Cell block material from puncture can be obtained with endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) in many cases. The aim of this study was to analyze the value of additional information from cell blocks obtained with EBUS-TBNA samples from mediastinal and hilar lymph nodes and masses.
MethodsReview of pathology reports with a specific diagnosis obtained from EBUS-TBNA samples of mediastinal or hilar lesions, prospectively obtained over a two-year period. The generation of cell blocks from cytology needle samples, the contribution to morphological diagnosis, and the possible use of samples for immunohistochemistry were analyzed.
ResultsOne hundred and twenty-nine samples corresponding to 110 patients were reviewed. The diagnosis was lung cancer in 81% of cases, extrapulmonary carcinoma in 10%, sarcoidosis in 4%, lymphoma in 2.7%, and tuberculosis in 0.9%. Cell blocks could be obtained in 72% of cases. Immunohistochemistry studies on the cell blocks were significantly easier to perform than on conventional smears (52.6% vs 14%, P<.0001). In 4 cases, the cell block provided an exclusive morphological diagnosis (3 sarcoidosis and one metastasis from prostatic carcinoma) and in 3 carcinomas, subtype and origin could be identified. Exclusive diagnoses from the cell block were significantly more frequent in benign disease than in malignant disease (25% vs 0.9%, P=.002).
ConclusionsCell blocks were obtained from 72% of EBUS-TBNA diagnostic procedures. The main contributions of cell blocks to pathology examinations were the possibility of carrying out immunohistochemical staining for the better classification of neoplasms, especially extrapulmonary metastatic tumors, and the improved diagnosis of benign lesions.
La punción transbronquial guiada por ecoendoscopia permite obtener bloques celulares a partir del material de punción. Nuestro objetivo fue analizar su contribución al diagnóstico citológico convencional.
MetodologíaRevisión retrospectiva de las punciones por ecobroncoscopia realizadas de forma consecutiva durante 2 años con diagnóstico específico. Se analizó la capacidad de generar bloques celulares, su contribución al diagnóstico y a la realización de técnicas de inmunohistoquímica.
ResultadosSe revisaron 129 muestras de lesiones correspondientes a 110 pacientes. En el 91% el diagnóstico fue de malignidad. Las lesiones puncionadas más frecuentemente fueron las adenopatías 4R (28%) y subcarinal (21%). El 72% de las muestras se procesaron como bloque celular, siendo su capacidad para realizar técnicas de inmunohistoquímica significativamente mayor a la de las muestras citológicas (52,6% vs. 14%, p<0,0001). En 4 casos el bloque permitió un diagnóstico morfológico exclusivo (3 sarcoidosis y una metástasis de adenocarcinoma prostático) y en 3 carcinomas definir el subtipo y origen. El diagnóstico exclusivo mediante bloque celular fue significativamente más frecuente en la patología benigna que en la maligna (25% vs. 0,9%, p=0,002).
ConclusionesLa obtención de bloque celular a partir de muestras de punción por ecobroncoscopia fue del 72%. Sus principales aportaciones fueron la mejora del diagnóstico de lesiones benignas y la capacidad para realizar técnicas de inmunohistoquímica cuya contribución es esencial para la tipificación de neoplasias.
The recent introduction and generalized use of new diagnostic and staging tools, particularly positron emission tomography combined with computed tomography (PET-CT) and endoscopic ultrasound (EUS), have improved efficiency in the diagnosis of mediastinal node involvement, sidelining the use of more aggressive and costly tests such as surgical examination of the mediastinum.1
The incorporation of real-time endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has led to a considerable improvement in the validity and the safety of this relatively non-invasive diagnostic test, while maintaining an excellent cost-effectiveness ratio.2,3 Although all these technological advances have improved the diagnostic yield of cytohistological samples, insofar as the sampling of adequate material for diagnosis is concerned, the rate of false negatives is as high as 20% in most published series.4,5 Preparation of a cell block with the cytological sample may provide additional morphological information and allow both immunohistochemical and molecular techniques to be performed, thus helping improve histological subtyping and even targeted therapies.6–11 It may also help identify benign diseases that normally need larger specimens for diagnosis.6–10
On this basis, the aim of this study was to analyze the contribution made by cell blocks to conventional cytological smear obtained by EBUS-TBNA in the diagnosis of lymphadenopathies and mediastinal and hilar masses.
MethodologyDesignThis was a retrospective observational study of a prospectively collected series in which the capacity to generate cell blocks from cytological specimens obtained by EBUS-TBNA from hilar and mediastinal lymphadenopathies and/or pulmonary lesions and their additional diagnostic value were analyzed.
