The association between chronic obstructive pulmonary disease (COPD) and anxiety and depression is not yet completely characterized, and differences between countries may exist. We used a predictive model to assess this association in a Spanish population.
Patients and methodProspective transversal descriptive study of 204 patients with stable COPD. Concomitant anxiety or depression was diagnosed by psychiatric assessment, using the diagnostic criteria of the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10). Sociodemographic, clinical and lung function parameters were analyzed.
ResultsIn total, 36% of stable COPD patients had psychiatric comorbidities, but 76% were unaware of their diagnosis. Nineteen percent had a pure anxiety disorder, 9.8% had isolated depression, and 7.3% had a mixed anxiety-depression disorder. Predictive variables in the multivariate analysis were younger age, higher educational level, lack of home support, higher BODE index, and greater number of exacerbations. The ROC curve of the model had an AUC of 0.765 (P<0.001).
ConclusionsIn COPD, concomitant psychiatric disorders are significantly associated with sociodemographic factors. Anxiety disorders are more common than depression. Patients with more severe COPD, according to BODE, younger patients and those with a higher educational level have a greater risk of being diagnosed with anxiety or depression in a structured psychiatric interview. In our population, most patients with psychiatric comorbidities remain unidentified.
La asociación entre la enfermedad pulmonar obstructiva crónica (EPOC) y la ansiedad o la depresión no se conoce adecuadamente, y puede haber diferencias entre distintos países. Investigamos un modelo predictivo para esta asociación en una población española.
Pacientes y métodoEstudio prospectivo descriptivo transversal incluyendo 204 pacientes con EPOC estable. Se diagnostica la presencia de ansiedad o depresión mediante valoración psiquiátrica, aplicando los criterios diagnósticos de la 10.ª revisión del International Statistical Classification of Diseases and Related Health Problems (ICD-10). Se analizan variables sociodemográficas, clínicas y de función pulmonar.
ResultadosUn 36% de pacientes con EPOC estable tienen comorbilidad psiquiátrica, pero en el 76% de los casos se desconocía dicho diagnóstico. Presentan un trastorno de ansiedad pura el 19%, depresión aislada el 9,8% y un trastorno mixto de ansiedad y depresión el 7,3% de los pacientes. En el análisis multivariante las variables predictoras son: edad más joven, mayor nivel de estudios, falta de apoyo domiciliario, mayor índice de BODE y mayor número de agudizaciones. La curva ROC del modelo muestra un AUC de 0,765 (p<0,001).
ConclusionesEn la EPOC, una mayoría de pacientes con comorbilidad psiquiátrica no son identificados. Los trastornos de ansiedad son más frecuentes que la depresión, en base a un diagnóstico mediante entrevista estructurada. Los pacientes más jóvenes y con mayor nivel de estudios tienen más riesgo de de padecer ansiedad o depresión. Otros factores predictivos son: un mayor índice BODE, más agudizaciones y la falta de apoyo domiciliario.
Clinical guidelines for chronic obstructive pulmonary disease (COPD) point to depression and anxiety as key comorbidities.1,2 These conditions, associated with higher mortality and more frequent and longer hospital stays for exacerbations,3 are a main determinant of the quality of life of patients with COPD.4
Although current guidelines recommended that patients with COPD undergo specific psychosocial assessment,1,2,5 anxiety and depression frequently go undiagnosed and untreated.3,6 A review article published as recently as 20143 discussed the methodological limitations affecting scientific studies of this association, pointing, among other factors, to the failure to obtain an accurate diagnosis of anxiety or depression and the absence of anxiety or depression as primary endpoints. Furthermore, both prevalence of COPD-related anxiety and depression and patient characteristics differ according to geographical region.7,8 Better designed studies are clearly needed to pinpoint the relationship between COPD and psychiatric comorbidities.9
According to the PubMed database, 6 articles have been published in the last 10years referring to anxiety and depression in patients with COPD in Spain: 4 confirmed the existence of psychiatric comorbidities on the basis of different symptom-related questionnaires10–13; and the other 2 were population studies where COPD, anxiety and depression diagnoses were established based on medical records and patient surveys.14,15 Just 4 of these studies referred to stable patients and just 1 was specifically designed to explore depression in patients with COPD.13
Our aim was to investigate the presence of anxiety or depression in a sample of Spanish patients with stable COPD in order to developing a predictive model of the association between COPD and these comorbidities.
