Neuroblastoma-like schwannomas or neurilemomas arising from the Schwann cells of the nerve sheath are extremely uncommon benign tumors, first described by Goldblum in 1994.1 They mainly affect the head, particularly the jaw and neck, the flexor surface of limbs and the posterior root of the spinal nerve.1 Tumors tend to be solitary, and in exceptional circumstances occur in the chest wall,2 but they can occasionally be multiple in neurofibromatosis type 2 (NF2) or in the entity known as schwannomatosis.3
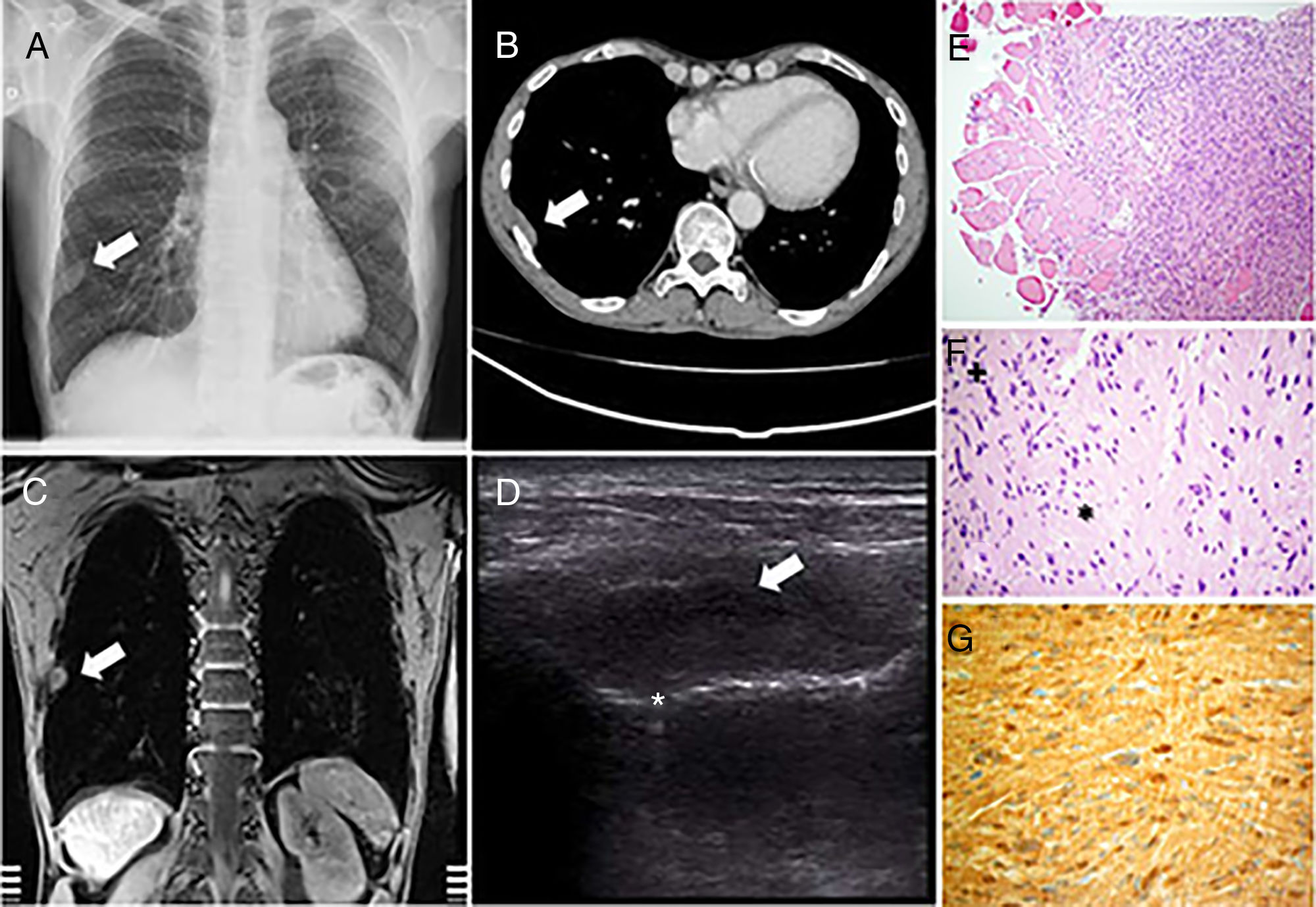
We report the case of a 57-year-old man with an 80 pack-year smoking history, prostate cancer treated with transurethral resection, and rectal cancer in the lower middle third of the rectum, treated surgically, with subsequent chemotherapy and radiation therapy (RT). The patient was clinically stable and asymptomatic from a respiratory point of view. Chest computed tomography (CT) was performed as part of the extension study, revealing well-defined, nonspecific oval pleural nodular thickening in the posterolateral portion of the 8th right intercostal arch measuring 35×11mm. The same lesion was visualized on magnetic resonance imaging (MRI). The patient was referred to our clinic to rule out the existence of pleural metastases. We performed a chest ultrasound, which showed a poorly defined, anechoic, homogeneous lesion in the right chest wall, about 4.3cm long and 1.8cm thick. No infiltration was observed in the visceral pleura located medially to this lesion. Ultrasound-guided biopsy was performed using 14G Acecut® needles with 75mm and 22mm penetration depth (TSK, Japan). The pathology study showed spindle cell proliferation, with no characteristic pattern, swirling cellularity, moderate pleomorphism, occasional karyomegaly, and few mitotic figures, as well as more hypocellular areas with less compact stroma. Immunohistochemistry results were as follows: S100-positive, vimentin-positive, and Sox-10 positive, consistent with schwannoma with focal degenerative changes (Fig. 1).