PatientsThe pathology reports from the EBUS-TBNA performed in patients with hilar and/or mediastinal lymphadenopathies with a short axis >1cm on CT or 5mm in the case of pathological uptake on PET-CT or with accessible lung lesions, in whom an etiological diagnosis was determined, were reviewed. All procedures were performed consecutively between September 2009 and December 2011 in the Complexo Hospitalario de Vigo, a tertiary level hospital with a referral area of 350000 inhabitants, and 800000 inhabitants specifically for this technique, since neighboring towns with secondary level referral hospitals are also included. EBUS-TBNA was indicated for staging or diagnosis of lung cancer or extrathoracic lesions, and the study of mediastinal or hilar masses/lymphadenopathies of undetermined etiology. Specific informed consent for participation in the study was obtained in writing from all patients. The study was approved by the ethics committee of the region (Research Ethics Committee of Galicia).
EBUS-TBNA and Evaluation of SpecimensAll procedures were performed in an outpatient setting in the conventional bronchoscopy room, with echocardiographic, pressure and pulse oximeter monitoring, under conscious sedation with midazolam and fentanyl. All procedures were performed by a team of 3 pulmonologists, a nurse and a nursing assistant with wide experience in the technique.12 A BF-UC180F-OL8 bronchoscope (Olympus, Japan) and an Aloka Prosound alpha 5 endoscope (Aloka, Japan) were used. After endoscopic examination, the lesion was measured and aspirated using NA2015X-4022 needles (Olympus, Japan). Between 1 and 3 passes through the lymphadenopathy, depending on the immediate results. An expert pathologist was present during all procedures to perform rapid on-site evaluation (ROSE) on all specimens after drying and Diff-Quick staining. Another part of the specimen was fixed in alcohol, and if clots or abundant hematic material or tissue microfragments were obtained, these were fixed with formaldehyde and placed in paraffin to make a cell block. Cytological specimens were systematically stained according to the Papanicolaou method, and histological specimens were stained with hematoxylin and eosin.13 Specimens were considered acceptable when they contained abundant lymphocytes or lymphoid tissue indicative of lymph node, malignant cells or findings suitable for the determination of another specific diagnosis (diagnostic specimens). The specimens were analyzed by the same pathologists who carried out the ROSE. Suspicious and inconclusive specimens were not included, nor were those with a diagnosis of anthracosis. In addition to the etiological diagnoses, sociodemographic variables, type, site and size of the aspirated lesion, the feasibility of preparing cell blocks and their contribution to the morphological diagnosis and their utility for performing immunohistochemical studies were recorded.
Statistical AnalysisOverall results were expressed in percentages and absolute frequencies for qualitative variables and as mean and standard deviation (SD) for quantitative variables. The diagnostic value of the procedures was analyzed with McMemar's exact test, using a two-tailed level of significance of 0.05. The data were analyzed using the Statistical Package for Social Sciences software, version 15.0 (SPSS, Chicago, IL, USA). For the descriptive study, both lymphadenopathy and patient were taken as an analysis unit. For the purposes of the comparative study, each lymphadenopathy was used as an analysis unit.
ResultsA total of 129 EBUS-TBNA specimens from 110 patients, retrieved from various node stations and corresponding masses, were included in the study. Patient characteristics and the aspirated lymphadenopathies and masses (9 pulmonary and one esophageal) are summarized in Table 1. In 81% of the patients, the diagnosis was lung cancer, in 10% extrapulmonary cancer, in 5.4% sarcoidosis, in 2.7% lymphomas and in 0.9% tuberculosis. The most frequently aspirated lesions were 4R (28%) and subcarinal (21%) lymphadenopathies. Lesion diameter on EUS was 15.6mm (SD: 7) and the number of passes through the lymphadenopathy/mass was 2.19 (SD: 0.9). A cell block could be prepared from 72% of the specimens. Cytology was the method for determining diagnosis in 99.1% of cancers and in 75% of benign disease. No relationship was found between the aspirated lymph node and positivity of results. In 52.6% of the cell blocks, immunohistochemical techniques could be performed, contributing to histological typing, compared to 14% of the cytological smears (P<.0001). In 4 patients, the cell block was the only specimen that permitted a morphological diagnosis: benign disease in 3 cases and extrapulmonary metastasis in the other (3 sarcoidosis and one prostate adenocarcinoma metastasis). Diagnosis exclusively from the cell block was significantly more common for benign disease than malignant disease (25% vs 0.9%, lymphadenopathy analysis; P=.002). In 50% of cases of sarcoidosis, diagnosis was obtained from the cell block. In three patients with a diagnosis of malignant disease (1 NOS [non-specific carcinoma], 1 epidermoid carcinoma and 1 adenocarcinoma) with the conventional cytological smear, the cell block provided a diagnosis of the tumor strain. In two cases, the diagnosis was extrapulmonary metastasis (esophageal squamous cell carcinoma and colon adenocarcinoma) and one case it was lung adenocarcinoma (Fig. 1).