MethodsStudy DesignProspective descriptive transversal study that included patients consecutively diagnosed with stable COPD in the outpatient pulmonology clinic of a tertiary hospital in Granada (Spain) between June 2012 and November 2013.
Sample SelectionInclusion criteria: (a) a post-bronchodilation forced expiratory volume in the first second (FEV1) to forced vital capacity (FVC) ratio of <0.7; (b) a history of smoking of 20 or more pack-years or other exposure related to the pathogenesis of COPD; and (c) clinical stability, defined as not having required any change to usual COPD treatment in the previous 3months.
Exclusion criteria: (a) advanced comorbidity or decompensated comorbidity; (b) a diagnosis of asthma or other different from COPD; (c) physical limitations in performing basic activities of daily living; (d) no informed consent; and (e) an inability to properly complete the study questionnaire.
Sample size was calculated on the basis of an estimated depression prevalence of 17%,16–18 given that depression was the most widely documented psychological comorbidity in the literature. A sample size of 215 patients was needed for a precision of 5% and an asymptotically normal two-sided 95% confidence interval (CI).
Study VariablesSociodemographic and clinical variables. Patient sociodemographic and clinical data were collected through interviews and from medical histories.
Anxiety and depression assessment. The patients were screened using the Hospital Anxiety and Depression Scale (HADS),19 designed for use in medically ill patients with somatic symptoms that may mimic psychological symptoms. HADS—which has been validated in both the general population20 and in patients with COPD21,22—is a self-administered 14-item questionnaire, divided into 2 subscales of 7 items each for anxiety and for depression. Anxiety items were selected from the Hamilton Anxiety Scale so as to avoid questions that could lead to confusion regarding symptoms of physical illness. Depression items focus on anhedonia (loss of pleasure), thereby avoiding questions reflecting energy loss. The questionnaire refers to the previous week, and symptom intensity or frequency are evaluated on a scale of 0–3. Patients who scored 8 or more on either subscale or who scored 12 or more in total were evaluated by a psychiatrist. The initial suspicion was confirmed or ruled out in this psychiatric interview—structured according to criteria described in the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10)23—after checking that the patient had not experienced COPD exacerbations or any other comorbidity. Patients with a previous psychiatric diagnosis of anxiety or depression were considered as confirmed cases and so were excluded from further psychiatric evaluation.
Respiratory function assessment. Spirometry values (FEV1, FVC and FEV1/FVC) were measured in the 3 months prior to enrolment. Values considered were those measured after bronchodilation with 4 puffs of 100μg of salbutamol, as recommended by the Global Initiative for Chronic Obstructive Lung Disease (GOLD).2 Anthropometric data were collected during the spirometry sessions. All patients performed the 6-minute walk test (T6MM). Examinations were performed according to Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) protocols.24 Dyspnea was assessed using the modified Medical Research Council (mMRC) scale.
Statistical AnalysisAbsolute and relative frequencies were calculated for qualitative variables and means and standard deviations were calculated for quantitative variables. Hypotheses were tested using the Chi-square or Fisher test for qualitative variables and the Student t test or one-way analysis of variance (ANOVA) for quantitative variables. The Wald forward stepwise selection method was used for multivariate analysis of all variables associated with the presence of anxiety or depression according to the bivariate analysis. Scores for the BODE index (reflecting body mass index, airflow obstruction, dyspnea and exercise capacity) and for its individual components were analyzed. The predictive capacity of the models was evaluated by calculating the receiver operating characteristic (ROC) curve and the area under the curve (AUC). The level of significance for all tests was set to P<.05. Analyses were performed using IBM SPSS Statistics 20 software.
The study was approved by the Ethics Committee of the Hospital Virgen de las Nieves de Granada (Spain).
ResultsA total of 204 patients were included, 18 (9%) of whom had a previous psychiatric diagnosis of anxiety or depression. Patient characteristics are summarized in Table 1.
