Oxygen therapy improves survival, quality of life, and exercise capacity in patients with chronic obstructive pulmonary disease (COPD) and severe respiratory failure at rest.1–3 Portable oxygen (O2) devices facilitate compliance with oxygen therapy and help avoid restrictions in physical activity. The SEPAR guidelines for oxygen therapy recommend that O2 flow be adjusted during stress testing to achieve a mean arterial oxyhemoglobin saturation (SpO2) of ≥90%.4 The 6-minute walk test (6MWT) is the method most widely used.5 Often, however, O2 is inappropriately adjusted for exercise, since it is a laborious process and can sometimes be contraindicated.6,7 Some countries recommend using the same O2 flow rate as that indicated at rest or recommend increasing O2 by an additional 1l.8
The aim of this study was to determine if the prescribed oxygen flow after titrating portable oxygen therapy for the 6MWT is similar to the flow that would be indicated if an additional liter were added to the prescribed O2.
We prospectively included all patients with chronic respiratory failure seen in the oxygen therapy clinic between October 2015 and September 2018 who were prescribed a continuous flow portable O2 device. They were in a stable phase, met criteria for home O2 therapy, had the autonomy to carry out activities outside the home, and were capable of performing a 6MWT.6 Patients who were prescribed a device with a valve were not included in the study.
O2 was initially adjusted to the at rest rate following SEPAR recommendations.4 At least 1 6MWT was then performed, using a WristOx2 pulse oximeter, Model 3150, with continuous flow O2 using the device that we considered most appropriate, depending on the estimated flow requirement and the patient's mobility and preferences. The 6MWTs were performed following SEPAR recommendations.6 If mean SpO2≥90% was not achieved in the first test, the test was repeated after a minimum rest period of 30min, increasing flow by 1l/min until the objective was achieved. We compared the flow rate after adjustment for the 6MWT with the flow that would be prescribed if 1l was added to the O2 at-rest flow rate.
The SPSS package version 20.0 was used for the statistical analysis. A descriptive analysis of patient characteristics was performed, and the Student's t-test was used for comparison of means. A p value<0.05 was considered statistically significant.
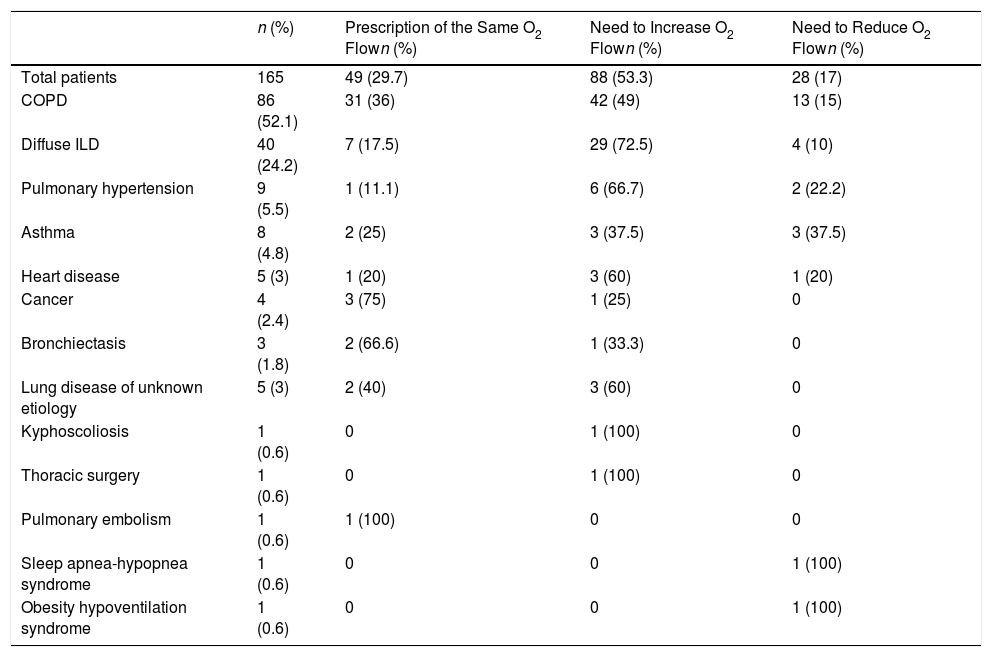
A total of 165 patients, 113 (68.5%) of whom were men, mean age 70.9 (SD 9.31) years, were included. Mean O2 flow prescribed for the portable device was 3.64 (SD 0.95) l/m. Seventy-seven patients (46.7%) used continuous flow concentrators and 88 (53.3%) had liquid O2 backpacks. After titration for the 6MWT, the prescribed O2 was only the same if 1l had been added to the resting O2 rate in 49 patients (29.7%) (p<0.0001). We increased the O2 flow rate in 88 patients (53.3%) and reduced it in 28 (17%). Table 1 shows the diseases causing chronic respiratory failure and the relationship between both methods for prescribing portable O2 flow. The prescriptions coincided in 36% of the COPD patients, but in only 17.5% of the interstitial diseases, and in 11% of the patients with pulmonary hypertension, in whom desaturation with exertion is greater. Twenty-one patients refused the liquid O2 backpack, despite requiring more than 3l/min. In 10 patients, desaturation experienced during the 6MWT could not be corrected.
