Exogenous lipoid pneumonia (ELP) is a rare (incidence 1.0%–2.5%), often under-diagnosed disease, caused by the aspiration and accumulation of exogenous lipids within the pulmonary alveoli. Various cases have been described due to inhalation of lubricants via the nasal passages and oropharynx, aspiration of mineral oils in laxatives in patients with eating disorders, application of lip gloss, occupational exposure to liquid paraffin or mineral oils (“fire-eaters”, industrial use in washing of machinery, automobile workshops, plastic paints, etc.) and application of Vaseline during the insertion of nasogastric tubes and in the care of tracheotomy patients.
ELP usually presents radiologically as areas of low-attenuation peribronchial consolidation and ground glass opacities, with a predominantly bibasal distribution. We present 5 cases of long-standing laryngectomy patients diagnosed with ELP who admitted using Vaseline in their tracheal stoma care.
La neumonía lipoidea exógena (NLE) es una patología inusual (incidencia del 1-2,5%), frecuentemente infradiagnosticada, causada por la aspiración y la acumulación de lípidos de origen exógeno dentro de los alvéolos pulmonares. Se han descrito casos por inhalación de lubricantes en fosas nasales y orofaringe, aspiración de aceites minerales contenidos en laxantes en pacientes con trastornos alimentarios, aplicación de brillo de labios, exposición profesional a parafina líquida o aceites minerales («comedores de fuego», uso industrial en lavado de maquinaria, talleres de automóviles, pinturas plásticas, etc.) y aplicación de vaselina en la inserción de sondas nasogástricas y en el cuidado de traqueotomías en pacientes traqueotomizados.
Radiológicamente la NLE suele presentarse como consolidaciones peribronquiales de baja atenuación y opacidades en vidrio deslustrado con una distribución preferentemente bibasal. Presentamos 5 casos de pacientes laringectomizados de larga evolución con diagnóstico de NLE que admitían el uso de vaselina en el cuidado del estoma traqueal.
Exogenous lipoid pneumonia (ELP) is a rare disease, caused when oily substances are aspirated and deposited in the alveoli.1
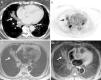
The most common radiological findings in ELP are ground glass opacities or peribronchial consolidations, mainly in the lower lung fields. Typical computed tomography (CT) findings include areas of fat attenuation, while on magnetic resonance imaging (MRI), the signal intensity for ELP in the various sequences is similar to that of fatty tissue. When accompanied by consistent clinical symptoms, these imaging study findings can determine a diagnosis of ELP.2
There are very few reports in the literature of ELP due to inhalation of lubricants used in cannula care in tracheotomy patients. We report 5 cases of ELP in patients with tracheotomy using Vaseline for the lubrication and insertion of cannulas.
Clinical ReportCase 1An asymptomatic 81-year-old woman, non-smoker, with a personal history of tracheotomy for recurring bilateral paralysis after thyroid surgery in 2000. On a preoperative chest X-ray, the chance finding of an image consistent with a mass in the left lung base was revealed.
Consolidation, ground glass opacities and a focus of fat density were seen in the left lower lobe (LLL) on chest CT (Fig. 1).
Bronchoscopy and tumor markers were negative for malignancy. Bronchoalveolar lavage (BAL) fluid analysis revealed lipid-loaded macrophages.
The patient reported daily use of liquid Vaseline to facilitate changing and placing her tracheotomy cannulas. After discontinuing this practice, partial resolution of the opacity described was seen on radiological follow-up X-ray at 3 months.
Case 2An asymptomatic 67-year-old woman, former smoker, tracheotomized for squamous cell carcinoma in 2004 after treatment with supraglottal laryngectomy and radiation therapy. Chest X-ray showed right basal consolidation.
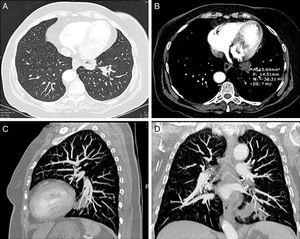
In view of the patient's history of cancer, a positron emission tomography (PET)/CT was performed. In the PET component, hypermetabolic areas were observed in the areas of lung consolidation. Parenchymal opacities with fat attenuation were observed in the CT component, so a presumed diagnosis of lipoid pneumonia was given. Since the patient refused a fiber bronchoscopy, the opacity was studied with a chest MRI that revealed hyperintensities in T1-weighted sequences, which were suppressed in fat suppression sequences (e.g. the STIR sequence) (Fig. 2). These findings were consistent with ELP.