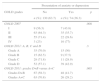
Patient Demographics and Clinical Characteristics (n=204).
| Sex, n (%) | |
| Men | 184 (90.2) |
| Women | 20 (9.8) |
| Age, mean±SD | 66.2±9.5 |
| BMI, mean±SD | 27.6±4.4 |
| Occupational status, n (%) | |
| Active | 55 (27.0) |
| Retired | 149 (73.0) |
| Marital status, n (%) | |
| Separated/divorced | 16 (7.8) |
| Married | 153 (75) |
| Widow(er) | 19 (9.3) |
| Single | 16 (7.8) |
| Home support, n (%) | |
| Yes | 195 (95.6) |
| No | 9 (4.4) |
| Limitations on activities of daily living, n (%) | |
| None | 170 (83.3) |
| Some | 34 (16.7) |
| Current smoker, n (%) | 53 (26.0) |
| Comorbidity drugs, median (minimum-maximum) | 2 (0–14) |
| Charlson comorbidity index, median (minimum-maximum) | 1 (0–5) |
| T6MM distance <350m, n (%) | 32 (15.7) |
| Dyspnoea (mMRC), n (%) | |
| 0–1 | 91 (44.5) |
| 2–3 | 113 (55.4) |
| Exacerbations, n (%) | |
| 0–1 | 120 (58.8) |
| ≥2 | 84 (41.2) |
| Admission in the previous year, n (%) | 30 (14.7) |
| Smoking in pack-years, mean±SD | 56.3 (21.7) |
| FVC (mL), mean±SD | 2930 (794) |
| FVC (%), mean±SD | 78.7 (18.7) |
| FEV1(mL), mean±SD | 1591 (578) |
| FEV1%, mean±SD | 54.2 (17.1) |
| FEV1/FVC%, mean±SD | 53.8 (9.7) |
| T6MM distance in metres, mean±SD | 462.1 (98.3) |
Abbreviations: BMI, body mass index; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; mMRC, modified Medical Research Council scale (dyspnoea); SD, standard deviation; T6MM, 6minute walk test.
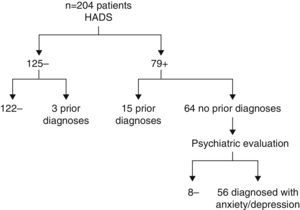
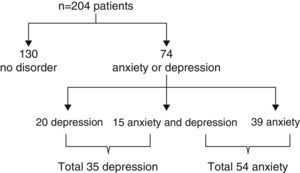
Mean HADS scores were 10.98±7.19 overall, 6.26±4.08 for the anxiety subscale and 4.77±3.59 for the depression subscale. The HADS pointed to significant symptoms of anxiety or depression in 79 patients (39%). Of these 79 patients, 15 had been diagnosed prior to inclusion in the study and so were considered confirmed cases; the remaining 64 patients underwent psychiatric evaluation and a diagnosis of depression or anxiety was confirmed in 56 cases. In total, therefore, 74 study patients (36%) had anxiety or depression confirmed by psychiatric diagnosis (Fig. 1) and a fifth of these had a mixed anxiety-depression disorder. Of the total sample of 204 patients, 19% had pure anxiety and 9.8% had pure depression (Fig. 2).
According to the bivariate analysis (Table 2), patients with anxiety and depression had a higher educational level, lacked home support, were younger and occupationally active and were single, separated or divorced. They had also experienced more exacerbations in the previous year, had higher baseline dyspnoea, covered less distance in the T6MM and scored higher on the BODE index. To a statistically significant degree, anxiety and depression were more frequent in patients treated with 7 or more drugs and in patients with more limited autonomy. The presence of more than 4 comorbidities associated with COPD was not statistically significant (P=.08), nor were statistically significant differences found regarding sex, smoking, alcoholism, presence of cardiovascular comorbidities, FEV1, FVC, FEV1/FVC, hospital admissions for exacerbations or use of home oxygen therapy. A higher proportion of patients with stage I and stage IV airflow obstruction according to the GOLD classification2 presented anxiety and depression (P<.009). Anxiety and depression were also more prevalent in the more symptomatic patients versus the less symptomatic patients (groups D and B versus groups A and C, respectively; P=.065) (Table 3).
