We report the case of a young asymptomatic patient with a chest mass that was finally diagnosed as an intrafissural primitive neuroectodermal tumor (PNET). A pulmonary mass was detected in this 27-year-old woman on an unrelated chest X-ray. All laboratory test results were normal. Computed tomography (CT) revealed an elliptic, heterogeneous mass with contrast uptake in the left hemothorax, about 12cm in diameter with smooth borders, located within the oblique fissure of the left pleura (Fig. 1). CT-guided fine-needle aspiration biopsy cytology was inconclusive. Surgical resection revealed an intrafissural mass. Hematoxylin and eosin staining produced a surprisingly uniform pattern of solidly compacted round cells.
Immunohistochemical assays showed tumor cells that were strongly positive for MIC2 (CD99) and for vimentin, but negative for other markers, such as cytokeratin (CK), small cell lung cancer, chromogranin, CK7, CK19 and thyroid transcription factor-1. Molecular genetic studies using fluorescence in situ hybridization showed positive translocation of the long arms of chromosomes 11 and 22 [t(11;22)(q24;q12)]. These results were suggestive of PNET. No distant metastases were found using standard staging methods, including brain magnetic resonance imaging (MRI), whole body MRI, abdominal CT and bone scintigraphy. After complete surgical resection, the patient received chemotherapy. Since then, she has been monitored in the outpatient clinic and her situation remains unchanged after 2 years.
Chest PNETs, also known as Askin's tumors, probably originate in the embryonic neural crest cells. They consist of small round cells with neural differentiation, and are associated with translocation of chromosome 22.1,2 They typically appear in the soft tissues of the chest. A primary tumor located inside the lung is very rare, but pleural involvement is common.3 Patients are generally children or young adults, although PNET can develop at any age. It usually presents with pain in the chest wall, and can be associated with pleural effusion and dyspnea.4
The most common CT finding in PNET is a mass with heterogeneous contrast uptake. Occasionally, a central area of low density with no contrast uptake seen inside the mass. The heterogeneous aspect of these large tumors is usually due to focal areas of bleeding or necrosis.5
Diagnosis of PNET is made using various techniques, such as optical microscopy, histological findings of small round cells arranged in a lobular pattern with rosettes or pseudorosettes, and by immunohistochemical and ultrastructural signs of neural differentiation. Reciprocal translocation of the long arms of chromosomes 11 and 22 [t(11;22)(q24;q12)] is currently thought to be characteristic of this tumor family.1 Although there are no standard treatment guidelines, neoadjuvant chemotherapy and surgical resection, with or without local radiation therapy, followed by adjuvant chemotherapy appears to be the best option.2 In conclusion, although primary fissural PNET is an extremely rare soft tissue sarcoma, this possibility must be taken into consideration in the differential diagnosis of a primary fissural mass.
Please cite this article as: Hochhegger B, Felicetti JC, Marchiori E. Una masa intracisural infrecuente: tumor neuroectodérmico primitivo pleural. Arch Bronconeumol. 2015;51:47–48.


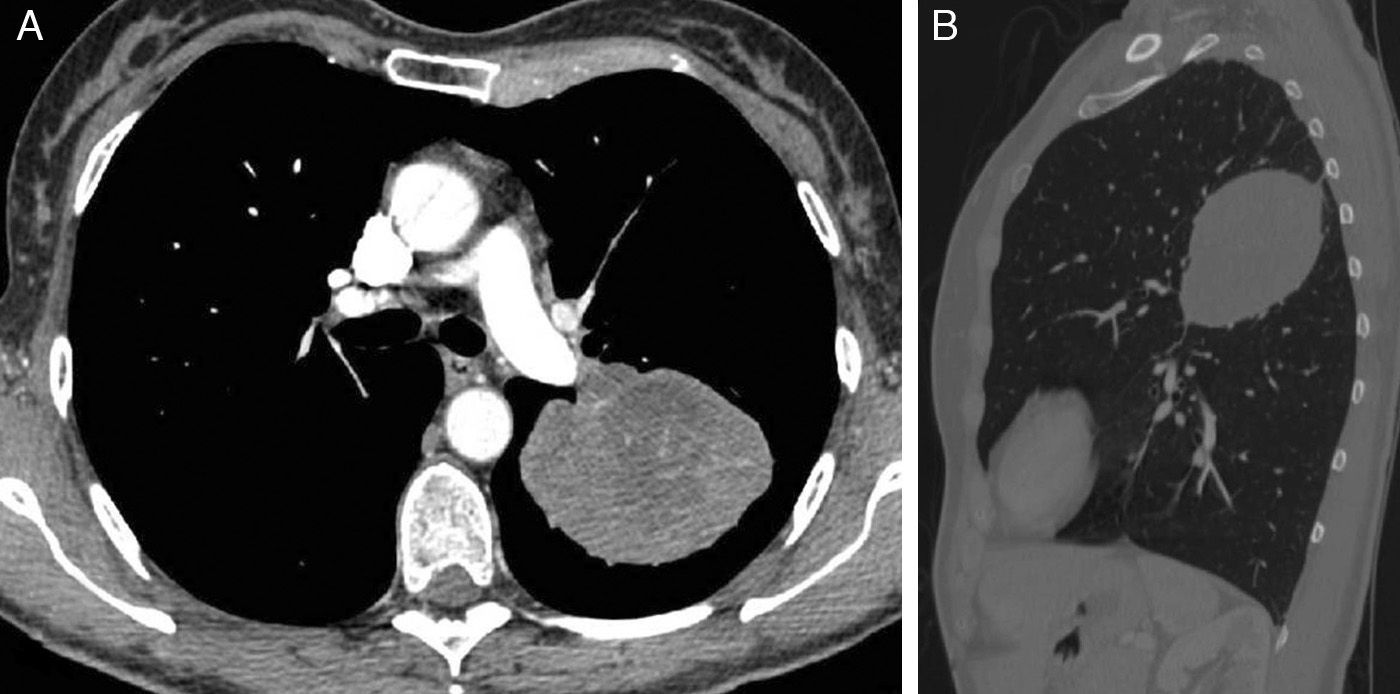
![Chest computed tomography images [axial (A) and sagittal (B)] showing a heterogeneous elliptic tumor with contrast uptake in the oblique fissure of the left hemothorax. Chest computed tomography images [axial (A) and sagittal (B)] showing a heterogeneous elliptic tumor with contrast uptake in the oblique fissure of the left hemothorax.](https://static.elsevier.es/multimedia/15792129/0000005100000001/v1_201412231236/S1579212914003450/v1_201412231236/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)








