We report a series of 6 cases, 4 women and 2 men, with a median age of 57 years, all of whom had comorbidities involving immunosuppression. They were admitted with respiratory symptoms and a chest X-ray with pulmonary infiltrates consistent with bacterial pneumonia. Empirical antibiotic treatment was administered in all cases. No response was obtained, patients deteriorated progressively, and cultures were negative.
Case 1: An 18-year-old female patient was referred from an urban area with a diagnosis of left pleural empyema. A simple chest CT scan revealed infected pulmonary sequestration in the left lower lobe. A left lower lobectomy was performed by lateral thoracotomy, without complications. An examination of the surgical piece detected Lophomonas blattarum infection (Fig. 1), so treatment began with metronidazole. The patient’s postoperative progress was favorable and she was discharged on the fifth day with complete resolution of her respiratory symptoms.
Case 2: A 52-year-old male patient from a rural area with a history of chronic renal failure was admitted with severe acute respiratory failure. Complete blood count and chest X-ray were performed, and were consistent with community-acquired pneumonia (CAP). He received empirical antibiotic treatment and oxygen therapy but showed no improvement. In view of the lack of response, bronchoscopy was performed and samples were collected. A direct study showed flagellated parasites and intravenous metronidazole began, with great improvement. The patient completed 20 days of home treatment, with complete resolution.
Case 3: A 55-year-old male patient from an urban area with a history of pulmonary tuberculosis treated with isoniazid and rifampicin was admitted for severe respiratory failure requiring orotracheal intubation. Due to a high suspicion of superinfection, empirical antibiotic therapy began, but given the lack of response, bronchoscopy was performed and direct examination of the sample showed a flagellated protozoan (Lophomonas blattarum). Treatment began with intravenous metronidazole, and the patient improved progressively. He remained in hospital until 7 days of intravenous treatment were completed and was discharged with oral metronidazole. He remains in good condition.
Case 4: A 59-year-old female patient from a rural area, with a history of renal cell carcinoma in remission, was admitted with a severe respiratory process. Chest CT was consistent with CAP, so empirical antibiotic therapy began, with partial improvement. Direct examination of sputum revealed flagellated parasites (Lophomonas blattarum), so treatment was supplemented with oral metronidazole. The patient improved quickly and was discharged to complete the regimen at home.
Case 5: A 69-year-old female patient from a rural area, with a history of chronic renal failure receiving dialysis, was admitted for respiratory symptoms. Chest CT and complete blood count were consistent with severe pneumonia, so she started empirical antibiotic therapy, without improvement. Samples were obtained by bronchoscopy and direct examination showed Lophomonas blattarum. Treatment started with intravenous metronidazole, and the patient showed gradual improvement.
