Intravascular space-occupying lesions of the pulmonary artery are uncommon and diagnosis can be delayed due to non-specific accompanying clinical data.1 Primary tumors originating in systemic blood vessels are very rare, and even rarer in the pulmonary artery. We report the first case described in the literature of small-cell lung cancer metastasis in the trunk of the pulmonary artery.
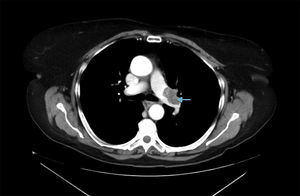
A 68-year-old woman presented with a history of colon and thyroid cancer, and in situ epiglottal carcinoma. In June 2011, fiberoptic bronchoscopy returned a diagnosis of small-cell lung cancer in the anterior segment of the left upper lobe (LUL), for which she received 6 cycles of CDDP-VP-16, and chest and whole-brain radiation therapy (RT). Treatment was completed in November 2011. On radiological studies, a space-occupying lesion was seen in the left pulmonary artery, suggestive of an intramural thrombus (Fig. 1), so anticoagulant treatment was administered for 1 year.
Follow-up radiological studies showed progression of the intra-arterial lesion, suggesting that it might be a tumor. As it was impossible to obtain a sample for histology from this site, surgery was undertaken for the purposes of diagnosis and treatment. Left intrapericardial pneumonectomy with arterial section extending to the disease-free zone was performed. Pathology results confirmed small-cell lung cancer with disease-free surgical margins. No intrathoracic complications occurred during the post-operative period. The patient is currently being followed up by the medical oncologist and has shown no signs of recurrence of her lung disease.
Malignant tumors within the pulmonary artery may be rare, but they must be considered in the differential diagnosis of pulmonary embolism; in half the cases, diagnosis is made postmortem,2 but advances in diagnostic imaging techniques mean that more cases are being detected. Shepard et al. published 4 cases of intravascular tumor in the pulmonary artery detected in 14,000 consecutive chest CTs, and concluded that the images of the peripheral branches of dilated pulmonary arteries could be highly suggestive of tumor emboli.3 In a review of 1085 autopsies of patients with a known diagnosis of solid malignant tumors, metastases causing intraarterial obstruction were found to occur in cancers with access to large veins, such as hepatocarcinomas, choriocarcinomas and renal cell carcinomas.4
In our case, a primary lesion was suspected due to the slow progress observed in radiological monitoring and the possibility of tumor relapse was ruled out in view of the stability of the LUL lesion.
The intrapericardial site of the lesion posed problems, including a high risk of bleeding during histological sampling. For this reason, a surgical approach was taken, and an intrapericardial pneumonectomy was performed, in view of the tumor location. Decision-making in this case was a tangible diagnostic and therapeutic challenge.
Please cite this article as: Laguna Sanjuanelo S, Zabaleta J, Aguinagalde B. Lesión intraluminal en la arteria pulmonar: un reto diagnóstico. Arch Bronconeumol. 2015;51:253–254.