(A) Posteroanterior chest X-ray. (B) CT with intravenous contrast in mediastinum window. (C) MRI with GRE-T1 sequence after the administration of paramagnetic contrast medium. (D) Ultrasound with linear probe following an intercostal space. The white arrows show a lesion with extrapulmonary features in all images. In the ultrasound image, a linear image can be seen below the lesion corresponding to the pleuropulmonary line that, in the dynamic examination, showed normal movement suggesting no infiltration of the visceral layer. (E) Spindle-shaped cells in a whirling pattern, with trapped muscle and blood vessels. (F) Moderate cellular pleomorphism is observed, with occasional karyomegaly, alternating Antoni A hypercellular areas (+) and Antoni B hypocellular areas (*), with no visualization of mitotic figures. (G) Positivity for S100 protein.
The majority (approximately 95%) of pleural tumors are malignant, and mostly metastatic,4 while benign pleural tumors are unusual. Among the benign tumors, schwannomas usually occur in the posterior mediastinum, especially in a paravertebral site. Schwannomas located in the lateral chest wall are uncommon, and account for less than 5% of these tumors.5 Pathological findings are characteristic and consist of a proliferation of tumor cells growing eccentric to the nerve with a spindle-like appearance; there are densely cellular areas (Antoni A) in which the nuclei are may occasionally palisade to form Verocay bodies, and less compact areas (Antoni B).6 They are almost always positive for S100.
From a clinical point of view, schwannomas may be asymptomatic or cause cough, chest pain, or dyspnea.2 Malignancy is exceptional and has been described primarily in patients who have received RT.7
Chest ultrasound usually shows anechoic tumors and can generally discriminate well between benign and malignant tumors.8 However, in our case, the image lacked well-defined borders, and given that the existence of pleural metastasis could have therapeutic implications, we decided to perform an ultrasound-guided biopsy of the lesion.
Other imaging techniques should clarify the differential diagnosis between solitary pleural lesions, such as lipomas, single metastatic lesions, mesotheliomas, fibrous tumors, and other neurogenic tumors. In schwannoma, CT with contrast can distinguish heterogeneous lesions with different cellularity demarcating the Antoni type A or B areas, with enhancement of the former suggesting areas of cystic degeneration.9 On MRI, schwannomas usually display an isointense image in T1, similar to muscle, sometimes called the “split fat sign” that appears as a peripheral margin of displaced fat in the neurovascular bundle,10 with hyperintense signal in T2, although the cystic regions may have a low signal intensity. MRI is also useful for visualizing vascular involvement. Positron emission tomography/computed tomography (PET/CT), however, is of limited utility, given that often shows high uptake,11 even in benign tumors, preventing the differential diagnosis with metastases of tumors from another source.
Treatment is usually surgical and recurrence after treatment is unusual.12 However, in view of the lack of symptoms and the accompanying underlying disease of our patient, we decided to maintain a conservative attitude, while monitoring his clinical and radiological progress.
Please cite this article as: López González FJ, García Alfonso L, Enríquez Rodríguez AI, Torres Rivas HE. Schwannoma pleural que simula metástasis pleural de un carcinoma de recto. Arch Bronconeumol. 2019;55:110–111.