Case 6: A 79-year-old female patient from a rural area, with a history of diabetes mellitus receiving treatment with insulin, was admitted for severe respiratory failure requiring orotracheal intubation. Results of the additional examinations including complete blood count and chest CT led to a diagnosis of severe pneumonia. Management began with empirical antibiotic therapy, with no response and gradual deterioration. A bronchoscopy was performed in which infection with Lophomonas blattarum was detected, so treatment with intravenous metronidazole started without improvement. The patient deteriorated progressively and died on day 10.
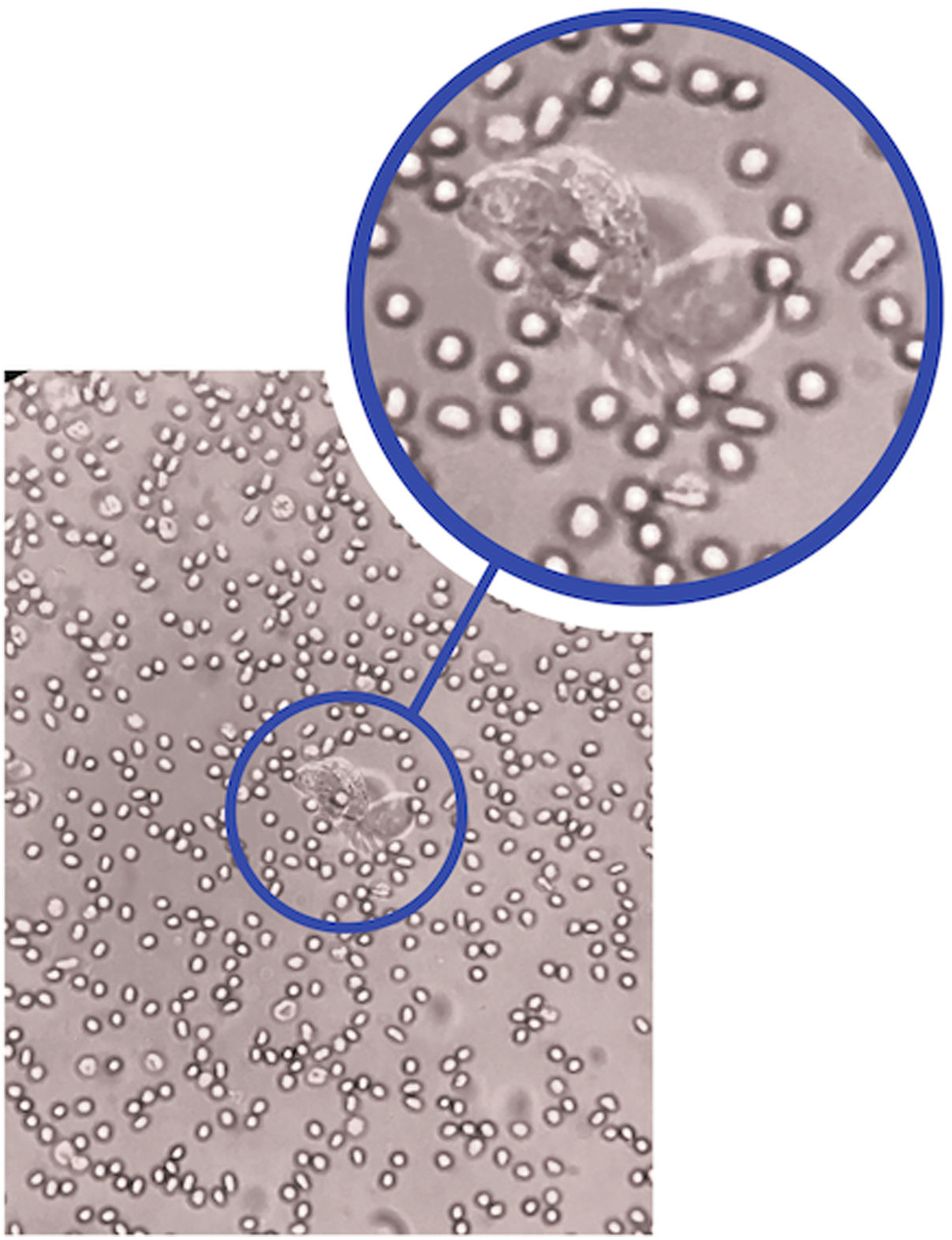
The species Lophomonas blattarum is a round, oval, or pyriform protozoan, 20−60 mm long and 12−20 mm wide. It has a granular cytoplasm, and its apical pole has irregular flagellae which vibrate to help it move. These parasites are found in the intestinal tract of some termites and cockroaches, while infection in humans is rare and closely related to states of chronic immunosuppression. The form of transmission is by direct ingestion of the feces of an infected termite or cockroach. The symptoms mimic a respiratory infection and can include cough with or without expectoration, chest pain, respiratory failure, etc., and bilateral pulmonary infiltrates on chest X-ray, so it is commonly confused with pneumonia. Diagnosis is confirmed by the identification of the parasite in respiratory secretions1–3.
Few cases of lung infection with Lophomonas blattarum have been reported in the literature: most are from China, where 137 cases have been reported to date, while 6, 2, 1, and 1 cases have been reported in Peru, Spain, Mexico and the Arab Emirates, respectively. In previous series, most patients are male, while women predominate in ours. Almost all are adults (3 children in Peru and 1 in Mexico) and are immunocompromised (69.1% in the literature vs. 100% in our study) or have previous or concomitant lung infections, similar to the situation presented in our series4–13.
In all patients, both in the existing literature and in our series, the symptoms presented are typical of a respiratory infection (cough, expectoration, fever, chest pain), with a chest X-ray suggestive of pneumonia, so it is often confused with this disease. Diagnosis is based on the direct live observation of the parasite in sputum, bronchoalveolar lavage, bronchial brushing or tracheal aspirate. Care should be taken not to confuse the parasite with ciliated bronchial epithelial cells that resemble Lophomonas morphology in form and characteristics, the main difference being the constant mobility of the parasite — the vibration of its apical flagellae that it uses to move around can be clearly observed under the microscope4–13.
Treatment is based on oral or intravenous metronidazole administration for patients weighing over 40 kg. The dose is 500 mg every 8 h for 20–30 days, depending on the severity of the infection, and for children the dose is calculated at 30–40 mg/kg/day divided into 3 doses. No resistance to this treatment has been reported to date4–13.
In conclusion, this is a rare parasitic infection, which should be suspected in individuals with comorbidities that predispose to immunosuppression, who after being in an endemic place develop a lung infection that responds poorly to antibiotic treatment.
Please cite this article as: Pinos Vélez N, Ordoñez Vintimilla R, Agreda Orellana S. Infección pulmonar por Lophomonas blattarum. Arch Bronconeumol. 2021;57:594–596.