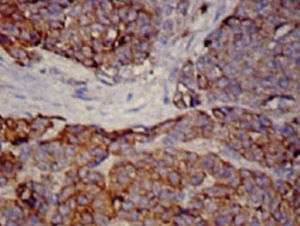
We report the case of a 69-year-old woman admitted with a 7-month history of anorexia and asthenia, along with unsteadiness, vomiting, tremor and double vision. She also reported a 1-month history of dyspnea and voice changes. On examination, she presented a bitonal voice, ataxic gait and dysmetria, with intention tremor in the left arm. Magnetic resonance imaging (MRI) of the head revealed a small lacunar infarction, which did not explain the clinical symptoms. Blood work, biochemistry, proteins, immunoglobulins, thyroid profile, vitamin B12, vitamin E and folate were normal, and serologies for HIV, hepatitis, cytomegalovirus, Epstein–Barr virus, syphilis and Borrelia were all negative. Cerebrospinal fluid cytochemistry was also normal. Carcinoembryonic antigen and neurospecific enolase tumor markers were elevated at 30.4ng/ml (0–5ng/ml) and 21.7ng/ml (0–16ng/ml), respectively. Computed tomography (CT) of the chest and abdomen revealed a mass in the upper mediastinum, measuring 70mm×40mm, suggestive of clustered lymphadenopathy. An immune-mediated process was suspected, so antinuclear antibodies and onconeuronal antibodies were tested, but these were negative, with anti-glutamic acid decarboxylase antibodies (anti-GAD) 2.4U/ml (0–5U/ml) and anti-acetylcholine receptor antibodies 0.01nmol/l (0–0.1nmol/l). F-18 fluorodeoxyglucose uptake on a positron emission tomography scan suggested malignancy, so a biopsy was obtained by mediastinoscopy. The pathology report confirmed small cell neuroendocrine carcinoma of the thymus, positive for chromogranin and synaptophysin (Fig. 1). A scintigraphy (octreoscan) was then performed to complete the examination, showing 111indium-pentetreotide uptake in the tumor and supraclavicular lymph node metastases. The patient underwent surgical resection and received chemotherapy with carboplatin and etoposide. She achieved full remission of the cancer and almost complete resolution of her neurological symptoms, although tremor at rest did persist.
Neuroendocrine tumors (NET) are rare cancers, generally found in the gastrointestinal tract, although they may occur in the lung, thymus, ovaries and non-parenchymatous tissue. Thymic NETs account for less than 5% of mediastinal tumors.1 Approximately 30% are malignant, although this rate rises to 82% if they are located in the thymus.1 They present as a mediastinal mass mainly in patients aged 30–50 years, and are 3 times more common in men.2 Local clinical manifestations can range from dysphonia or dyspnea to superior vena cava syndrome, and one-third of patients have endocrine symptoms associated with multiple endocrine neoplasia syndrome. CT, MRI and 123I-metaiodobenzylguanidine scintigraphy are useful, but the octreoscan is the most sensitive procedure (71%–100%) for detecting NETs, depending on the somatostatin receptors expressed by the tumors. Histology examination shows cell nests with fibrovascular tracts, positive for neuroendocrine markers such as chromogranin, synaptophysin and neuroenolase. Paraneoplastic cerebellar degeneration (PCD) is the most common paraneoplastic neurological syndrome. In 18%–50% of cases, no antibodies are identified,3 and in early stages of the disease, MRI is normal.4 It is associated with several neoplastic processes, including thymic NETs.5
In view of the favorable response to specific cancer treatment, we classified our case as seronegative PCD associated with thymic NET.
Please cite this article as: Serrano-Martínez JL, Zamora-Pasadas M, Redondo-Orts M. Degeneración cerebelosa paraneoplásica asociada a carcinoma neuroendocrino mediastínico de células pequeñas. Arch Bronconeumol. 2015;51:659–660.