Organizing pneumonitis (OP) has been defined as secondary (SOP) if it is caused by external aggressions, such as infections, toxic substances, drugs, connective tissue diseases, or other processes, and primary, idiopathic or cryptogenic when no association with any other disease can been determined.1,2 The relationship between different infection types and the onset of OP is unknown.2,3
We report the case of a 75-year-old patient, former smoker (25 pack-years) for 30 years, with a history of arterial hypertension, atrial fibrillation and surgery for colonic polyps, receiving treatment with acenocumarol, digoxin and valsartan.
He presented with a 2-week history of cough, sputum expectoration, dyspnea on moderate exertion, fever, joint pain and general malaise. Chest radiograph revealed pulmonary infiltrates in the right and left lower lobes, so treatment was started with cefditoren 400mg/day and azithromycin 500mg/day for 7 days.
The patient developed pleuritic pain in the right hemithorax due to pleural effusion and his clinical symptoms persisted, so he was admitted to hospital. Physical examination showed temperature of 38.1°C, tachypnea and 93% oxyhemoglobin saturation while breathing ambient air (FiO2 21%). Pulmonary auscultation revealed rhonchi and crackles in the right lung base.
Laboratory tests on admission showed leukocytosis, 13900leukocytes/mm3 (80% neutrophils, 9% lymphocytes, 10% monocytes), 399000platelets/mm3 and ESR 111mm/h. Of particular note among the biochemistry parameters were: ALP 133IU/l, gamma-GT 231IU/l and CRP 140mg/l. Other liver tests, renal function, ions, lipids, total proteins, albumin, uric acid, thyroid hormones, procalcitonin, ACE, immunoglobulins and complement parameters were within normal limits.
Autoimmune assay was negative and no precipitins were detected in plasma for Aspergillus or bird proteins. Arterial blood gases on ambient air showed partial respiratory failure (pO2 59mmHg) and intradermal Mantoux reaction was negative.
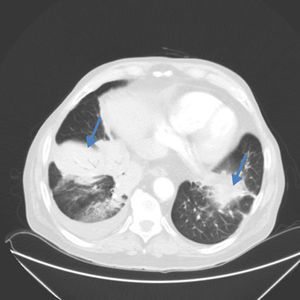
Chest computed tomography showed alveolar infiltrate with poorly defined borders, with the appearance of a polylobulated mass in the anterior segment of the right lower lobe and a solid nodule in the same lobe, measuring 25mm in diameter, associated with pleural effusion. Patchy infiltrates with areas of ground glass opacity were also seen in the lingula and left lower lobe (Fig. 1).
Thoracocentesis yielded 50cm3 of yellowish serous liquid with mixed cellularity consisting of mesothelial and polymorphonuclear cells and lymphocytes. pH was 7.44, concentration of protein in pleural fluid (3.6IU/l) and serum (6.3g/dl), glucose 125mg/dl and ADA 36IU/l with no evidence of acid-alcohol resistant bacilli or other microbes. Microbiological culture of the pleural fluid, including specific media for Koch's bacillus, were negative. Bronchoscopy was performed, revealing “saber-sheath” trachea and main bronchi with tendency to collapse, with no other significant findings.
After starting treatment with piperacillin and linezolid (for 6 days), fever resolved without radiological improvement, and the remaining symptoms persisted. Given the CT findings, a Tru-cut® needle biopsy was performed in the right lower lobe. The histological report was consistent with organizing pneumonia, and a non-caseifying granuloma with no AFB was also observed in the stain.
Pulmonary infiltrate and pleural effusion resolved within 3 days of starting treatment with methylprednisolone 40mg/day. After Mycobacterium tuberculosis was isolated in a bronchoalveolar lavage culture, antituberculostatics were started (etambutol/isoniazid/pyrazinamide/rifampicin), while corticosteroid dosing was maintained, leading to significant clinical improvement.
Huo et al. recently associated the presence of epithelioid cell granulomas or giant multinucleated cells in organizing pneumonia resections with an infectious etiology.4,5 Our patient had no history of exposure that might cause hypersensitivity pneumonitis. In contrast, the presence of consolidation with air bronchogram, a nodule and patchy infiltrates with multiple areas of ground glass opacity are common findings in organizing pneumonia, and although the infectious etiology could not be ruled out, series have been published in which organizing pneumonia occurs with pleural effusion in up to 20% of patients with focal lesions.
We can conclude from this clinical case that secondary organizing pneumonia should be considered in cases of persistent infiltrates despite antibiotic treatment (including antituberculous treatment).
Our thanks to Dr M. Marigil of the Anatomical Pathology Department and Dr E. Briz of the Respiratory Medicine Department of the Hospital San Jorge, Huesca.
Please cite this article as: Sander R, Gómez C, Borderías L. Neumonía organizada y tuberculosis pulmonar: coexistencia o enfermedad asociada. Arch Bronconeumol. 2016;52:570–571.