Bivariate Analysis. Variables Associated With the Presence of Anxiety or Depression in Patients With COPD (n=204).
| Presentation of anxiety or depression | |||
|---|---|---|---|
| No | Yes | p ≤ | |
| n (%): 130 (63.7) | n (%): 74 (36.3) | ||
| Sex | .179 | ||
| Men | 120 (65.2) | 64 (34.8) | |
| Women | 10 (50.0) | 10 (50.0) | |
| Age | .001 | ||
| ≥65 years | 87 (73.7) | 31 (26.3) | |
| <65 years | 43 (50.0) | 43 (50.0) | |
| Occupational status | .001 | ||
| Retired | 105 (70.5) | 44 (29.5) | |
| Active | 25 (45.5) | 30 (54.5) | |
| Education | .008 | ||
| No/primary | 106 (68.8) | 48 (31.2) | |
| Secondary/tertiary | 24 (48.0) | 26 (52.0) | |
| Marital status | .003 | ||
| Married/widow(er) | 117 (68.0) | 55 (32.0) | |
| Single/separated | 13 (40.6) | 19 (59.4) | |
| Home support | .01 | ||
| Yes | 128 (65.6) | 67 (34.4) | |
| No | 2 (22.2) | 7 (77.8) | |
| Personal autonomy | .03 | ||
| Fully autonomous | 114 (67.1) | 56 (32.9) | |
| Some limitations | 16 (47.1) | 18 (52.9) | |
| Comorbidity drugs (n) | .03 | ||
| <7 | 126 (65.6) | 66 (34.4) | |
| ≥7 | 4 (33.3) | 8 (66.7) | |
| Dyspnoea (mMRC) | .01 | ||
| 0 | 11 (78.6) | 3 (21.4) | |
| 1 | 53 (68.8) | 24 (31.2) | |
| 2 | 52 (66.7) | 26 (33.3) | |
| 3 | 14 (40.0) | 21 (60.0) | |
| Exacerbations (n) | .01 | ||
| 0–1 | 85 (70.8) | 35 (29.2) | |
| ≥2 | 45 (53.6) | 39 (46.4) | |
| T6MM (metres) | .03 | ||
| ≥350m | 115 (66.9) | 57 (33.1) | |
| <350m | 15 (46.9) | 17 (53.1) | |
| BODE | .004 | ||
| <4 | 109 (69.0) | 49 (31.0) | |
| ≥4 | 21 (45.7) | 25 (54.3) | |
Abbreviations: BODE (index), body mass index, airflow obstruction, dyspnoea, exercise capacity; COPD, chronic obstructive pulmonary disease; mMRC, modified Medical Research Council scale (dyspnoea); T6MM, 6minute walk test.
Bivariate Analysis. Anxiety or Depression According to GOLD Severity Grades for COPD (n=204).
| Presentation of anxiety or depression | |||
|---|---|---|---|
| GOLD grades | No | Yes | p |
| n (%): 130 (63.7) | n (%): 74 (36.3) | ||
| GOLD 2007 | .008 | ||
| I | 9 (56.3) | 7 (43.8) | |
| II | 63 (64.3) | 35 (35.7) | |
| III | 55 (71.4) | 22 (28.6) | |
| IV | 3 (23) | 10 (77) | |
| GOLD 2011: A, B, C and D | .3 | ||
| Grade A | 35 (70.0) | 15 (30) | |
| Grade B | 15 (62.5) | 9 (37.5) | |
| Grade C | 28 (71.8) | 11 (28.9) | |
| Grade D | 52 (57.1) | 39 (42.9) | |
| GOLD 2011: grades D+B versus A+C | .065 | ||
| Grades D+B | 67 (58.3) | 48 (41.7) | |
| Grades A+C | 63 (70.8) | 26 (29.2) | |
Abbreviations: COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
For the multivariate analysis, which included all significant variables from the bivariate analysis, an equation each was calculated for the overall BODE index score and for that of individual BODE index parameters (Table 4). Of the 2 resulting models, the overall BODE index offered a better ROC curve value, for an AUC of 0.765 (P<.001), contrasting with an AUC of 0.753 (P<.001) for the individual BODE index parameters. Of those parameters, only a higher level of dyspnea was a risk factor. The logistic regression model for the BODE index had specificity and sensitivity values of 90% and 54%, respectively.
