Diagnosing recurrent tracheoesophageal fistula (TEF) in a child with congenital esophageal atresia repair during the neonatal period who has recurrent or persistent respiratory symptoms is a real challenge, since medium leakage in the gastrointestinal tract may be missed on standard contrast studies.1,2 We present a case that illustrates the importance of high-pressure administration of contrast medium in the esophagus via a catheter, for visualization of recurrent TEF, and the additional utility of flexible bronchoscopy for diagnosis.
A 3 ½-year-old boy was evaluated for recurrent lower respiratory tract infections. He had a history of congenital esophageal atresia with distal TEF repair in the neonatal period. At the age of 2 ½ years, the child was hospitalized for complicated pneumonia with pneumothorax and pneumomediastinum, requiring admission to the intensive care unit and chest tube placement. Chest CT showed diffuse ground glass opacities and areas of atelectasis in both lungs. In view of the seriousness of the clinical signs, recurrent TEP was considered in the differential diagnosis. The patient had a history of anastomotic leakage, a known risk factor for fistula recurrence,3 yet there were no signs of contrast medium leak or esophageal stenosis in the gastroduodenal tract.
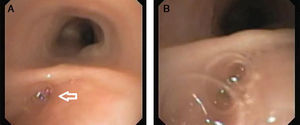
Nonetheless, the patient was admitted on 4 occasions in the following year for fever, cough and shortness of breath. Evaluation by a pediatric pulmonologist was requested by the attending physician. Chest auscultation revealed crepitations and wheezing. Chest X-rays showed areas of atelectasis in both lungs and mild gastroesophageal reflux was detected on pH-metry. The most important finding on flexible bronchoscopy was a pouch in the posterior tracheal wall, with air bubbling during bag valve mask ventilation administered by the anesthesiologist, suggesting a communication between the esophagus and the pouch (Fig. 1 and Supplementary video 1). Lipid-laden macrophages were found in bronchoalveolar lavage (BAL) fluid and Pseudomonas aeruginosa was isolated from BAL culture. Both of these data suggest chronic aspiration and lower respiratory tract infection. Since no diagnostic procedures had been performed in the gastroduodenal tract, contrast medium was injected via a catheter into the esophagus, confirming concurrent TEF (Fig. 1 and Supplementary video 2).2
Approximately 50% of children with history of esophageal atresia and TEF repair have recurrent or persistent respiratory symptoms due to bronchial hyperreactivity, tracheomalacia or aspiration due to esophageal dyskinesia, esophageal stenosis, gastroesophageal reflux or relapse of repaired TEF (in up to 10% of cases of esophageal atresia).3–5 Recurrence of the fistula in the gastrointestinal tract may be difficult to identify, so injection of contrast medium in the esophagus is the next diagnostic step.2 Under cinefluoroscopic guidance and with the patient prone, contrast medium is injected under pressure via a nasogastric tube placed in the stomach that is slowly withdrawn to the esophagus.
The identification of lipid-laden macrophages in the cytological examination of BAL fluid obtained by flexible bronchoscopy is a sign that aspiration may have occurred. Intubation of the fistula with the bronchoscope or injection of methylene blue with esophagoscopy are additional methods that can provide important information for the diagnosis of recurrent TEF.2
Conflict of InterestNone of the authors has any conflict of interests to declare.
The following are the supplementary data to this article:
After administration of inhaled anesthetic via the bag valve mask and intravenous propofol, a flexible video-assisted bronchoscope was inserted via the right nostril, pharynx, glottis and trachea. Mild tracheomalacia was observed. A tracheal pouch was identified in the posterior tracheal wall, near the carina. Air bubbling was seen in the pouch during with bag valve mask ventilation performed by the anesthesiologist, suggesting a communication between the esophagus and the trachea.
Under cinefluoroscopic guidance and with the patient prone, contrast medium was injected under pressure via a slowly withdrawn nasogastric tube. The black column corresponds to contrast medium inside the esophagus. Contrast medium leak can be seen in the right side of the esophagus in the form of a pale gray U-shaped loop, suggestive of the presence of a tracheoesophageal fistula (TEF).
Please cite this article as: Platnaris A, Lianou D, Kaditis AG. Fístula traqueoesofágica recurrente en niños con atresia esofágica reparada y utilidad de la broncoscopia flexible. Arch Bronconeumol. 2015;51:49–50.