Underlying Diseases of Patients and Comparison of the Prescribed Oxygen Flow, After Titrating Portable Oxygen Flow Using Both Methods.
| n (%) | Prescription of the Same O2 Flown (%) | Need to Increase O2 Flown (%) | Need to Reduce O2 Flown (%) | |
|---|---|---|---|---|
| Total patients | 165 | 49 (29.7) | 88 (53.3) | 28 (17) |
| COPD | 86 (52.1) | 31 (36) | 42 (49) | 13 (15) |
| Diffuse ILD | 40 (24.2) | 7 (17.5) | 29 (72.5) | 4 (10) |
| Pulmonary hypertension | 9 (5.5) | 1 (11.1) | 6 (66.7) | 2 (22.2) |
| Asthma | 8 (4.8) | 2 (25) | 3 (37.5) | 3 (37.5) |
| Heart disease | 5 (3) | 1 (20) | 3 (60) | 1 (20) |
| Cancer | 4 (2.4) | 3 (75) | 1 (25) | 0 |
| Bronchiectasis | 3 (1.8) | 2 (66.6) | 1 (33.3) | 0 |
| Lung disease of unknown etiology | 5 (3) | 2 (40) | 3 (60) | 0 |
| Kyphoscoliosis | 1 (0.6) | 0 | 1 (100) | 0 |
| Thoracic surgery | 1 (0.6) | 0 | 1 (100) | 0 |
| Pulmonary embolism | 1 (0.6) | 1 (100) | 0 | 0 |
| Sleep apnea-hypopnea syndrome | 1 (0.6) | 0 | 0 | 1 (100) |
| Obesity hypoventilation syndrome | 1 (0.6) | 0 | 0 | 1 (100) |
COPD: chronic obstructive pulmonary disease; IPD: interstitial lung disease.
The results show the superiority of titration by 6MWT over the alternative of adding 1l of O2 to the resting flow rate for correcting desaturation during activities of daily living. This is because with the latter, 53.3% of patients (72.5% and 66.7%, in the case of diffuse interstitial pulmonary disease and pulmonary hypertension, respectively) continue to desaturate during exertion. Patients with chronic respiratory failure who are stable often present prolonged periods of hypoxemia that are associated with reduced exercise tolerance and an increased rate of complications, such as pulmonary hypertension, right heart failure, and polycythemia.9 Arterial blood gas at rest is not useful for adjusting portable O2 flow.10 Stress tests, in contrast, allow us to assess the effectiveness of therapeutic interventions.5,11 The most widely used is the 6MWT,7 in its different modalities,6,12 though cycle ergometers have also been used to titrate O2.13
Other factors to bear in mind are the mobility profile of each patient, their preferences, and the mobility permitted by each of the O2 sources.14 Thus, 21 patients (12.7%) refused to change their device to a liquid O2 backpack, despite needing to increase their flow by more than 3l/min O2, because that would limit their autonomy.
At the present time, no portable devices are available that meet the needs of the more severe patients, as the liquid O2 backpack can only provide a flow of up to 5l/min. In fact, despite having liquid O2 backpacks providing 5l/min, 10 patients in our study experienced desaturation during the 6MWT that could not be corrected, with a mean sustained SpO2 of <90%.
In the future, an alternative to the current titration procedures may be to individualize the provision of home oxygen supply to each patient by integrating sensors in portable O2 devices that would measure SpO2 in real time and automatically adjust the flow of O2, according to patient needs.15
In summary, it currently seems necessary to titrate the portable O2 flow with a stress test if we want to adequately correct desaturation during exercise. Even so, this method has its limitations and is not the only factor to be taken into account when prescribing portable O2.
Please cite this article as: Lourido-Cebreiro T, González-Barcala FJ, Álvarez-Dobaño JM, Pereiro-Brea T, Abelleira-Paris R, Valdés L. Necesidad de titular el oxígeno portátil mediante pruebas de marcha de 6 minutos. Arch Bronconeumol. 2019;55:541–542.