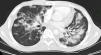
We report the case of 23-year-old man with human immunodeficiency virus (HIV) infection and a history of Kaposi sarcoma of the palate, treated with radiation therapy and antiretrovirals 2 years previously. He presented due to the appearance of violaceous skin lesions on the face, dyspnea and pleuritic pain with a CD4 T-lymphocyte count of 149cells/mm3 and viral load of 52092copies/ml. High resolution computed tomography of the chest (Fig. 1) revealed bilateral nodules with irregular margins and ground glass opacities, peribronchial cuffing and left pleural effusion. Bronchoscopy showed a raised lesion in the mucous membrane of the apical segment of the right upper lobe. Abundant hemosiderophages were found in the bronchoalveolar lavage (BAL) fluid, confirming alveolar hemorrhage. Immunohistochemistry was positive for human herpesvirus 8 (HHV-8). Treatment began with liposomal doxorubicin and antiretroviral treatment was switched. The patient remains alive at 8 months.
Kaposi sarcoma involving the lung occurs in 6%–32% of patients with acquired immunodeficiency syndrome (AIDS). It presents with skin lesions,1,2 and in 47%–75% of patients it is diagnosed post-mortem.3 Lesions can appear in the pulmonary parenchyma, bronchial tree, pleura, chest wall, and mediastinal lymph nodes,1,3 and CD4 T-lymphocyte count is generally <100cells/mm.3 In 80% of cases, death is a result of co-infection, due to cytomegalovirus, Mycobacterium avium complex, Pneumocistis jirovecii, bacterial pneumonia and herpes simplex infection.1
Chest computed tomography reveals poorly defined bilateral nodules, distributed symmetrically around the bronchial vessels (flame-like lesions). Other findings include septal peribronchial and interlobar cuffing, progressive air space consolidation and ground glass opacities.3
Lesions on the palate are a strong predictor for bronchopulmonary involvement.1 Typical lesions observed on bronchoscopy are red or violaceous cherry-like plaques in the bronchial Tree.1 HHV-8 is detected in BAL, which is highly specific (95%–98.9%) with variable sensitivity (58%–100%).
Occult alveolar hemorrhage has been described in HIV-positive patients with respiratory symptoms and abnormal radiological findings in the absence of hemoptysis. In 35.6% of cases, bronchopulmonary Kaposi sarcoma was detected, and of these 60.5% had occult alveolar hemorrhage.4
Vincent et al.5 subsequently characterized the following risk factors for AIDS-related alveolar hemorrhage: Kaposi sarcoma (OR: 5.3; 95% CI: 1.8–16.7; P=.003); cytomegalovirus pneumonia (OR: 9.8; 95% CI: 1–100; P=.05); hydrostatic pulmonary edema (OR: 16.4; 95% CI: 1.8–142; P=.01) and platelet count <60000 (OR: 5.6; 95% CI: 1.5–20; P=.009).
In conclusion, bronchoscopy is a useful tool for the diagnosis of occult alveolar hemorrhage in patients with HIV infection and respiratory symptoms.
FundingThis report received no type of funding.
Our thanks go to Drs Edgar Sánchez and Alfredo Saavedra, Internists and Pulmonologists from the Pulmonology Unit, Instituto Nacional de Cancerología, Universidad Nacional de Colombia.
We also thank Dr Sonia Cuervo, Infectologist from the Instituto Nacional de Cancerología, Bogotá, Colombia.
Please cite this article as: Martinez Ramirez I, Luquez AJ, Garcia Herreros P. Hemorragia alveolar oculta en paciente con sarcoma de Kaposi broncopulmonar. Arch Bronconeumol. 2015;51:364–365.