New lung cancer staging techniques, such as transcervical extended mediastinal lymphadenectomy (TEMLA) and video-assisted mediastinal lymphadenectomy (VAMLA), provide sensitivity and specificity figures of close to 100%, thanks to the extensive nature of the procedure and the large amounts of lymph node collected. On the other hand, these techniques are highly invasive and their benefits have been questioned.1 Our surgical team only performs TEMLA in 2 types of patients: operable patients with N0-1 lymph node staging and a high prevalence of N2 disease, to avoid false negatives on mediastinoscopy; or in patients with a high comorbidity burden, to avoid high-risk thoracotomy in patients for whom this intervention would not benefit survival if they turn out to have N2 disease. We report the case of a patient subjected to TEMLA staging who developed incisional metastasis. This is the first report of this kind in the medical literature.
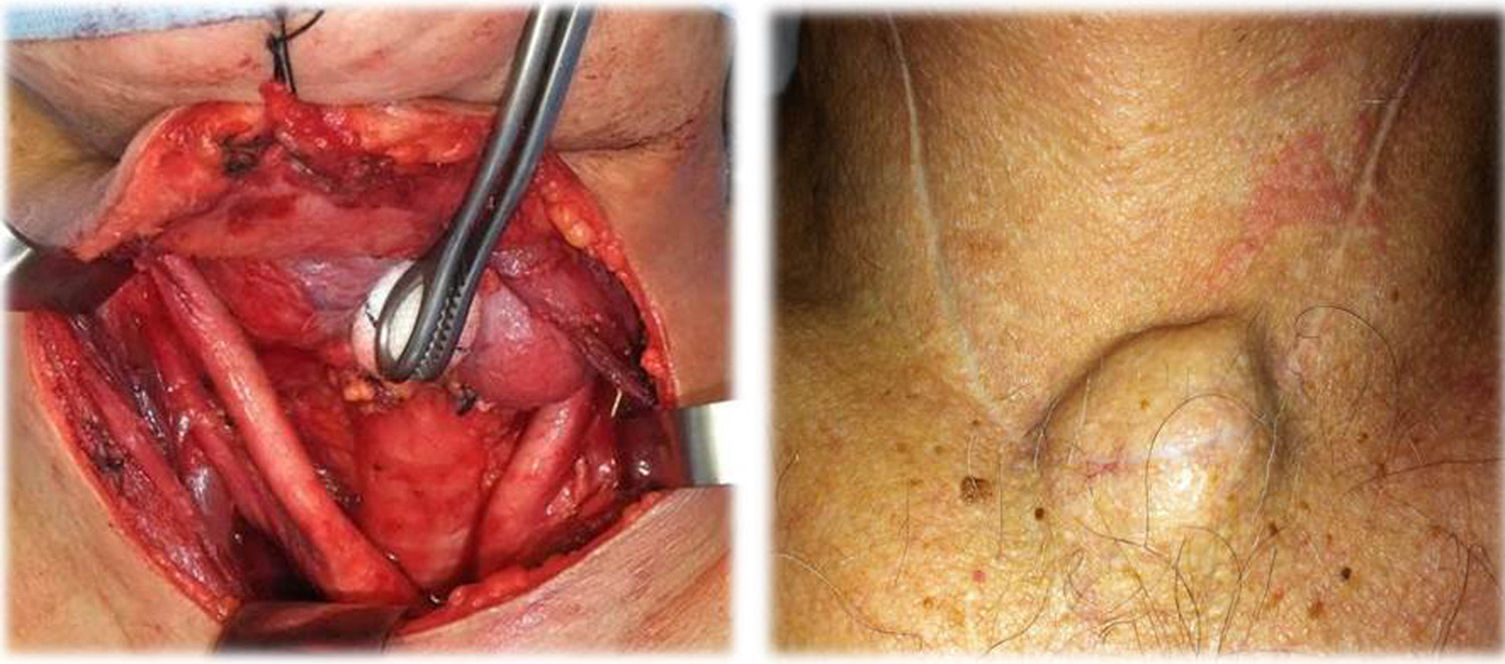
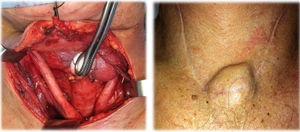
A 72-year-old man presented with multiple comorbidities, including left hilar lung cancer, 55mm×56mm with undetermined station 4R and 6 lymph nodes. TEMLA was used to obtain 28 nodes from stations 1+3, 2R/L, 4R/L 5, 6, 7 and 10R/L (Mountain–Dresler classification). Disease was confirmed in multiple stations, with malignancy in stations 10L, 5 and 6. Rescue surgery was indicated after induction chemotherapy, but the patient was finally deemed inoperable due to intrapericardial arterial infiltration. Three months later, he developed a tumor in the site of the TEMLA scar, which was resected with local anesthesia (Fig. 1). Histological examination confirmed metastasis of the primary tumor. The patient died due to progressive disease 23 months later.
Recurrence of lung cancer in surgical wounds is very rare, although reports have been published of implants in surgical wounds following open lung resection or thoracoscopy, and in mediastinoscopy incisions. The low prevalence of recurrence makes it difficult to determine if the primary cancer cell type or degree of differentiation is associated with the incidence of this type of relapse.2 With regard to incisional recurrence in surgical scars after staging, the meta-analysis published by Ashbaugh in 1970 estimated that implants in the mediastinal incision occur in 0.12% of procedures3; the incidence of this type of lesion after maximal staging techniques is unknown – indeed, no case has been reported to date. The greater invasiveness (Fig. 1) and volume of lymph node obtained in TEMLA – both factors impacting on the genesis of incisional metastasis – prevent any assumption that the incidence of incisional metastasis is comparable to mediastinoscopy.
The detection of the first case of metastasis in a TEMLA scar sets the rate of incisional metastasis in our patient series at 0.09%.
The etiology and pathogenesis of these lesions are still to be clarified, but related factors include lymph node or hematogenetic dissemination to the hypervascularized wound – which would occur in disseminated stage disease – and the local shedding and implantation of malignant cells,4 in which case the staging defined in the primary staging would not be affected, and long-term survival would remain a possibility.5 In our specific case, the patient's extended survival supports the second of the above-mentioned etiopathological mechanisms.
Please cite this article as: Pérez-Alonso D, Hernández-Escobar F, López-Rivero L. Metástasis incisional de carcinoma broncogénico tras linfadenectomía mediastínica transcervical extendida. Arch Bronconeumol. 2016;52:276–277.