Multivariate Analysis. Predictors of Anxiety or Depression in Patients With COPD.
| BODE model | p | OR | 95% CI for OR | |
|---|---|---|---|---|
| Age | ≤.001 | .93 | .89 | .96 |
| Secondary/tertiary education | ≤.005 | 2.83 | 1.33 | 6.00 |
| Lack of home support | ≤.049 | 6.04 | 1.20 | 35.70 |
| Exacerbations ≥2 | ≤.029 | 2.15 | 1.11 | 4.23 |
| BODE ≥4 | ≤.001 | 3.98 | 1.79 | 8.91 |
| BODE components model | p | OR | 95% CI for OR | |
|---|---|---|---|---|
| Age | <.001 | .93 | .90 | .97 |
| Secondary/tertiary education | ≤.012 | 2.58 | 1.28 | 5.41 |
| Lack of home support | ≤.037 | 6.45 | 1.12 | 37.09 |
| Exacerbations ≥2 | ≤.029 | 2.12 | 1.08 | 4.01 |
| Dyspnoea ≥3 mMRC | ≤.001 | 4.45 | 1.85 | 10.71 |
Abbreviations: BODE (index), body mass index, airflow obstruction, dyspnoea, exercise capacity; CI, confidence interval; COPD, chronic obstructive pulmonary disease; mMRC, modified Medical Research Council scale (dyspnoea); OR, odds ratio.
Age in the two models was highly significant (P<.001), for an estimated odds ratio of 0.93. Also significant in both models were frequent exacerbations, a higher education level and lack of home support.
DiscussionWe investigated a sample of 204 Spanish patients with COPD for anxiety or depression. Our sample reflected the profile of patients typically seen in a Spanish pulmonology clinic and, except for the high smoking rate, also reflected the characteristics of the INSEPOC Spanish multicentre population study.14,25 We estimated prevalence of anxiety and depression in patients with COPD, confirmed by psychiatric diagnosis, to be between 30% and 43% (95% CI). Depression was detected in 17% (95% CI: 12%–22%) and anxiety in 26.5% (95% CI: 21%–33%) of the patients in our study. Of the patients with psychiatric comorbidities, 20% (15/74 patients) had a mixed anxiety-depression disorder.
A recent literature review of anxiety in COPD identified studies designed on the basis of structured psychiatric interviews and established diagnostic criteria (ICD-10; Diagnostic and Statistical Manual of Mental Disorders (DSM III and DSM IV)).26 Only 3 of those studies17,18,27—with confirmed COPD diagnoses—explored both anxiety and depression in sufficiently large samples (137, 116 and 143 subjects).
In contrast with our finding of a 36% prevalence rate, Kühl et al.,17 reported an overall prevalence of 25%; this lower percentage could be due, as the authors themselves concede, to the fact that the number of patients with generalized anxiety disorder was probably underreported, given that anxiety secondary to the disease itself was not taken into account. Yohannes et al.27 and Laurin et al.18 reported prevalence rates of 47% and 49%, respectively. The fact that these 2 studies included approximately 50% of women might explain their higher prevalence rates; indeed, when stratified by sex, Laurin et al.18 reported a 38% rate of anxiety or depression in men—a rate comparable to that reported in our study.
We found anxiety to be more frequent than depression in our patients, corroborating the findings of Laurin et al.18 Yohannes et al.,27 in contrast, found depression to be more frequent, although this could be attributable to the significant degree of disability in their patients. In fact, disability was the factor most strongly associated with depression according to their own conclusions. In Kühl et al.,17 depression and anxiety were found in roughly equal proportions, although as already mentioned, anxiety was probably underdiagnosed. Overall, the findings of the above studies tend to reinforce the cogency of our own results.
As for the Spanish population, a recent article by Miravitlles et al.13 reported that 74.6% of patients with stable COPD treated at outpatient clinics in Spain had depression as assessed using the Beck Depression Inventory. We would suggest that this questionnaire with its conventional cutoff points is possibly overestimating the presence of depression in patients with stable COPD.
