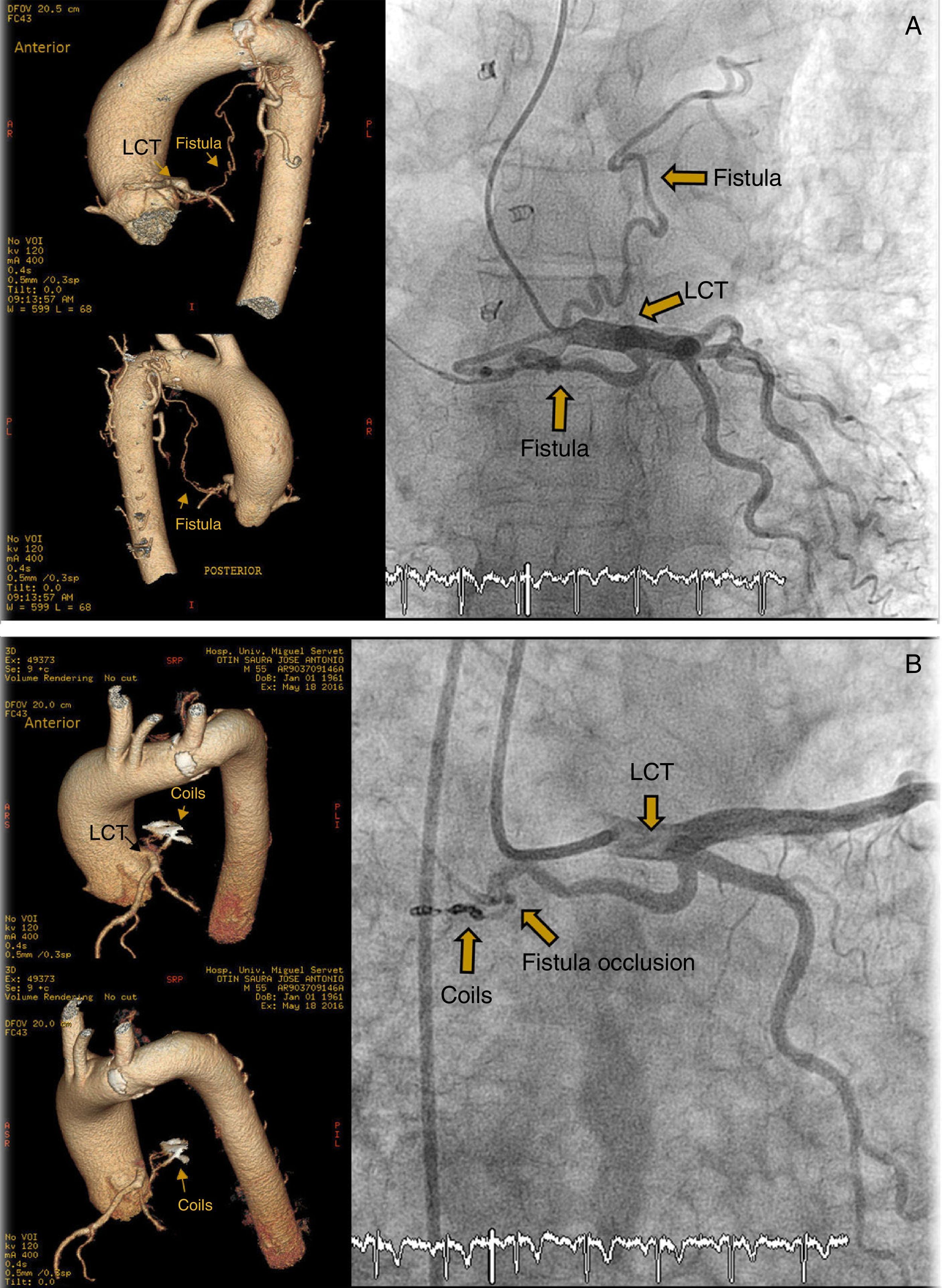
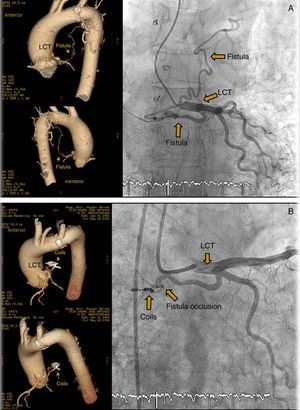
We report the case of a 54-year-old man, waitlisted for lung transplantation with a diagnosis of end-stage diffuse bronchiectasis. On arrival at the catheterization laboratory for coronary angiography prior to transplantation, the patient developed a hypertensive crisis (BP 200/110mmHg), at which stage he reported habitually uncontrolled blood pressure. Coronary angiography revealed coronary arteries free of lesions and a coronary artery fistula emerging from the left common trunk (LCT), 3mm in caliber at the proximal end and 2mm at the most distal end (Video 1, Appendix), with drainage to the left pulmonary artery, causing hemodynamic alterations in the form of high cardiac output (thermodilution 7.86l/min). Increased pulmonary pressures (mPAP 71mmHg, PVR 5.5 Wood units [WU]) associated with pulmonary hyperflow and significant diastolic dysfunction due to hypertensive heart disease evidenced in the rest of the study data (mean PCP 35mmHg and left ventricular end-diastolic pressure [LVEDP] 25mmHg). The examination was completed with heart computed tomography (Fig. 1A). Transesophageal echocardiography (TEE) showed involvement of right chambers, while the bubble test ruled out intra-cardiac shunt. Diastolic changes with LV parietal hypertrophy and normal LV systolic function were confirmed. Percutaneous closure of the fistula in the proximal/medial segment was performed with 3 coils measuring 3mm×4mm and 3mm×2mm. Occlusion was confirmed immediately with fluoroscopy (Video 2, Appendix), and subsequently with a follow-up coronary CT one month after the procedure (Fig. 1B). Follow-up right heart catheterization revealed a marked improvement in mPAP (48mmHg) after resolution of pulmonary hyperflow (cardiac output 4.3l/min and aPVR 4.6 WU), and persistently elevated PWP and LVEDP associated with the patient's hypertensive left heart disease (PWP 25mmHg and LVEDP 23mmHg).
