Leiomyosarcoma of the pulmonary artery is an entity that is highly difficult to diagnose, due to its low prevalence and similarity to pulmonary embolism (PE). We report the case of a patient in whom the results of magnetic resonance imaging (MRI) and positron emission tomography (PET-CT) changed the diagnosis from suspected PE to pulmonary artery leiomyosarcoma, subsequently confirmed by endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA).
A 58-year-old man with type 2 diabetes, former smoker of 25 pack-years, underwent transthoracic echocardiogram as part of a kidney donor protocol. This procedure revealed right heart dilation and estimated systolic pulmonary artery pressure (SPAP) of 60mmHg. He presented dyspnea mMRC grade 2, and no other clinical manifestations.
On physical examination, breathing was normal, with basal SpO2 96% and blood pressure 140/100mmHg. A II/IV systolic murmur was detected in the aortic area, and the rest of the examination was normal.
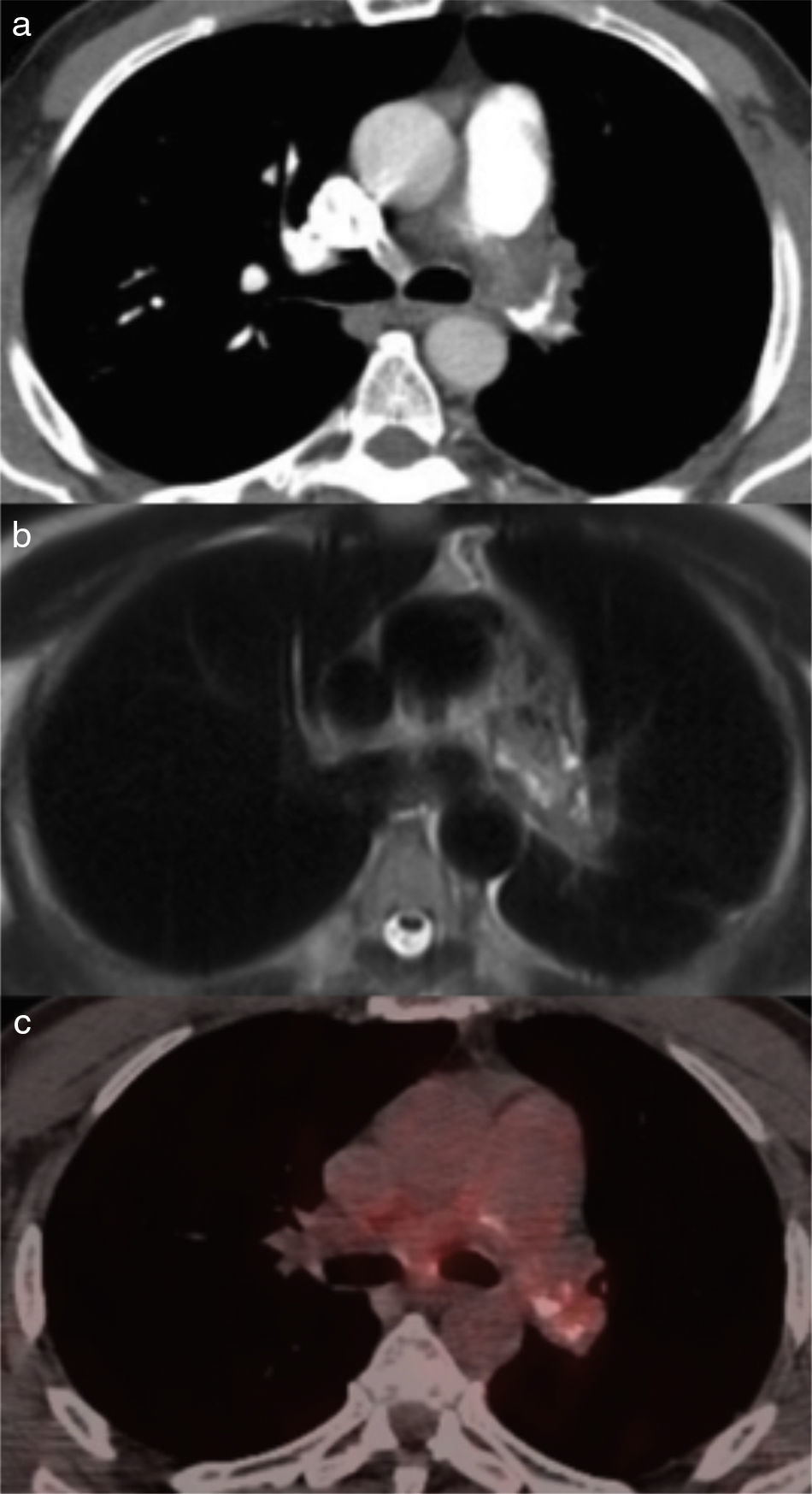
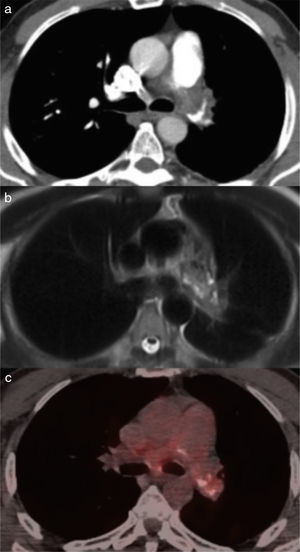
Findings suggestive of enlarged right heart were observed on electrocardiogram. Chest radiograph was normal. Pulmonary hypertension due to an interatrial communication was suspected, so we performed a transesophageal echocardiogram (TEE) which ruled out this hypothesis, but revealed a reduced pulmonary artery diameter. Computed tomography angiography (CT angiogram) was requested, which showed occlusion of the left and partial occlusion of the right pulmonary arteries and an increase in the diameter of the pulmonary conus, suggestive of chronic bilateral PE (Fig. 1a).