Computed tomography (CT) axial image of the mediastinum (A) showing peribronchial opacity in the right lung with areas of fat attenuation (arrow). Positron emission tomography image (B), showing hypermetabolic areas in the right lung base, coinciding with the opacities seen on the CT (arrow). Axial magnetic resonance images, showing signal hyperintensity of the opacity in T1-weighted sequences (C) and signal suppression in the fat saturation sequence (D) (arrows).
The patient stopped using Vaseline for tracheotomy cannula care and received low dose corticosteroids. Six months later, complete radiological resolution of the opacity was confirmed.
Case 3A 57-year-old man, former smoker, with a clinical history of tracheotomy in 2005 due to long-term orotracheal intubation. The patient was admitted to our hospital for aspiration pneumonia. After receiving antibiotic therapy, he improved clinically and the consolidation resolved. Nevertheless, treatment-refractory left basal opacity with characteristic foci of fat attenuation on CT persisted. These findings led to the diagnosis of ELP.
Intraluminal mucous plugging was observed on bronchoscopy.
Case 4A 60-year-old male, former smoker with COPD, chronic bronchitis phenotype, and history of supraglottal, squamous cell carcinoma, treated in 2004 with total laryngectomy, radiation treatment and chemotherapy. The patient subsequently presented local and distant progressive disease (lung metastases).
The patient had a series of hospital admissions due to repeated pneumonia with clinical improvement after antibiotic treatment. In successive radiological check-ups, the lung opacities had resolved, although a pseudonodular image (3mm) with a focus of fat attenuation persisted in LLL, consistent with ELP.
No malignant findings were seen on bronchoscopy, and only traces of fibrin were seen in the LLL bronchus.
Case 5A 53-year-old man, former smoker, with chronic bronchitis phenotype COPD, treated for squamous cell carcinoma in 2004 with laryngectomy, radiation therapy and chemotherapy. In May 2013, a 16mm pulmonary nodule obstructing the bronchial lumen was observed in the right lower lobe (RLL). Alveolar opacities with areas of fat attenuation were also seen in the lower parts of the middle lobe and LLL, consistent with ELP in a tracheotomy patient. PET/CT showed uptake suggestive of malignancy in the area of the RLL nodule. Lipophages were seen in BAL fluid. Fiberoptic bronchoscopy biopsy results confirmed mucous membrane invasion by squamous cell carcinoma. The patient was not considered a candidate for surgery, so was referred to the oncology radiotherapy unit for treatment.
DiscussionLipoid pneumonia is a rare disease, defined by the presence of intraalveolar lipids, classified as exogenous or endogenous.1–6
Exogenous lipoid pneumonia (ELP) is a very rare form of lipoid pneumonia caused by the aspiration of oily products (nostril lubricants, Vaseline, lip gloss, paraffin, etc.). It can be chronic, when associated with recurrent aspiration, or acute, when caused by the accidental aspiration of a large amount of oily substances.
From a clinical point of view, the chronic variant of ELP is often asymptomatic or presents with generalized symptoms. In our series, most patients were asymptomatic. The most common symptom was unproductive chronic cough (Table 1).
Clinical and Radiological Characteristics of the Patients.