Patient Characteristics, Lesions Aspirated and Final Diagnosis.
| Patients | n=110 |
| Age, mean (SD) | 62.5 (10.7) |
| Sex, males | 83 (75.5%) |
| EBUS-TBNA samples | 129 |
| Lymphadenopathies | 119 (92.2%) |
| 4R | 36 (27.9%) |
| 7 | 28 (21.7%) |
| 4L | 11 (8.5%) |
| 10R | 10 (7.7%) |
| 11R | 6 (4.6%) |
| 12R | 2 (1.5%) |
| 2R | 4 (3.1%) |
| 2L | 1 (0.7%) |
| 10L | 2 (1.5%) |
| 11L | 12 (19.3%) |
| 8 | 5 (3.8%) |
| 5 | 1 (0.7%) |
| 3p | 1 (0.7%) |
| Masses | 10 (7.8%) |
| Patient diagnosis | 110 |
| Non-small cell carcinoma | 77 (70%) |
| Small cell carcinoma | 9 (8%) |
| Metastasis | 12 (10.9%) |
| Neuroendocrine carcinoma | 1 (0.9%) |
| NOS | 1 (0.9%) |
| Sarcoidosis | 6 (5.4%) |
| Lymphoma | 3 (2.7%) |
| Tuberculosis | 1 (0.9%) |
NOS: not otherwise specified.
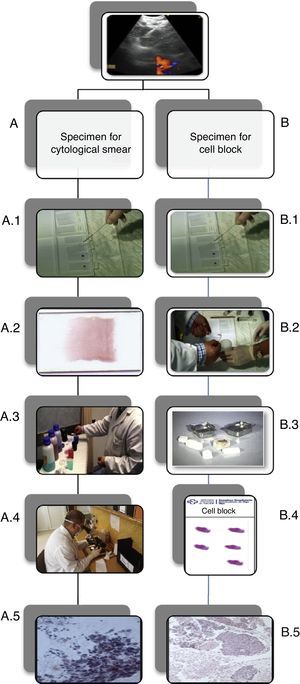
Processing of samples. (A) Cytological smear processing. (A.1) Aspirated material discharged on a slide. (A.2) It is smeared with the aid of another slide and then left to dry. (A.3) Diff-Quick staining. (A.4) Rapid on-site evaluation. (A.5) Example of an epidermoid carcinoma cytology smear. (B) Preparation of the cell block. (B.1) Aspirate material containing bloody remains and tissue microfragments is left to clot. (B.2) The clot is fixed in formol. (B.3) It is then set in paraffin for processing as a biopsy specimen. (B.4) Slide with cell block specimen. (B.5) Microscopic image of an epidermoid carcinoma cell block.
