Primary amyloidosis is a rare disease caused by deposits of amyloid fibrils formed by insoluble protein in different tissue types.1 No genetic or environmental factors that might make an individual more susceptible to amyloid deposits have been identified.2
Primary pulmonary amyloidosis, when deposits are limited to the lungs and associated structures with no involvement of other organs, is a very rare manifestation of the disease.2–4
Amyloid nodules in pulmonary parenchyma are usually an incidental finding that must be distinguished from other diseases.4,5 Pulmonary amyloid nodules with uptake on positron emission tomography (PET) are very rare. To date, only 7 cases have been published in the English literature.1
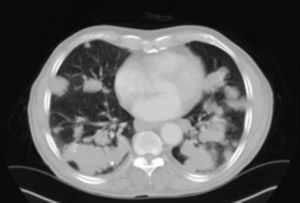
An 80-year-old man, a former smoker, presented with a few months’ history of dyspnea and systemic signs (asthenia, anorexia and loss of weight). Physical examination and laboratory tests results did not reveal any significant changes. Chest X-ray showed multiple disperse nodular lesions in both lung fields. Chest and abdominal computed tomography (CT) found disperse nodular pulmonary lesions with lobulated borders and no calcifications, in both lungs (Fig. 1). No microorganisms or malignant cells were identified in bronchoscopy specimens. PET-CT results suggested that some of the lesions in both lungs had significantly higher affinity for FDG than others, and there were no lesions with increased uptake in any other part of the body. Lung function tests showed moderate airway obstruction. Transthoracic and transbronchial biopsies showed amorphous amyloid-type cells. Two years after diagnosis, the patient remains in good clinical condition under treatment with inhaled long-acting beta-antagonist bronchodilator and corticosteroid.
Primary pulmonary amyloidosis occurs in 4 forms: tracheobronchial amyloidosis, nodular pulmonary amyloidosis, infiltrating interstitial amyloidosis and amyloidosis of the lymph nodes. The anatomical and functional evaluation of respiratory tract amyloidosis should be evaluated using standard X-ray, CT, endoscopy and lung function testing.5
From a radiological point of view, primary nodular parenchymal pulmonary amyloidosis occurs in the form of single or multiple nodules in any lobe, and must be taken into account in the differential diagnosis of primary or metastatic pulmonary malignancies, pulmonary tuberculosis, pulmonary sarcoidosis, and connective tissue diseases.2 Nodules are generally peripheral and subpleural and 4 typical features are observed on CT: well-defined lobulated borders, calcification that is often central or forms in an irregular pattern within the nodule, multiple shapes and sizes, and slow growth, often over years, with no remission.3
F-FDG PET-CT is widely used in the detection of cancer.2 As with other diagnostic procedures, some results may be false positives, and some non-malignant diseases, such as tuberculosis, sarcoidosis, fungal disease, interstitial lung disease, arthrosis, vascular thrombosis, osteoporosis and rheumatoid nodules, can show increased metabolic activity.1,2 In our case, multiple pulmonary amyloidosis nodules with moderate F-FDG uptake were observed, an observation also reported by Khan et al.1 and Zhang et al.2
Pathological examination of a tissue sample is the standard reference for diagnosing amyloidosis.
On optical microscopy, hematoxylin and eosin staining shows homogeneous, pinkish, amyloid substances with no cell structure, often associated with typical fibrosis, and a red-green birefringence on polarized light microscopy of Congo-red stained tissue.4 Information on prognosis and treatment of amyloid in the lung is taken from testimonial reports. To date, no fully effective treatment is available.4 Nodular disease may progress slowly, with lesions increasing in size and number.1 Some patients have an excellent prognosis,4 while in others, disease progresses until death from respiratory failure.1
Although primary pulmonary amyloidosis is a very rare disorder, a definitive diagnosis may mean that the patient can be correctly monitored and unnecessary interventions and treatments can be avoided.
Please cite this article as: Pacheco C, Cruz J, Ferreira L. Tomografía por emisión de positrones/tomografía computarizada positiva y nódulos pulmonares múltiples: un diagnóstico poco habitual. Arch Bronconeumol. 2015;51:48–49.