Meningeal carcinomatosis (MC) is the most serious neurological complication in lung cancer, and is relatively common, affecting approximately 5% of our patients, and around 20% according to some autopsy series.1
An oncogenic epidermal growth factor receptor (EGFR) mutation has recently been associated with a greater probability of developing MC2; the exon 19 deletion (del19) in particular appears to confer a higher risk of diffuse neurological dissemination.3 However, autopsy reports of patients with oncogenic mutations are rare.
We report an unusual case of a 54-year-old woman, non-smoker, with advanced adenocarcinoma (Fig. 1) with an EGFR del19 mutation who showed good tolerance and partial radiological response after 6 months of targeted treatment with erlotinib, an oral tyrosine kinase inhibitor (TKI).
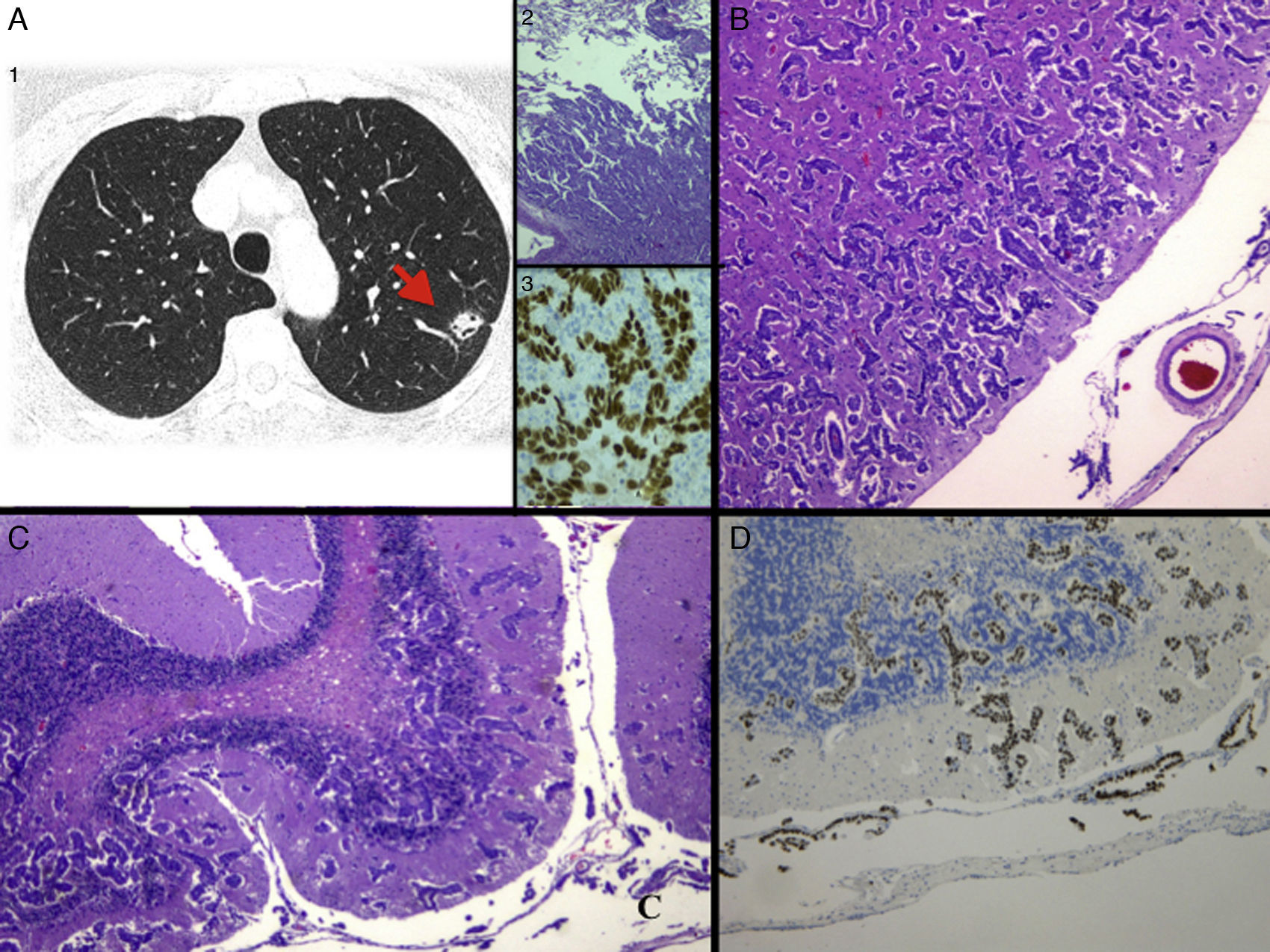
(A) 1: Chest computed tomography at diagnosis, showing a nodule in the left lower lobe suggestive of primary lung tumor; 2: histological image with hematoxylin–eosin (H&E) staining of the pulmonary nodule biopsy, consistent with adenocarcinoma (4×), and 3: immunohistochemistry staining positive for thyroid transcription factor 1 (TTF-1), confirming the primary pulmonary origin. (B) Histological image with H&E staining of MC with extensive deep invasion of the frontal cortex (2.5×) and (C) cerebellum (4×). (D) Staining positive for TTF-1, confirming infiltration by adenocarcinoma of pulmonary origin.
The patient was admitted with a neurological syndrome of dysarthria, instability and behavioral changes, but all laboratory, microbiology, cerebrospinal fluid (CSF), and radiological tests were normal. She rapidly progressed to coma, and died after 4 weeks.
Autopsy showed extensive progression in the form of meningeal carcinomatosis, with marked deep invasion of all the parenchyma of the cerebral (Fig. 1A), cerebellar (Fig. 1B) and medullar central nervous system (CNS) by lung adenocarcinoma (Fig. 1D), with a normal gross appearance. Curiously, no extracranial or spinal disease was observed. The molecular study showed the same EGFR del19 mutation originally diagnosed, sensitive to TKI, while the T790M mutation, conferring acquired resistance to TKI treatment4 was negative.
In MC, tumor cells infiltrate the leptomeninges and can disseminate throughout the craniospinal CNS via the CSF. Clinical manifestations are variable and no specific diagnostic tools are available. Cerebral magnetic resonance imaging can reveal meningeal enhancement and hydrocephaly, and malignant cells may be detected in the CSF. However, diagnosis tends to be late, when therapeutic options are limited.
Prognosis is extremely poor, and mean survival is from days to months, depending on the treatment of the underlying disease. Intrathecal chemotherapy, radiation therapy and “retreatment” with TKIs in patients with EGFR mutations have been proposed as palliative treatments, and survival can be prolonged in some selected cases.5
In our case, the patient showed extensive neurological progression in the form of invasive meningeal carcinomatosis, while maintaining an excellent systemic response, which could suggest insufficient penetration of the drug across the blood–brain barrier.
We believe that our case is interesting because it illustrates a particularly aggressive presentation of neurological progression in a patient with an EGFR del19 mutation, with dissociated response and diagnosis on autopsy.
Please cite this article as: Mezquita-Pérez L, Pian H, García N. Síndrome neurológico progresivo inusual en adenocarcinoma de pulmón epidermal growth factor receptor mutado: carcinomatosis meníngea invasiva, un diagnóstico de autopsia. Arch Bronconeumol. 2016;52:571–572.