Mycobacterium interjectum (M. interjectum) is a rare, nontuberculous mycobacterium, known to cause lymphadenitis cervicalis in young patients.1 We report a case of pulmonary disease.
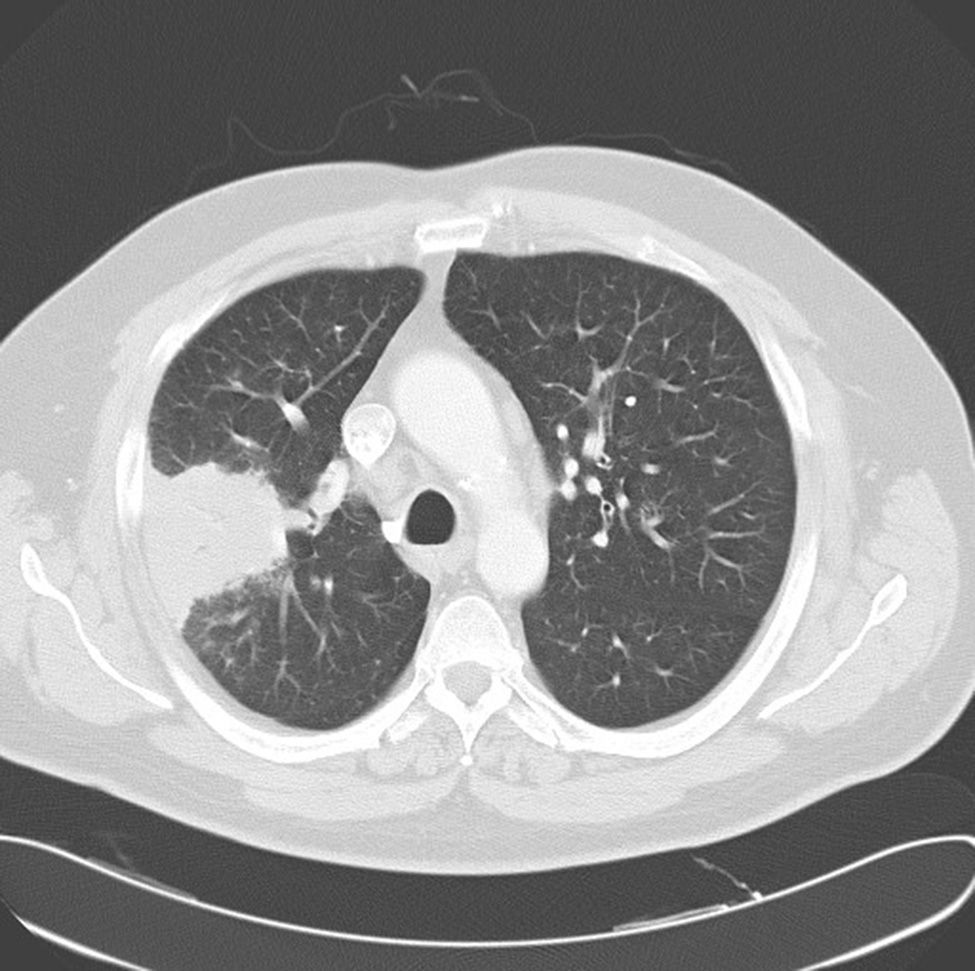
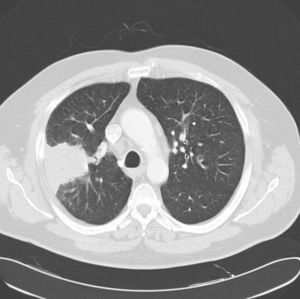
A 52-year-old man, active smoker, presented with a 15-day history of fever, general malaise and bloody expectoration. Isolated crepitating rales were heard on lung auscultation. Chest X-ray showed right upper lobe condensation and enlarged right hilum. Treatment with levofloxacin was prescribed, but improvement was limited, so a chest computed tomography (CT) was performed, revealing condensation with air bronchogram in the posterior segment of the right upper lobe (Fig. 1), and enlarged right hilar, retrocava-pretracheal and prevascular lymph nodes. Bronchoscopy was performed: gross results were normal, and cytology and bacilloscopic results from bronchial aspirate were also normal. CT-guided core biopsy of the lung was conducted, and histologic analysis of the specimen showed granulomas with multinucleated giant cells and epithelioid cell histiocytes, some of which had central necrosis. Treatment began with isoniazid, rifampicin, pyrazinamide and ethambutol. Mycobacteria were subsequently isolated from the culture of the bronchial aspirate; these were identified as M. interjectum using DNA technology based on inverse hybridization of PCR products targeting the 23S rRNA gene (GenoType®Mycobacterium CM). The patient's progress was satisfactory and, 2 months later, cultures were negative for mycobacteria. Pyrazinamide and ethambutol were withdrawn, while isoniazid and rifampicin administration continued for 1 year. At that time, the patient remained asymptomatic, with fibrous scarring and infiltration in the right upper lobe on chest X-ray. Currently, 20 months later, he is stable with no signs of disease reactivation.
Only three cases of lung involvement with M. interjectum have been reported in the literature.2–4 All three were cases of cavitary disease in which M. interjectum was later isolated. The strains were resistant to isoniazid, rifampicin, pyrazinamide3 and ethambutol,3,4 although one patient3 initially responded well to standard antituberculosis treatment. Nevertheless, 18 months later, symptoms and radiological progression recurred, and a nontuberculous mycobacteria with the same resistance profile as before was isolated.
In contrast to the above-mentioned cases, our patient did not have cavitary disease, and response to first-line antituberculosis drugs was good, despite rifampicin and ethambutol resistance found on antimicrobial sensitivity testing. In view of the good clinical progress after identification of the mycobacteria, an antibiogram was felt to be unnecessary, and this may be considered as a limitation of our report. However, discrepancies between in vitro and in vivo resistance data raise questions regarding the real significance of in vitro resistance in certain situations. This issue and the long follow-up period add to the value of the experience reported.
To conclude, M. interjectum is a very unusual cause of lung disease. Once diagnosed, treatment with a standard antituberculosis regimen may be attempted.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: Villanueva MÁ, Gullón JA, Álvarez-Navascués F. Enfermedad pulmonar por Mycobacterium interjectum: a propósito de un caso. Arch Bronconeumol. 2015;51:155–156.