Primary pleural tumors are uncommon, accounting for 3%–3.5% of all chest tumors.1 They most frequently appear as malignant pleural mesothelioma, and occur more often in men (ratio 4:1), with incidence peaking between the ages of 50 and 70 years.2 In more than 80% of cases, there is a clear relationship between direct (occupational exposure) and indirect (non-occupational) exposure to asbestos fibers. Environmental exposure has also been described, and the risk is higher in Greece, Cyprus, Turkey and Corsica.1,2
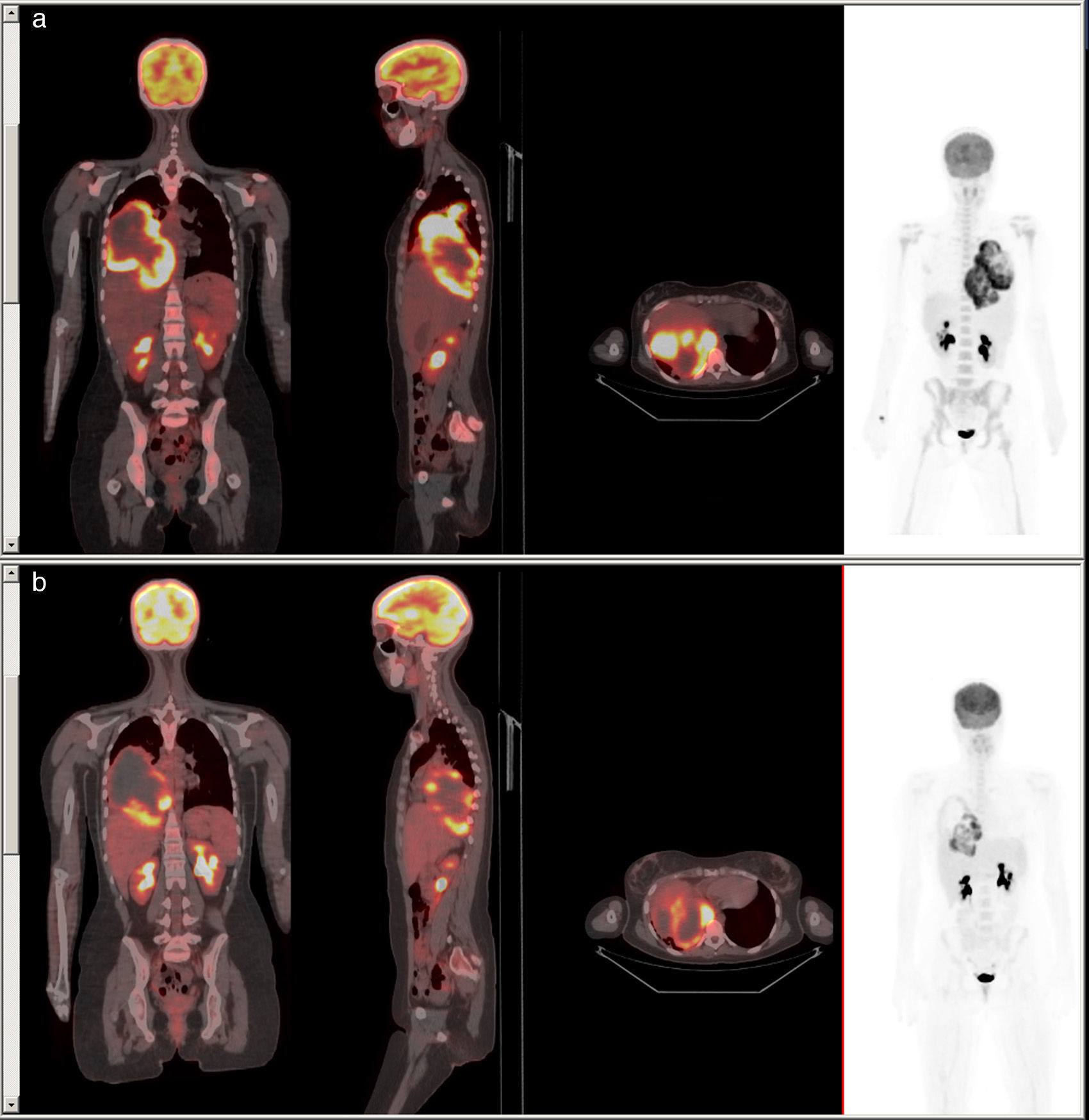
We report the case of a 22-year-old woman with no personal or family history of asbestos contact, who reported a 10-month history of right scapular pain with no other clinical complaints. Around 2 months before presenting, she developed a cyclic febrile pattern, lasting 1 week, coinciding with her menstrual cycles, along with dyspnea on exertion. She was admitted with a suspected diagnosis of pelvic inflammatory disease. Leukocytosis with significant thrombocytosis and CRP 137 were determined, and empirical treatment began with ampicillin and gentamycin, but no improvement was observed. A chest radiograph and chest-abdominal computed tomography (CT) were performed, showing a large right-sided paravertebral mass occupying almost all the ipsilateral hemithorax. The PET-CT with 18F-FDG revealed a hypermetabolic mass in the right hemithorax, suggestive of malignancy, and diffuse increased reactive uptake in the bone marrow (Fig. 1a). Biopsy found undifferentiated carcinoma in the posterior mediastinum, suggestive of right pleural mesothelioma.
