–6.6) | 69.9 (57.1–80.2) | 1.8 (0.8–3.6) | 4.7 (2.6–8.1) | 10 (6.8–13.9) |
| Stage III | 0.8 (0.3–1.6) | 10.4 (5.5–18.7) | 0.4 (<0.01–1.7) | 0.8 (0.1–2.6) | 1.2 (0.4–3.4) |
| Stage IV | 0.2 (0.02–0.7) | 3.3 (0.6–17.0) | 0 | 0.1 (<0.01–0.1.7) | 0.7 (0.1–2.4) |
Risk Factors for Chronic Obstructive Pulmonary Disease: Odds Ratio (OR) and 95% Confidence Interval (CI).
| Variablesa | OR (95% CI) | P |
| Pack years | 1.02 (1.02–1.036) | <.001 |
| BMI | ||
| <20 | 9.58 (1.02–1.036) | .011 |
| 20–25 | 5.45 (2.56–11.61) | <.001 |
| 26–30 | 3.23 (1.59–6.60) | .001 |
| >30b | – | |
| Age, years | ||
| 40–49b | – | |
| 50–59 | 1.32 (0.63–2.80) | .046 |
| 60–70 | 3.33 (1.55–7.13) | .002 |
| Sex: male | 1.52 (0.88–2.61) | ns |
| Educational level | 0.92 (0.72–1.18) | ns |
| Workplace exposure | 0.94 (0.546–1.626) | ns |
| Childhood hospitalizations for pulmonary disease | 2.3 (0.3–13.9) | ns |
| Domestic exposure to wood or coal smoke | 0.73 (0.38–1.41) | ns |
ns: not significant.
The percentage of underdiagnosis of COPD is below 71.6%, and is more common in the milder obstruction grades (GOLD 2010): 81.8% in stage I vs 33% in stage IV, P<.001). Undertreatment was found in 63.5%, with a greater proportion of more severe patients being treated than less severe patients (81% underdiagnosis in stage I vs 33% in stage IV, P<.001).
DiscussionThis study provides data on the heterogeneity of the prevalence of COPD. The prevalence of COPD is lower than the rates established in the IBERPOC and EPISCAN studies in the overall Spanish population, or in the BOLD or PLATINO studies. Similarly, if we compare our study with other epidemiological studies conducted in large samples in individual countries,5,18 our prevalence is also lower, despite a similar or greater proportion of smokers/ex-smokers. In the two Spanish studies, the prevalence of COPD in the overall sample was 9.1% in IBERPOC and 10.2% in EPISCAN, higher that that found in the Canaries. It is difficult to establish a comparison between our study and IBERPOC, due to the different diagnostic criteria used. In both our study and the EPISCAN study, the criteria for disease diagnosis were based on the GOLD criteria; however, the age range in EPISCAN was between 40 and 80 years, and it is well known that an FEV1/FVC ratio of <70% does not necessarily indicate obstruction in the elderly population. This may have produced a significant increase in COPD prevalence. In parallel with international studies, neither smoking (in the Canaries the proportion of current smokers was 29.4%, while in EPISCAN it was 26%), nor environmental pollution19 are variables that can explain the low prevalence of COPD in the Canaries compared to that observed in the other Spanish studies. The relationship between pollution and COPD prevalence has been ruled out by various studies. The PLATINO and BOLD studies, for example, showed that cities with low levels of pollution, such as Montevideo or Salzburg, have a higher COPD prevalence than Mexico DF or Shanghai, which have the highest levels of pollution in the world. Nor is the use of biomass fuel a plausible explanation, since its use in our community is similar to that in the cities included in the PLATINO and BOLD studies. Similarly, one possible explanation for low prevalence in the Canaries may be climatic factors. The islands have a temperate, subtropical climate all year round, with mild seasons, little variation in temperatures and moderate environmental humidity. This mild climate could contribute to reducing the development and severity of respiratory symptoms and exacerbations. The relationship between low vitamin D levels and COPD severity has been described recently.20 Considering that exposure to sun in the Canary Islands is greater than in the rest of Spain, it may be speculated that high vitamin D levels in our population may cause the disease to be more stable.
With regard to undertreatment and underdiagnosis, the rates found were slightly lower than those from IBERPOC, but somewhat higher than those observed in EPISCAN. These data may be explained by patients minimizing symptoms and thus preventing them from seeking medical advice in the early stages of the disease, and also by poor care on the part of physicians, that would lead to failure to detect the disease in its early stages. Undertreatment and underdiagnosis go hand-in-hand. In this aspect, our study is similar to other international epidemiological studies showing a high rate of COPD underdiagnosis.21,22
The use of a fixed ratio for the diagnosis of COPD can cause problems in epidemiological studies. Overdiagnosis of COPD in the elderly is a well-recognized phenomenon when GOLD criteria are used instead of the lower limit of normality (LLN).23 In this study, this phenomenon is clear in the case of non-smokers with a diagnosis of COPD. Perhaps if the LLN had been applied, the number of subjects with a diagnosis of COPD that had never smoked would have been largely reduced, putting even more emphasis on the role of smoking in the development of COPD. Indeed, of the diagnosed subjects who never smoked, 50% had had a previous diagnosis of asthma. This indicates that the prevalence of COPD in the non-smoking population is secondary to diseases such as asthma, thus underlining the confusion surrounding the term COPD, which is understood indiscriminately as a spirometric pattern or else the term for a specific disease.24 Subjects with a diagnosis of COPD in epidemiological studies can present some type of lung disease that involves an irreversible airway obstruction pattern, since the different types of obstruction cannot be distinguished by spirometry. This limitation means that diagnosed patients can present a wide range of diseases grouped under the umbrella term COPD. This differentiation between the various causes of airway obstruction has been recently recognized in the ATS/ERS guidelines for the treatment of stable COPD,25 in which a distinction is made between COPD (composed of a clinical entity and a compatible spirometry) and a simple pattern of irreversible obstruction on spirometry.
Another important result from our study is the low prevalence of COPD in the population with a BMI>30. Certainly, the proportion of subjects with COPD shows a linear relation with BMI, with a prevalence of 10.5% in subjects with BMI between 20 and 25 and only 3.3% in subjects with BMI>30 (adjusted for age, sex and pack years, P>.005). These results are similar to those found by Ran et al.,26 who reported that in these patients, the lower the BMI, the lower the prevalence of COPD. This association between COPD prevalence and BMI merits future investigation.
One of the limitations of our study is the inclusion of exclusively urban subjects, with the exclusion of rural areas. However, at least 80% of the population of the Canary Islands live in urban areas. Another limitation is the difference between the rate of smokers who answered the questionnaire and who subsequently completed the spirometry. The effect of this difference was minimized by giving greater specific weight to the group of smokers in the statistical analysis. The non-response rate was observed principally in the younger population group, so in our opinion this has not significantly affected the final prevalence.
To conclude, this is the first study to report data on the prevalence of COPD and its risk factors in the Canary Islands. Despite the high rate of smoking in this region, a lower prevalence of COPD was observed compared to the overall national territory of Spain. This finding may be due to the particular climatic factors of the islands.
FundingThis study was funded by Boehringer Ingelheim GmbH. This company had no role in the design and conduct of the study or in the preparation of this article.
Conflict of InterestsThis study was sponsored by Boehringer Ingelheim.
Please cite this article as: Cabrera López C, Juliá Serdá G, Cabrera Lacalzada C, Martín Medina A, Gullón Blanco JA, García Bello MÁ, et al. Prevalencia de enfermedad pulmonar obstructiva crónica en las Islas Canarias. Arch Bronconeumol. 2014;50:272–277.