Coronary artery fistulas are abnormal connections between a coronary artery and one of the heart chambers or one of the vessels located around the heart.1,2 Most are congenital, but they may also be acquired.1 Coronary artery fistulas are observed in 0.2%–0.6% of all angiograms.1 Most patients are asymptomatic; however, the fistula can sometimes form an arteriovenous short circuit with hemodynamic repercussions, generating heart failure due to volume overload caused by the left-to-right shunt, ischemia due to coronary steal syndrome, fistula rupture or thrombosis, arrhythmias, and infectious endocarditis.1,2
In adults it is usually an incidental finding during a coronary angiography,1 as was the case with our patient during the pre-lung transplant study. Some authors recommend closure of the fistula, even in asymptomatic patients.2 Reidy et al.1,3 performed the first percutaneous closure in 1983, and since then this procedure has been considered an effective and less traumatic option than surgical closure.2 Several authors have demonstrated its safety and effectiveness3,4 in the management of this disease, reserving surgical closure for multiple or large fistulas.2 Several devices have been used for percutaneous closure, the most commonly used being coils and Amplatzer vascular plugs. Amplatzer vascular plugs are usually used in longer, wider fistulas, and coils in smaller fistulas.3,4 Fistulas usually originate in the left anterior descending artery, followed by the right coronary and circumflex arteries,1,3 and frequently drain into the pulmonary artery.1 Approximately 10% of closures are incomplete or recurrent.1
Percutaneous closure of coronary artery fistula prior to lung transplantation is a safe and effective option that reduces the risk associated with volume overload, coronary steal and other complications encountered in patients with this anomaly.
Please cite this article as: Urmeneta Ulloa J, Molina Borao I, Ochoa Rea ME, Sánchez-Insa E. Embolización percutánea en fístula de arteria coronaria previo al trasplante pulmonar. Arch Bronconeumol. 2017;53:520–521.