The most unusual extraintestinal manifestations of inflammatory bowel disease (IBD) are respiratory, and ulcerative colitis (UC) is the most common causative entity. Clinical presentation is variable, ranging from asymptomatic patients to cases that present with cough, dyspnea, and respiratory failure. One peculiar characteristic is that pulmonary involvement does not always occur in parallel to intestinal tract disease, making it difficult to diagnosis. Pulmonary necrobiotic nodules as pulmonary complications of Crohn's disease (CD) are an exceptional manifestation, calling for a differential diagnosis with neoplastic diseases and infectious diseases, characterized by an excellent response to treatment with corticosteroids. Very few cases have been reported in the literature on this entity, and all of them presented with pulmonary symptoms, such as cough and dyspnea. We report the case of a patient with CD without respiratory manifestations, in whom pulmonary necrobiotic nodules were an incidental radiological finding.
A 26-year-old woman consulted for diarrhea, with a 2-year history of 6–10 stools per day of liquid consistency with blood and mucus, abdominal pain, and weight loss. She was a smoker of 10 cigarettes a day and had no other clinical history of interest. Physical examination revealed poor general condition and painful abdomen on palpation in the epigastrium. Cardiopulmonary auscultation was normal, and no adenopathies or skin lesions were observed. Clinical laboratory tests were significant for hemoglobin 10.5g/dl and transferrin saturation 5.1%, platelets 393000/ml, and eosinophils 1000/ml. Chest radiograph was normal. Stool cultures at the time of the study were negative. Ileocolonoscopy showed swollen and erythematous mucosa with crater-like, serpiginous ulcers alternating with normal mucosa. The pathology report was suggestive of CD. Treatment began with oral budesonide 9mg/day and mesalazine 2g/day, with clinical improvement.
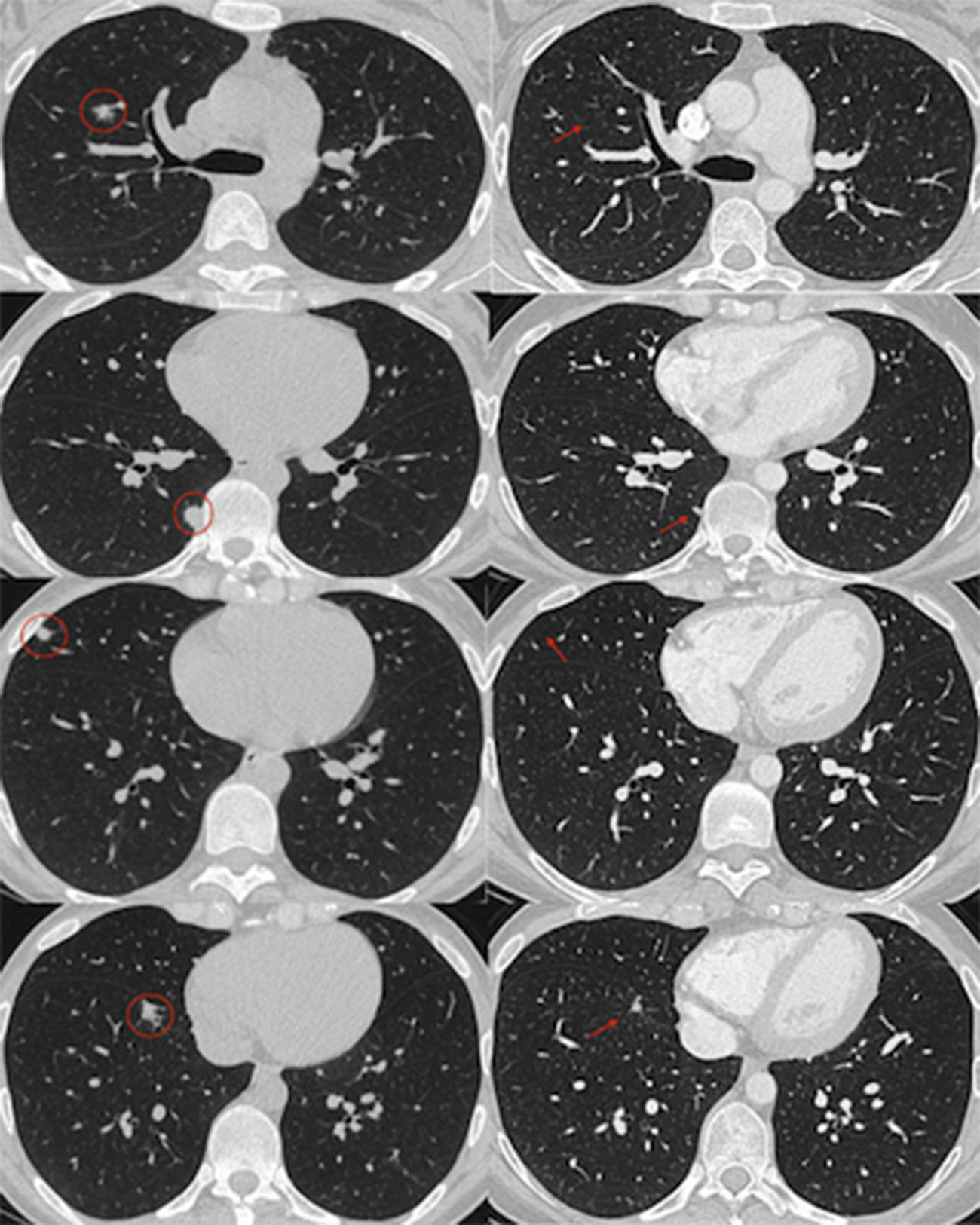
The patient's digestive symptoms subsequently improved, but lobar pneumonia developed, which was treated with levofloxacin. However, several lung nodules measuring 8–10mm in diameter were identified in the X-ray performed to monitor radiological progress when the respiratory symptoms had resolved, and confirmed on a chest CT scan (Fig. 1). Bronchoscopy was normal with no tumor cells or pathogens in bronchoalveolar lavage (BAL). Other diagnoses, including metastasis and abscesses, were considered in the differential diagnosis. The diagnosis of pulmonary necrobiotic nodules associated with CD was given, in view of the temporal relationship between the diagnosis and IBD flare-up, and the good condition of the patient. She was treated with systemic corticosteroids, and radiological resolution of the nodules was achieved after 1 month of treatment (Fig. 1).