Our risk model points to relative youth, higher education level, higher BODE index score, greater dyspnea, an exacerbator phenotype and lack of home support as predictors of anxiety and depression in patients with stable COPD.
In previous studies based on certain diagnoses, some of which did not specifically analyze age, no association was found with age. In our study, the association may be due to the fact that our sample had more patients aged under 65years. Yohannes et al.,27 in contrast, specifically included subjects aged over 60years (mean age, 73years).
While a higher level of education was a risk factor for developing anxiety or depression in our sample, the few other studies that considered this variable have reported contradictory findings. Chazelle et al.28 found that level of education was associated with income level, which, in turn, was associated with access to, or lack of, private medical insurance. This suggests that access to healthcare may modify the link between educational level and anxiety or depression and so should be taken into account in comparing populations located in different countries. Evidence that a higher educational level is a risk factor for developing anxiety and depression in both the general population29 and in patients with COPD,30 as reported in recent studies in Ontario, echo our own findings within the context of a similar healthcare system.
Our study did not find occupational status to be a predictive factor, although our sample admittedly had only 4 unemployed patients. The higher frequency of anxiety and depression found in occupationally active patients could be due to the younger age of these patients.
Regarding COPD clinical variables, other studies have championed the BODE index score as a predictor of risk.31,32 Our analysis shows that the overall BODE score was more relevant than the scores for individual parameters, for an odds ratio of 3.98 (P<.001) for patients with BODE score ≥4. Of the BODE parameters, only dyspnea was significant in the multivariate analysis. As for FEV1, although we found a significant association when patients were stratified according to the GOLD 2007 classification, this significance was not maintained in the multivariate analysis. A higher proportion of stage I and stage IV patients presented anxiety and depression. The lower age of stage I patients and the higher levels of dyspnoea in stage IV patients may have acted as confounders. Our study confirms the absence of any link between FEV1 and psychiatric comorbidities31,32; it should be noted, however, that the COPD Strategy of the Spanish National Healthcare Plan only provides for psychiatric assessment in patients with poor lung function.33
Our sample included few women (20/204 patients), in line with other similar studies in Spain.14,25 This would explain why no significant difference was found in our study between men and women, in contrast with findings of higher female prevalence reported for other studies.8,34,35 Few of the patients in our study were admitted for hospitalization during the previous year (30/204), and that could influence that hospital admission was not associated with anxiety or depression. We found that not having home support was more important than loss of autonomy, although this conclusion cannot be taken for granted for patients with greater physical limitations. For our population of patients with stable COPD monitored in a pulmonology clinic, neither the number of drugs prescribed nor the number of comorbidities were predictors, although these 2 variables could be relevant in populations with greater comorbidity rates.
Finally, for logistical reasons, the fact that patients who scored below the HADS cutoff point were not assessed by a psychiatrist may have underestimated the prevalence of anxiety and depression in our sample. To overcome this limitation, we sought greater sensitivity by considering total HADS scores as well as HADS subscale scores, given that some authors have reported total scores to be more useful for screening purposes.36,37
ConclusionsOur study included 204 patients with stable COPD and established a prospective psychiatric diagnosis of anxiety or depression using ICD-10 criteria. We found 36% of our study subjects to have anxiety and/or depression. Since only 9% were diagnosed before inclusion in the study, underdiagnosis of these comorbidities in our setting would appear to be very high. Anxiety was more common than depression, and the two conditions coincided in a significant proportion of our patients. Our results indicate that younger patients with higher education levels have an increased risk of developing anxiety and depression. Other risk factors were higher BODE index scores, more exacerbations and lack of home support. Of the individual BODE components, only dyspnoea was an independent predictor. Future studies should take into account access to healthcare resources in comparing samples from different countries.
FundingResearch grant from the Neumosur Foundation.
Conflict of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-Gutiérrez MV, Guerrero Velázquez J, Morales García C, Casas Maldonado F, Gómez Jiménez FJ, González Vargas F. Modelo predictivo de ansiedad y depresión en pacientes españoles con enfermedad pulmonar obstructiva crónica estable. Arch Bronconeumol. 2016;52:151–157.