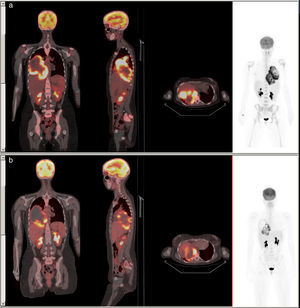
Coronal, sagittal and axial slices of PET-CT fusion imaging. (a) A large mass is observed occupying almost all the right hemithorax, with heterogeneous density and highly intense peripheral uptake (SUVmax=18.9), in contact with the parietal pleura, posterior mediastinum and right hilum. (b) Reduced metabolic uptake (SUVmax=16.8) seen after chemotherapy.
Neoadjuvant chemotherapy was started, and some response was seen. Post-treatment PET-CT showed a reduced tumor size with peripheral metabolic uptake (Fig. 1b).
The case was discussed with the oncological committee and surgical intervention was scheduled. Right pneumonectomy extending to the diaphragm and pericardium was performed, and the pathology report described a deciduoid variant of epithelioid mesothelioma in the right lung, parietal and visceral pleura, pericardium, diaphragmatic muscle, and the diaphragm.
Malignant pleural mesothelioma is a highly aggressive tumor, with a latency period of 20–30 years between exposure and disease onset, making it difficult to identify the “cause–effect” relationship,1 and most cases are diagnosed in advanced phases.
PET-CT is useful for correctly differentiating between benign and malignant disease and for quantifying the metabolic activity of the lesion, the presence of metastases, and for evaluating response to treatment.3 Sensitivity is greater than 90% and the negative predictive value is 96%.1,3 Semiquantitative evaluation of FDG-PET tumor uptake, histological subtype, mediastinal lymphadenopathies and extrathoracic metastases are prognostic markers.2
In recent years, biomarkers for early diagnosis have emerged, including soluble mesothelin in pleural fluid and fibulin-3 in plasma.4,5 Currently, microRNA gene expression associated with mesothelioma oncogenesis is under study, and this may be of use as a potential biomarker in the near future.4
Remarkable features of our case include the patient's young age and the absence of factors directly related with the genesis of mesothelioma, even after a thorough clinical investigation. Asbestos, comprising 2 natural types of silicates (serpentine and amphiboles), is the main etiological agent. Certain professions incur more risk of developing this tumor, and the risk extends not only to exposed workers but also their family members.1 Other known risk factors include the SV-40 virus (a potent oncogenic DNA virus) and post-radiation of malignant tumors such as Hodgkin's lymphoma, or breast or lung cancer.1,2
The absence in our patient of factors associated with malignant pleura mesothelioma and other reports of this entity in children suggest that there may be other etiological factors as yet undiscovered.
Please cite this article as: Espinosa Muñoz E, Ramírez Ocaña D, Gutiérrez Cardo AL. Mesotelioma pleural maligno en adulto joven sin exposición conocida al asbesto. Arch Bronconeumol. 2016;52:615–616.