Treatment with all-trans-retinoic acid (ATRA) induces myeloid differentiation among leukemia cells in acute promyelocytic leukemia (APL). The differentiation syndrome (DS) or ATRA syndrome occurs in up to 25% of APL patients treated with ATRA, due to an inflammatory reaction accompanied by an increase in capillary permeability. It is characterized by breathing difficulties, fever, pulmonary infiltrates, pleuro-pericardial effusion, kidney failure, and hypotension.1
We report the case of a 45-year-old man with a diagnosis of APL, under treatment with ATRA (45mg/m2) and idarubicin (12mg/m2), who developed fever and dyspnea hours after suspending prophylactic treatment with intravenous dexamethasone. Pulmonary auscultation revealed bilateral crackles. Chest radiograph showed a suspicious increase in density in the right lower lobe. The patient's situation was complicated by oxacillin-sensitive Staphylococcus aureus bacteremia, due to an infected catheter, which was treated with piperacillin-tazobactam and vancomycin.
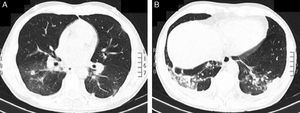
As no clinical improvement was observed, a chest computed axial tomography was requested, showing bilateral nodules and ground glass densities, mainly in the lower lobes. An area of parenchymal consolidation and associated pleural effusion was identified in the left lower lobe (LLL) (Fig. 1A and B). Bronchoalveolar lavage was performed and microbiological cultures were negative. Treatment was started with intravenous dexamethasone (10mg/12h), showing favorable progress and complete resolution of the bilateral pulmonary infiltrate in less than 48h. A diagnosis was given of DS due to ATRA treatment.
The introduction of ATRA in the treatment of APL has been one of the most significant advances in the management of hematological cancers. APL is now the most curable form of adult myeloid leukemia, with full remission persisting at 5 years and 70%–80% survival.2 However DS associated with ATRA administration is probably the most toxic adverse event. The prophylactic use and length of administration of corticosteroids are controversial. Our patient received prophylactic treatment with intravenous dexamethasone, but even so, developed the syndrome. The latest PETHEMA protocol recommends prophylaxis in all patients receiving >5×109l−1 for 15 days. DS mortality is currently low (1%), due to early treatment with corticosteroids, along with the concomitant use of chemotherapy in combination with ATRA.3
DS is a clinical diagnosis based on a group of signs and symptoms in APL patients receiving induction treatment with ATRA or arsenic trioxide. Three or more of the following findings are sufficient for diagnosis and starting treatment with glucocorticoids, if other causes have been previously ruled out: fever, weight gain, respiratory distress, pulmonary infiltrates, pleural and/or pericardial effusion and/or renal failure.3
Treatment should be initiated with intravenous dexamethasone (10mg/12h) as soon as the syndrome is suspected. Corticosteroid treatment should continue until the syndrome has resolved, followed by gradual dose tapering over the subsequent weeks.4
In conclusion, DS is a relatively common serious complication in APL patients, and the time of presentation varies widely. Take-home messages: (1) suspect DS in APL patients receiving ATRA and/or arsenic trioxide; (2) detect early signs of DS to confirm clinical diagnosis; and (3) examine the patient's behavior for rapid detection and treatment of complications.
Please cite this article as: Ariza-Prota M, Pando-Sandoval A, García-Clemente M. Afectación pulmonar por ácido transretinoico en el tratamiento de la leucemia promielocítica aguda. Arch Bronconeumol. 2016;52:441–442.