We report the case of a 73-year-old man, active smoker with a history of 60 pack-years, a former alcohol habit, hypertension and ischemic heart disease, with acute myocardial infarction 15 years previously. He was seen for a 12-month history of pain, weakness and paresthesia in the lower limbs, and lumbago. He also reported cough, mucopurulent expectoration and dyspnea on slight exertion, with no associated toxic syndrome. Physical examination revealed mild tachypnea and generalized bilateral diminished breath sounds with no adventitious sounds. Neurological examination showed no changes in campimetry or cranial nerves, and functional tests were normal. Gait was cautious, with proximal weakness of the lower limbs and loss of triceps, patellar and Achilles reflexes. The patient was referred to the neurology department, from where he was admitted to hospital.
General laboratory tests showed no significant findings. Protein levels and cerebrospinal fluid were normal, as were tumor markers AFP, CEA, Ca 125, Ca 19.9, Ca 15.3 and PSA. No pathological findings were seen on chest X-ray. The neurophysiological examination suggested demyelinating polyneuropathy. Head computed tomography (CT) showed bilateral frontotemporal atrophy, and the initial chest CT was normal. Magnetic resonance imaging of the cervical, dorsal and lumbar spine revealed only a foraminal disc protusion with no radicular involvement. An antibody study was negative for antigangliosides and anti-MAG (anti-myelin-associated glycoprotein) and positive for anti-Hu antibodies.
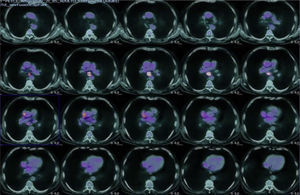
In view of the strong suspicion of a neoplastic process, PET-CT was performed, revealing a slightly hypermetabolic focus over a small infiltrate in the right subpleural lung base, and a large hypermetabolic focus in the subcarinal mediastinum, 3cm×2cm in size (Fig. 1).
No pathological endobronchial findings were observed on flexible bronchoscopy. Aspirates were obtained from the G7 region, and the cytological examination of these samples provided a diagnosis of small-cell anaplastic bronchogenic carcinoma. The patient was referred to the oncology department for treatment.
The association of paraneoplastic syndromes (PSs) with malignant tumors is well known, and any body organ or tissue can be affected. PS occurs in approximately 10% of the patients with lung malignancies, and is more common in small-cell carcinoma.1 Although most of the neurological complications of lung cancer are due to metastases, there are several neurological PSs, one of the most common being polyneuropathy. Clinical features of paraneoplastic polyneuropathy include the subacute development of asymmetric sensorial changes, such as pain, paresthesia and numbness affecting the distal extremities.2 Polyneuropathy can appear more than 1 year before the diagnosis of cancer, as occurred in our case.
In an adult with peripheral polyneuropathies and a long-term history of smoking, seropositivity for anti-neuronal nuclear autoantibodies type-1 (ANNA-1), also known as anti-Hu, is a marker for small-cell lung cancer.3 The pathogenic mechanism of these antibodies is probably due to these antibodies accumulating in the neurons of the nervous system. These antibodies can be detected in small-cell carcinoma patients without neurological symptoms, but not in healthy subjects.4 Management of this syndrome includes treatment of the underlying cancer, but this does not generally help the neurological symptoms, which tend to progress rapidly.5
Please cite this article as: Valenzuela Membrives MM, Sánchez Palop M, Esquivias López J. Neuropatía paraneoplásica con anti-Hu positivo. A propósito de un caso. Arch Bronconeumol. 2015;51:252–253.