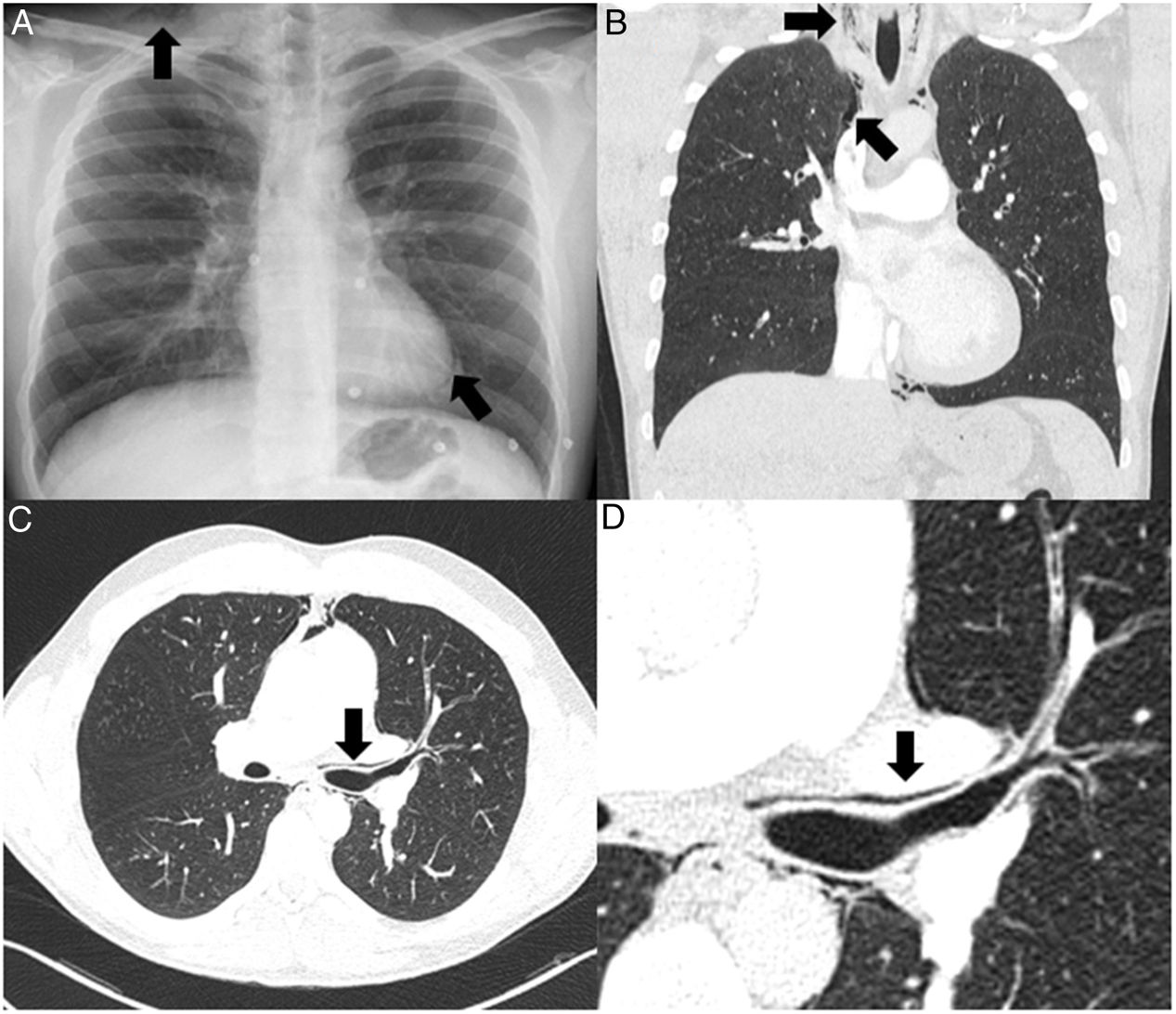
A 27-year-old man with a history of asthma was seen in the emergency department for acute respiratory failure, associated with signs of bronchospasm and fever of 38.5 °C. A chest X-ray was performed, revealing pneumomediastinum associated with subcutaneous emphysema (Fig. 1A), with no criteria for pleural drainage. No foci of condensation associated with pneumonia were observed. Given a diagnostic orientation of acute bronchitis, bronchodilator treatment and antibiotic therapy with amoxicillin-clavulanic acid were initiated. Although the patient showed some improvement, with resolution of bronchospasm, he continued to require supplementary low-flow oxygen therapy, so a CT angiogram was performed. This ruled out pulmonary embolism, but revealed areas of peribronchovascular emphysema, also known as the “Macklin effect” (Fig. 1C and D). Mediastinal emphysema and the previously reported subcutaneous emphysema were also observed (Fig. 1B). The patient showed progressive clinical improvement with the previously prescribed treatment.
(A) Plain chest X-ray in posteroanterior projection showing pneumomediastinum and subcutaneous emphysema (arrows). (B) Coronal reconstruction of the chest CT scan (lung window) confirming the presence of pneumomediastinum and subcutaneous emphysema (arrows). (C) Axial image of the chest CT (lung window) showing left peribronchial emphysema with pneumomediastinum (arrow) – the Macklin effect. (D) Enlarged image of peribronchial emphysema (arrow).
The pathophysiology of spontaneous pneumomediastinum was first described in 1937 by Charles Macklin. It is caused by abrupt increases in airway pressure, which result in the rupture of the alveolar septa and subsequent gas leakage through the peribronchovascular sheaths, producing a characteristic image of peribronchial emphysema (Fig. 1C and D) and mediastinal dissection1,2. Treatment is conservative, with oxygen therapy, rest, and analgesia.
Please cite this article as: Ferreiro A, Granados G, Villar A. Enfisema peribroncovascular. Efecto Macklin. Arch Bronconeumol. 2021;57:697.