Bronchiolitis obliterans (BO) is an entity that has been described in pediatrics as a complication of various diseases, including immunodeficiencies.1,2
We report the case of an 11-year-old boy with autosomal recessive polycystic kidney and hepatic disease (2 PKHD1 gene mutations). History significant for: chronic renal impairment, left pyelostomy, arterial hypertension, hemophagocytic syndrome at the age of 3 years due to a viral infection, hepatic fibrosis, and severe hepatosplenomegaly with chronic secondary pancytopenia. He continues to present exacerbations of pancytopenia coinciding with infectious episodes, with no medullary involvement. No respiratory history of interest. At the time of admission, he had been on the waiting list for liver-kidney transplantation for 1 year.
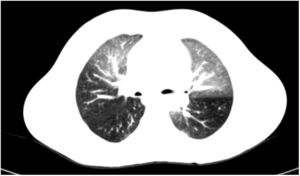
He consulted due to a febrile episode lasting 48h, with sparsely productive cough as the only symptom. On examination, he showed good general status, asthenia, mild tachypnea, and fine crackles in the right lung base. Clinical laboratory tests showed C-reactive protein 220mg/l and procalcitonin 7.4ng/ml, deteriorating creatinine clearance and worsening of baseline pancytopenia. Chest radiograph was normal. With sepsis of gastrointestinal origin as an initial diagnosis, treatment began with meropenem; the patient became afebrile 24h later and his infection parameters improved. Urinary, gastrointestinal, and ENT infectious foci and pneumonia were ruled out. Despite clinical improvement, bilateral pulmonary and migratory crackles persisted, with normal oxygen saturation at all times, so during the week that he was hospitalized, the following tests were conducted: pulmonary ventilation–perfusion scintigraphy, normal; spirometry, mixed pattern; diffusing capacity of the lung for carbon monoxide, lower limit of normal; and finally high-resolution CT (HRCT) that confirmed the suspected diagnosis of BO (Fig. 1, mosaic attenuation pattern).
The treatment of BO is complex, complicating the management of our patient and conferring an unfavorable prognosis. On the one hand, BO contraindicated kidney-liver transplantation and, in turn, lung transplantation would probably be required to cure possibly advanced BO in the future, yet that would be ruled out by the patient's renal impairment.1 The patient was taken off the kidney-liver transplantation waitlist. Pulmonary treatment began with inhaled budesonide (800μg/day),3 salbutamol on demand, and azithromycin (250mg/3 days per week). Post-infective BO was considered the most likely etiology, but this diagnosis was ruled out after polymerase chain reaction (PCR) was negative for respiratory viruses in 2 nasopharyngeal samples.4 Chronic immunosuppression due to pancytopenia secondary to continued hypersplenism was then thought to be the likely etiology of the BO. Splenectomy was performed, and an immediate improvement in neutropenia and thrombocytopenia was observed after surgery. Anemia persisted due to the patient's chronic kidney failure. After 3 months of respiratory treatment, he was symptom-free, spirometry was normal, and HRCT showed no lesions. Given the resolution of the BO and pancytopenia, respiratory therapy was discontinued, and the patient was included in the transplantation list again. The procedure was performed 6 months later with satisfactory progress to date.
BO is a clinical syndrome characterized by chronic and irreversible airflow obstruction caused by inflammatory changes associated with fibrosis in the small airway.2,5 The most common etiologies in children are immunosuppression and postinfective syndromes.1,4 The clinical picture in most patients is very nonspecific, so the initial diagnostic approach is difficult.4,5 Before BO is suspected, spirometry must show a fixed obstructive pattern and the characteristic mosaic attenuation pattern (areas of air trapping and atelectasis, and bronchial dilation) must be observed on HRCT (inspiration and expiration). Biopsy is usually not required if HRCT is available.5 The initial treatment consists of combined therapy with inhaled glucocorticoids, macrolides, and beta-2 adrenergic bronchodilators.3 When the disease is established, this treatment is supportive and must include immunosuppressive drugs. Lung transplantation is indicated in patients who have progressed.1
In our patient, respiratory therapy and splenectomy led to clinical improvement, so in the absence of other data, the most likely etiological hypothesis was chronic immunodeficiency secondary to pancytopenia that generated hypersplenism due to liver fibrosis.
Please cite this article as: Ibáñez Beltrán L, García Sánchez JM, Cortell Aznar I, Mendizábal Oteiza S. Bronquiolitis obliterante en paciente con poliquistosis hepatorrenal en lista para trasplante. Arch Bronconeumol. 2019;55:112.