Although the patient did not have any known risk factors, PE was assumed and anticoagulant therapy was initiated, while additional testing was being performed. A pulmonary scintigraphy was requested, which confirmed the absence of left lung perfusion and no changes in the right lung. Right heart catheterization confirmed severe pulmonary hypertension. However, both D-dimer and Doppler ultrasonography of the lower limbs were negative. Thrombophilia, inflammatory markers, tumor markers, and autoimmunity markers were also negative. After 3 months of anticoagulation, the patient's dyspnea persisted. A follow-up CT angiogram showed an increase in the filling defect in the right pulmonary artery, along with isolated pulmonary infiltrates.
In view of his poor progress, a chest MRI with contrast medium was requested, showing a mediastinal mass with the same intensity as the muscles in T1, and hyperintense in T2 due to contrast uptake, suggestive of leiomyosarcoma of the pulmonary artery (Fig. 1b). The lesion occupied the entire lumen of the left pulmonary artery and part of the common trunk of the pulmonary artery, with infiltration of the mediastinal fat surrounding the affected vessels, aortopulmonary window and ascending thoracic aorta. Uptake in this region was also observed on whole-body PET-CT (Fig. 1c), with no other focal enhancement. The pathological diagnosis of leiomyosarcoma was confirmed by fine needle aspiration (FNA) of the mass by EBUS-TBNA through the nodal station 7, with neoplastic cells expressing vimentin, smooth muscle actin and desmin. The procedure was performed without complications. Due to its extension, the lesion was considered unresectable. The patient died suddenly a few days after the diagnosis was reached.
Leiomyosarcoma of the pulmonary artery is a rare malignant tumor, and just over 100 cases have been reported in the literature.1 Symptoms are often nonspecific and insidious, with signs of right ventricular dysfunction being found on physical examination. The chest radiograph can show pulmonary nodules, dilation of the pulmonary artery, hypoperfusion, and cardiomegaly, but it can also be normal. Transthoracic echocardiogram generally reveals right ventricular dilation and high estimated SPAP; obstruction of the pulmonary artery trunk with no clear cause is sometimes observed. The usefulness of TEE has not been defined.2 CT angiogram detects filling defects in the lumen of the pulmonary artery, but it might not differentiate between a clot and a tumor in the absence of secondary lesions, such as pulmonary nodules or enlarged lymph nodes.3 Differential diagnoses include pulmonary artery arteritis, congenital pulmonary stenosis, chest neoplasms, and chronic PE. Of these, the most common is chronic PE; the other entities are exceptional.
This, along with the lack of symptoms suggestive of a tumor process, makes diagnosis a complex matter. However, lack of response to anticoagulation and the presence of a massive unilateral perfusion defect on the pulmonary scintigraphy should prompt clinicians to reconsider the diagnosis.
The 2 non-invasive tests that can differentiate between clots and masses are MRI with gadolinium contrast and PET-CT: in the MRI, tumor tissue captures contrast material, while a clot does not.3 It has also been demonstrated recently that an increase in 18-fluoro-2-deoxy-D-glucose uptake in a filling defect on PET-CT is suggestive of malignancy.4
The definitive diagnosis is reached by a pathology study, generally by autopsy, biopsy, or directly during the surgical act. Diagnosis by EBUS-TBNA, while unusual, has been described previously with good results, and can be proposed as a feasible technique for differentiating between a clot and a tumor.5 The major risk of this technique is bleeding, particularly in patients with pulmonary hypertension, and this risk is increased even further by enlarged bronchial arteries which may be associated with proximal obstruction of the pulmonary arteries.6 However, the probability of bleeding is minimized by using color Doppler combined with real-time ultrasonography to avoid puncturing areas of high blood flow.7,8 To date, no serious complications have been reported with the use of the EBUS-TBNA in this context.9 For this reason, EBUS-TBNA is being accepted as a new safe, minimally invasive technique for the diagnosis of mediastinal tumors, including tumors of the pulmonary artery. The treatment of choice is complete surgical resection, and if the tumor is unresectable, prognosis is grim.
Please cite this article as: Romero Francés L, Royo Prats JA. Leiomiosarcoma de arteria pulmonar, diagnóstico mediante resonancia magnética, PET-TC y EBUS-TBNA. Arch Bronconeumol. 2017;53:522–523.