| Age/sex | Time since laryngectomy | X-ray | CT | PET | MRI | FBC/BAL | Progress | Site | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 81/F | 13 years | Mass LLL | Consolidation with fatty density+ground glass opacity | – | – | Negative for malignant cells/lipophages | Partial resolution of opacity after discontinuation of Vaseline | LLL |
| 2 | 67/F | 9 years | Opacity in RLL | Areas of fat attenuation in RLL | ↑FDG | T1 hyperintensity suppressed in STIR | Not done | Complete resolution after discontinuation+corticosteroid | RLL |
| 3 | 57/M | 8 years | Opacity in LLL | Left basal opacity with fat attenuation hotspot | – | – | Mucous plugs/inflammatory cells | Not done (change of hospital) | LLL |
| 4 | 60/M | 10 years | Nodule in LLL | Pseudonodule in LLL | – | – | Fibrin traces/inflammatory cells | Death due to disease progression | LLL |
| 5 | 53/M | 10 years | Opacities in both bases | Peribronchial hypodense opacities in both bases | – | – | Chronic inflammatory changes/lipophages | Complete resolution | LLL and ML |
CT, computed tomography; F, female; FBC/BAL, fiberoptic bronchoscopy/bronchoalveolar lavage; LLL, left lower lobe; M, male; ML, middle lobe; MRI, magnetic resonance imaging; PET, positron emission tomography; RLL, right lower lobe.
Chest CT findings in ELP have been described in several articles, the most common being consolidations and areas of peribronchial ground glass opacities, mainly in the lung bases.1,2,6 Attenuation of these consolidations is typically in the range of fatty tissue (−200 to −100HU). According to some authors,2 this finding, when accompanied by consistent clinical symptoms, may be sufficient for determining a diagnosis of lipoid pneumonia. Other less common radiological findings include crazy paving pattern (a linear pattern superimposed on a ground glass opacity) in the lung parenchyma, endobronchial secretions or unspecific areas of post-obstructive pneumonitis.7,8 In our series, the most common radiological finding was poorly defined opacities with areas of fat density on CT (Table 1).
As this entity can appear in the form of nodules or masses, differential ELP diagnosis must rule out malignancy. For this reason, some patients undergo complementary diagnostic tests such as PET/CT. ELP may be associated with unspecific increase in FDG uptake due to concomitant inflammatory changes, so morphological findings on CT must be taken into consideration when interpreting these examinations to avoid false positives.2,9,10
Although MRI is not a technique of choice for evaluating pulmonary parenchyma, it can be useful in the diagnosis of ELP, since it shows the fat content of lesions in T1-weighted sequences and signal suppression in fat suppression sequences (e.g., STIR).2 The second patient in our series refused bronchoscopy, so MRI was used to complete the assessment, and was found to be useful for confirming the fat content in the opacity seen on CT.
Proof of lipophages (vacuolated lipid-loaded macrophages) in sputum, transthoracic fine-needle aspirate, transbronchial biopsy and/or BAL is usually required for a definitive diagnosis of ELP, and the number of vacuolated alveolar macrophages generally correlates well with the severity of the disease.3,5 In other studies, BAL has been shown to be an effective treatment option, as it rinses the oily substances from the lung parenchyma, thus preventing the formation of fibrosis.
No other series with so many laryngectomy patients in a single hospital was identified, even after an exhaustive review of the literature. The 5 cases presented (Table 1) share the common factor of use of oily products (Vaseline) for the care and lubrication of tracheotomy cannulas. All cases shows fat attenuation images on CT, highly suggestive of lipoid pneumonia.
Radiological differential diagnoses of lesions with fat content include metastatic liposarcoma or hamartoma, although the radiological characteristics differ from those of ELP.10
When these cases of ELP were detected, we contacted the Tracheotomy Unit of the ENT Department of our hospital to discuss the findings and their relationship with the use of Vaseline as a lubricant for tracheotomy cannulas. On the basis of our clinical and radiological data, we recommended that, to avoid aspiration, liposoluble lubricants (such as Vaseline) should not be used for the daily care of the tracheal stoma in laryngectomy patients.
In our opinion, radiological findings (standard X-ray, CT, MRI and/or PET/CT) in patients with consistent clinical symptoms should provide sufficiently reliable data for determining a diagnosis of lipoid pneumonia. In some cases, radiological testing may be sufficient and invasive testing procedures can be avoided.
Please cite this article as: García Latorre R, Rodríguez Díaz R, Barrios Barreto D, Ayala Carbonero A, García Gómez-Muriel MI, Gorospe Sarasúa L. Hallazgos radiológicos de la neumonía lipoidea exógena en pacientes laringectomizados. Arch Bronconeumol. 2015;51:e36–e39.