Chest CT. Pulmonary nodules at diagnosis and after 1 month of treatment. On the left, chest CT images showing lung nodules of varying size (circles) in the right middle and lower lobes and the paravertebral region. On the right, images showing complete resolution of some of the nodules (arrows) after one month of treatment, and others reduced in size.
IBD is a chronic inflammation of unknown etiology, which affects the digestive tract. Pathogenesis is due to a recurrent inadequate response of the mucosal immune system, activated by the presence of normal luminal flora in genetically predisposed individuals. It is histologically characterized by a lymphocytic polymorphonuclear infiltrate with formation of granulomas, ulcers, and fissures in the mucosa. Although it mainly affects the intestine, extraintestinal manifestations are well-known, with a prevalence of 21%–41% that increase as the disease progresses.1
Pulmonary involvement as an extraintestinal manifestation was first described by Kraft et al. in 1976 after observing 6 patients with a diagnosis of IBD who developed chronic bronchial suppuration.2 Different pathogenic mechanisms for the pulmonary involvement in these patients have been described, including the common embryological origin of the airway and the intestine, a similar immune system, and the presence of circulating immune complexes and autoantibodies.3 This is the most unusual extraintestinal manifestation of IBD and is usually seen in patients with UC, distinguishing it from other extraintestinal manifestations. Its real prevalence is unknown because it is sometimes asymptomatic or does not coincide chronologically with the IBD.1 All these factors make diagnosis difficult in the absence of a high suspicion. However, early identification is important to prevent it progressing to a more disabling condition and to avoid complications.
The most common symptoms are derived from airway inflammation (cough, expectoration, or dyspnea), which manifests in many ways, ranging from asymptomatic disease to involvement of the tracheobronchial tree (bronchitis, bronchiectasis or bronchiolitis), the lung parenchyma, and the pleura.
A distinction must be drawn between pulmonary involvement caused by IBD and that caused by IBD treatment, the latter being the most frequent. IBD treatment that might cause pulmonary involvement includes the long-term use of sulfasalazine, mesalazine, methotrexate, and anti-tumor necrosis factor (anti-TNF), rather than the underlying disease.
Pulmonary necrobiotic nodules in IBD are an exceptional complication and are more frequent in UC. This presentation was first described in patients with rheumatoid arthritis or pneumoconiosis (Caplan's syndrome). Histologically, necrobiotic nodules are sterile aggregates of neutrophils, which frequently cavitate.4
Radiologically, the differential diagnosis must consider pulmonary nodules of infectious origin (tuberculosis, fungi, staphylococci), autoimmune diseases, cancer, etc. In our case, the absence of fever, absence of neoplastic cells in BAL, and absence of eosinophils in BAL ruling out any association with mesalazine, led us to start empirical treatment with corticosteroids, with good response. Based on these findings, lung biopsy was avoided, pending clinical response and response to the new treatment.
Very few cases have been reported in the literature on this entity, and all of them presented with respiratory symptoms, including cough and dyspnea.5–9 This makes our patient even more unique, since she did not present respiratory manifestations, and diagnosis was made from an incidental finding.
Although the spontaneous resolution of necrobiotic nodules in IBD has been described, of the 5 cases associated with CD, only 1 resolved spontaneously.6 The other patients were treated with oral prednisone, with complete resolution. Infliximab is currently being used for lung nodules that are refractory to systemic steroids.10
Please cite this article as: Larrey Ruiz L, Sabater Abad C, Peño Muñoz L, Huguet Malavés JM, Juan Samper G. Nódulos necrobióticos pulmonares: una manifestación excepcional de la enfermedad de Crohn. Arch Bronconeumol. 2019;55:108–110.