The results of our study show that cell blocks contribute significantly to immunohistochemical techniques, leading to improved cell typing of cancers, and in some cases can also provide exclusive morphological diagnoses, particularly for granulomatous diseases (42.8% of all benign diseases in this study). The improved diagnostic yield of the cell block in benign disease is due to the fact that when the specimen is allowed to clot, the cell material from which morphological features are identified is concentrated, and this may aid the diagnosis of granulomatous diseases and lymphoma.10 The cell block may be prepared from the aspirated material discharged into saline solution or after the material has coagulated. Yung et al.6 compared the diagnostic yield of both techniques and found that the cell block prepared from the clot (the technique used by the authors) significantly increased diagnostic effectiveness, without changing the cytomorphological features of the specimen. The presence of a pathologist minimizes the number of inadequate specimens and can indicate the need for repeat sampling if the preparation of a cell block is required. Recently, Oki et al.14 carried out a comparative study on the contribution of ROSE in a group of 120 patients, showing a reduced need for repetition of procedures and a lower number of passes through the lesion in the EBUS-TBNA+ROSE group. In this series, the cell block contributed exclusively to the diagnosis and/or characterization of the disease in 5.4% (7 of 129) of patients. Several studies have shown the utility of EBUS-TBNA for the diagnosis of mediastinal and hilar lymphadenopathies and masses, particularly in malignant disease, and the greater utility of the cell block in immunohistochemical and even molecular studies.1,13,15–19 Bulman et al.13 found that a histological etiology could be determined from the cell block in 85% of NOS specimens and molecular studies could be performed. Similarly to the findings of the authors, the cell block greatly facilitated immunohistochemical techniques, even if no exclusive morphological diagnosis was determined from this specimen. In other publications in which cytological diagnosis by EBUS-TBNA is compared to other techniques, such as surgery, bronchial biopsy or blind transbronchial aspiration, greater concordance is shown in cases in which a cell block was obtained.15–17 With respect to the usefulness of these specimens in benign disease, there appears to be a general increase in yield,7 although the only entity in which they have been specifically studied is sarcoidosis.19–22 Early studies were performed with aspirations carried out with esophageal ultrasound.20,21 Von Bartheld et al.20 found that in patients with a final diagnosis of sarcoidosis, 33% of the negative cytologies revealed granulomas in the cell block. Iwashita et al.21 also found that diagnoses of sarcoidosis increased from 77.8% to 94.4% when determined with cell block. Schwartz et al.23 were able to diagnose sarcoidosis in 96% of cases exclusively on the basis of the cell block. In this study, the diagnosis could be determined from the cell block in 3 patients with sarcoidosis. With respect to tuberculosis, the specific contribution of EBUS-TBNA to the diagnosis of this disease is not clear.24 Thus, the results of this study coincide with the results previously reported in the cited studies.
This study has a series of limitation that should be mentioned. Firstly, its retrospective nature may allow bias in selection of cases and data. However, this is minimal, since all EBUS-TBNA and the corresponding diagnostic pathological reports made prospectively during the study period were included; the existence of a reliable case source, therefore, adds to the internal validity of the study. Secondly, the study was not blinded, and analyses of the specimens obtained both for standard cytology and for the cell block were performed by the same pathologist; therefore interpretation, particularly of the cytology, could be influenced by the results of the cell block, enhancing its diagnostic value. However, despite this possible advantage for cytology, the study found that the cell block has additional diagnostic value, particularly for benign diseases. Finally, the presence of the pathologist reduces the possible bias of insufficient sampling, since suitability of the specimens was determined by the pathologist during the procedure.
It can be concluded that a cell block can be prepared from a high percentage of cytological specimens from clotted material obtained by EBUS-TBNA. The cell block greatly facilitates immunohistochemical techniques and provides additional data, leading to better diagnostics and improved histological typing of cancers, and has been shown to be useful in the endobronchial diagnosis of node involvement due to benign disease.
Specific Contribution of Each of the AuthorsStudy concept and design: Fernández-Villar, Lourido-Cebreiro.
Patient inclusion: Lourido-Cebreiro, Leiro-Fernández, Núñez-Delgado, Botana-Rial, Fernández-Villar.
EBUS-TBNA performance: Leiro-Fernández, Fernández-Villar, Núñez-Delgado, Botana-Rial, Lourido-Cebreiro.
Pathological analysis: Tardío-Baiges, Álvarez-Martín.
Case review: Lourido-Cebreiro, Leiro-Fernández, Fernández-Villar.
Data analysis and interpretation: Lourido-Cebreiro, Leiro-Fernández, Fernández-Villar, Tardío-Baiges, Álvarez-Martín, Botana-Rial.
Statistical analysis: Lourido-Cebreiro, Fernández-Villar.
Manuscript preparation: Lourido-Cebreiro, Leiro-Fernández, Fernández-Villar.
Critical review of manuscript: Núñez-Delgado, Botana-Rial.
Study supervision: Fernández-Villar.
Conflicts of InterestThe authors declare that they do not have any conflicts of interest.
The specimens used belong to the CHUVI Biobank (RETIC-FIS-ISCIII RD09/0076/00011).
EU Seventh Framework Program (FP7/REGPOT-2012-2013-1; Code: No. 316265, BIOCAPS).
Please cite this article as: Lourido-Cebreiro T, Leiro-Fernández V, Tardio-Baiges A, Botana-Rial M, Núñez-Delgado M, Álvarez-Martín MJ, et al. Aportación del bloque celular en el diagnóstico de adenopatías y masas mediastínicas o hiliares realizado por ecobroncoscopia. Arch Bronconeumol. 2014;50:267–271.