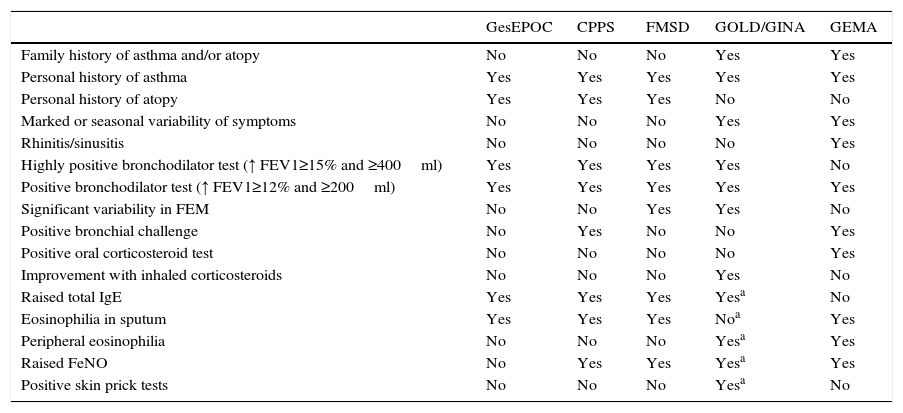
The combination of COPD and asthma in the same patient still raises controversy in international and national guidelines.1–5 The phenomenon (mixed COPD-asthma phenotype in Spanish)1 is called asthma-COPD overlap syndrome – ACOS – in English, but the range of diverging definitions (Table 1) suggests that “chaos” might better describe the current situation.
Characteristics and Parameters Guiding the Characterization of the Asthma-COPD Overlap Syndrome (COPD-Asthma Mixed Phenotype) According to Different Guidelines and Initiatives.
| GesEPOC | CPPS | FMSD | GOLD/GINA | GEMA | |
|---|---|---|---|---|---|
| Family history of asthma and/or atopy | No | No | No | Yes | Yes |
| Personal history of asthma | Yes | Yes | Yes | Yes | Yes |
| Personal history of atopy | Yes | Yes | Yes | No | No |
| Marked or seasonal variability of symptoms | No | No | No | Yes | Yes |
| Rhinitis/sinusitis | No | No | No | No | Yes |
| Highly positive bronchodilator test (↑ FEV1≥15% and ≥400ml) | Yes | Yes | Yes | Yes | No |
| Positive bronchodilator test (↑ FEV1≥12% and ≥200ml) | Yes | Yes | Yes | Yes | Yes |
| Significant variability in FEM | No | No | Yes | Yes | No |
| Positive bronchial challenge | No | Yes | No | No | Yes |
| Positive oral corticosteroid test | No | No | No | No | Yes |
| Improvement with inhaled corticosteroids | No | No | No | Yes | No |
| Raised total IgE | Yes | Yes | Yes | Yesa | No |
| Eosinophilia in sputum | Yes | Yes | Yes | Noa | Yes |
| Peripheral eosinophilia | No | No | No | Yesa | Yes |
| Raised FeNO | No | Yes | Yes | Yesa | Yes |
| Positive skin prick tests | No | No | No | Yesa | No |
CPPS, Czech Pneumological and Phthisiological Society; FMS, Finnish Medical Society Duodecim; GEMA4.0, Spanish Guideline for Asthma Management 4.0; GesEPOC, Spanish COPD Guidelines; GOLD/GINA, Global Initiative for Chronic Obstructive Lung Disease/Global Initiative for Asthma.
The Spanish COPD Guidelines (GesEPOC)1 and other similar documents2,3 recommend evaluating the presence of major and minor criteria, but these do not include clinical symptoms in asthma patients, such as rhinitis, polyposis or wheezing, or seasonal or diurnal variability. Moreover, these guidelines do not address response to corticosteroid treatment, while great importance is given to the bronchodilator test or certain allergic sensitization criteria. The assessment of Th2 inflammation is recommended, but this procedure cannot be performed in routine clinical practice, yet other more accessible variables, such as FeNO or peripheral eosinophilia, are omitted. Moreover, these guidelines, drawn up from the standpoint of COPD, ignore the existence of neutrophilic asthma, a major clinical problem in this setting.
In the GOLD-GINA4 initiative, ACOS is determined on the basis of a numerical score calculated from clinical, functional and radiological criteria characterizing COPD and asthma. This approach makes greater clinical sense, but it seems to lack specificity, and overlooks essential elements, such as smoking history.
Finally, the Spanish Guideline for the Management of Asthma (GEMA)5 recommends that a stepwise approach be taken in patients whose clinical course is indicative of overlapping asthma and COPD. These steps include the attempt to treat with oral corticosteroids, a post-bronchodilator test (the benefit of which in COPD is currently under debate), or a methacholine bronchial challenge test (contraindicated in many of these cases).
We should emphasize that the only thing clear about ACOS is that patients with this syndrome benefit significantly from the inclusion of inhaled corticosteroids in their treatment regimens. As things stand, different treatments could be prescribed for the same patient, depending on the recommendations followed. In our opinion, scientific societies and working groups should work together to produce common criteria that will help clinicians to reach the right decisions.
GesEPOC and GEMA4.01,5 were both spearheaded by the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR), yet surprisingly the recommendations for characterizing what appears to be the same syndrome or phenotype vary widely. Even more surprising is that none of recommended approaches has been validated. The authors of these guidelines, in their zeal to provide a solution to a significant clinical problem, must not forget that the guidelines, far from being an end in themselves, are an instrument, a working tool, in which recommendations must be preceded by research. For this reason, we call for the formation of a working team to define the specific questions that need answers and to carry out the studies needed to produce the best evidence-based consensus document possible.
Please cite this article as: Fernández-Villar A, López-Campos JL. ¿Fenotipo mixto EPOC-ASMA, ACOS o CAOS? Una reflexión sobre las guías y recomendaciones recientes. Arch Bronconeumol. 2016;52:277–278.