We report the case of an 80 year-old woman who had had dry cough and wheeze for many years, presenting with increased symptoms associated with recent development of generalized weakness and weight loss. She had had several episodes of pneumonia. Previous bronchoscopy and bronchoalveolar lavage (BAL) 13 years ago was negative for acid-fast bacilli (AFB) but identified Curschmann's spirals. Recent chest CT showed progression of consolidation in the right upper, middle and lower lobes with bilateral bronchiectasis and centrilobular micronodules in a tree-in-bud configuration. Bronchoscopy was performed for further evaluation.
Shortly after the procedure, she reported acute right-sided back pain, which responded to acetaminophen. Examination was unchanged, and chest radiography performed 3h later did not show pneumothorax. As her pain had resolved, she was discharged home. During subsequent days, she reported fever (101–105°F) and intermittent back and right upper quadrant pain with no dyspnea or change in cough. She was evaluated in the clinic on the fifth day after the procedure. Chest CT showed an extensive right lower and middle lobe consolidation with hydropneumothorax (Fig. 1, upper panel).
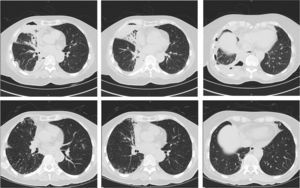
Upper panel: computed tomography (CT) images of the chest obtained at the time of presentation with pneumothorax and pleural effusion. Consolidation is shown in the right middle lobe (first and second panel), and air-fluid levels are shown in the right pleural space (third panel). Tree-in-bud opacification is shown in both lungs. Lower panel: CT images obtained 3 months following commencement of treatment for NTM disease. There is resolution of the right sided pleural effusion and pneumothorax, with re-expansion of the lung and improvement in consolidation of the right middle lobe.
By this time, BAL smear and cultures were positive for AFB. Thoracentesis was performed, confirming an exudative pleural effusion that was lymphocyte-predominant (82% lymphocytes), and cultured no organisms. She commenced recommended treatment for non-tuberculous mycobacterium (NTM),1 and also treatment for presumed health-care associated pneumonia. The hydro-pneumothorax was managed without need for insertion of a pleural catheter or surgical intervention.
A diagnosis of M. avium complex was later confirmed from BAL fluid. She tolerated the NTM regimen well, reporting decreased symptoms of fever and back pain. Subsequent chest CT imaging following 3 months of treatment for NTM showed resolution of the pleural effusion and pneumothorax, and improvement in tree-in-bud appearances (Fig. 1, lower panel).
NTM disease may be associated with spontaneous pneumothorax with an incidence of 2.4%–4.1%.2 Mortality due to pneumothorax in such patients may be as high as 66%, compared to 8% in those without pneumothorax.2 Conversely, the overall risk of pneumothorax during BAL fluid collection is extremely low.3 In a study of 1127 BAL procedures, no patient developed pneumothorax,4 while in patients with Acute Respiratory Distress Syndrome, the reported incidence related to BAL is 0.9%.5 To our knowledge, there are no previous reports of pneumothorax due to BAL performed for the diagnosis of NTM disease.
While our patient developed back pain shortly after the procedure, chest radiography did not show pneumothorax at 3h post-procedure. It is possible that the pneumothorax may have been too small to be initially recognized by portable chest radiography. Furthermore, a protracted history of fevers and persistent pain in the days following the procedure may have reflected aggravation of pleural inflammation, thus conceivably increasing the risk of pneumothorax during this later period.
Bronchoscopy is a commonly-used procedure in diagnosing NTM.1 Our case highlights an important complication in patients with NTM who undergo bronchoscopy for diagnostic confirmation. Despite the occurrence of pneumothorax, a definitive diagnosis was obtained, allowing initiation of treatment for an otherwise rapidly-progressive pulmonary infection.
Please cite this article as: Nicholson TT, Mutlu GM. Neumotórax tras lavado broncoalveolar realizado para diagnóstico de infección por micobacterias no tuberculosas. ¿Una complicación «atípica» de la broncoscopia? Arch Bronconeumol. 2016;52:278–279.