High flow nasal cannula (HFNC) oxygen therapy is a recently introduced alternative to conventional oxygen therapy. It uses a system that mixes oxygen and air to administer an FIO2 of 21%–100% at flow velocities of up to 60 lpm. To avoid condensation, the mixture of oxygen and air passes through a humidifier to a heated inspiratory circuit. This mixture is then administered to the patient by way of wide-bore nasal cannulae. The most important feature of HFNC is that it can be used to administer a humidified flow higher than the maximum inspiratory flow, and, moreover, the real FIO2 can be more reliably assessed.
We report 3 patients with acute respiratory failure despite conventional oxygen therapy, who received HFNC in a hospital ward using an Optiflow® device, AIRVO 2® model (Fisher & Paykel).
Patient 1 was a 71-year-old man with a history of stage IIIA epidermoid lung cancer, treated with right upper lobectomy, hilar and mediastinal lymphadenectomy, chemotherapy and radiation therapy. Areas of honeycombing indicative of radiation-induced fibrosis were seen on successive tomography follow-ups. The patient was admitted for an episode of respiratory infection. He received conventional oxygen therapy (COT) via nasal prongs, antibiotics, nebulized bronchodilators and intravenous corticosteroid therapy. On day 10 of admission, the patient's respiratory status declined, and he developed heart failure with hypoxemic respiratory failure (Table 1). Treatment began with high flow oxygen therapy at an initial FIO2 of 100% and a flow of 50lpm. The patient tolerated the device well, and reported greater comfort compared with nasal prongs (9/10 compared to 6/10, respectively) and an absence of mouth dryness. His respiratory situation improved significantly, and the device was withdrawn 48hours later.
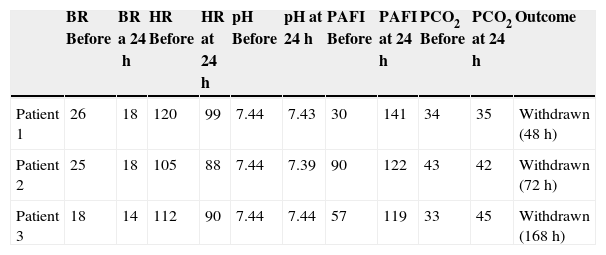
Clinical Parameters of Patients Before and 24Hours After Starting HFNC.
| BR Before | BR a 24h | HR Before | HR at 24h | pH Before | pH at 24h | PAFI Before | PAFI at 24h | PCO2 Before | PCO2 at 24h | Outcome | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | 26 | 18 | 120 | 99 | 7.44 | 7.43 | 30 | 141 | 34 | 35 | Withdrawn (48h) |
| Patient 2 | 25 | 18 | 105 | 88 | 7.44 | 7.39 | 90 | 122 | 43 | 42 | Withdrawn (72h) |
| Patient 3 | 18 | 14 | 112 | 90 | 7.44 | 7.44 | 57 | 119 | 33 | 45 | Withdrawn (168h) |
BR: breathing rate; HFNC: High Flow Nasal Cannula Oxygen Therapy; HR: heart rate; PAFI: PaO2/FIO2 ratio; PCO2: CO2 partial pressure.
Patient 2 was an 85-year-old woman with a history of obesity, cardiac hypertension and Dana Point group 2 pulmonary hypertension, receiving home oxygen therapy. She was admitted for a clinical picture of fever, cough with greenish expectoration, increased basal dyspnea, and signs of decompensated heart failure. Treatment began with oxygen therapy using a Ventimask® face mask with an FIO2 of 50%, antibiotics, diuretics, nebulized bronchodilators, and systemic corticosteroid therapy. Twenty-four hours after admission, she continued to show increased work of breathing and developed hypoxemic respiratory failure (Table 1), so HFNC was introduced at an initial FIO2 of 100% and a flow of 50 lpm. The patient tolerated the device well, and reported greater comfort compared with the face mask (8/10 compared to 2/10, respectively) and an absence of mouth dryness. Her clinical progress and blood gas parameters were favorable, and the patient was switched to COT via nasal prongs 72hours later.
Patient 3 was a 74-year-old woman, former smoker, with a history of idiopathic pulmonary fibrosis. She had been diagnosed with lung cancer 7 months previously, treated with chemotherapy and radiation therapy. She was admitted for an episode of progressive dyspnea, until breathing difficulties were present at rest, in addition to fever and symptoms of lower respiratory tract infection. Treatment began with antibiotics, bronchodilators and a corticosteroid, plus concomitant oxygen therapy via a Ventimask® face mask at an initial FIO2 of 50%. Respiratory failure worsened, and the patient developed marked hypoxemic respiratory failure (Table 1) despite the use of a reservoir mask, so on day 8 of admission, HFNC was introduced, at an initial FIO2 of 95% and a flow of 40 lpm. The patient tolerated the device well, and reported greater comfort compared with the reservoir mask (9/10 compared to 1/10, respectively) and an absence of mouth dryness. The device was used for 7 days, after which the patient was switched to COT via nasal prongs.
In adults, HFNC has been studied in many situations, including bronchoscopies, weaning from intubation, patients who are not candidates for invasive ventilation, acute respiratory failure in emergency settings or intensive care, etc.1,2 However, this evidence is based largely on observational studies and case series. Lenglet et al.3 found a significant reduction in respiratory rate, less dyspnea on the Borg scale, and increased PaO2 in a group of patients with acute respiratory failure treated in an emergency department. The same group (Sztrymf et al.4) found similar results in patients with acute respiratory failure refractory to oxygen therapy in an intensive care unit.
Our patients tolerated the device better than conventional oxygen therapy. The heated humidification provided by the HFNC appears to improve patient comfort and tolerance, compared to face masks, as shown in recent studies.5 This may benefit patients with borderline respiratory capacity, whose hypoxemia levels can fall when the mask is removed for eating, drinking or expectorating. Comparative studies have focused on patients with hypoxemic respiratory failure, while excluding those with hypercapnic respiratory failure. Although the results from preliminary studies appear promising, with no significant increases in PCO2 or pH, the use of HFNC is not approved in these patients, so more research is needed.6
To conclude, we report our initial experience with the use of high-flow nasal cannula with heated humidification in an acute hospitalization unit. To date, most publications in adults have focused on emergency departments and intensive care units, but no data are available on the use of these devices in hospitalized patients.
Please cite this article as: Demelo-Rodríguez P, Olmedo Samperio M, Gaitán Tocora DG, Cano Ballesteros JC, Andueza Lillo JA. Oxigenoterapia de alto flujo con cánula nasal: estudio preliminar en pacientes hospitalizados. Arch Bronconeumol. 2015;51:657–659.