European experience regarding lung cancer screening using low-dose chest CT (LDCT) is available. However, there is limited data on the Spanish experience in this matter. Our aim is to present the results from the longest ongoing screening program in Spain.
MethodologyThe Pamplona International Early Lung Cancer Detection Program (P-IELCAP) is actively screening participants for lung cancer using LDCT since the year 2000 following the IELCAP protocol, including spirometric assessments. Men and women, ≥40 years of age, current or former smokers with a tobacco history of ≥10 pack-years are included. Results are compared to those from other European trials.
ResultsA total of 2989 participants were screened until March 2014 (73% male). A median of 2 (IQR 1–3) annual screening rounds were performed. Sixty lung cancers were detected in 53 participants (73% in Stage I). Adenocarcinoma was the most frequent. The lung cancer prevalence and incidence proportion was 1.0% and 1.4%, respectively, with an annual detection rate of 0.41. The estimated 10-year survival rate among individuals with lung cancer was 70%. Chronic obstructive pulmonary disease and emphysema are important lung cancer predictors.
ConclusionsThe experience in Spain's longest lung cancer screening program is comparable to what has been described in the rest of Europe, and confirms the feasibility and efficacy of lung cancer screening using LDCT.
La experiencia europea en relación con el cribado de cáncer de pulmón con tomografía de baja dosis de radiación (TBDR) es amplia. Sin embargo, la evidencia sobre la experiencia en España es limitada. Nuestro objetivo es presentar los resultados del programa de cribado de cáncer de pulmón más largo de España.
MétodosEl Programa Internacional de Detección Precoz de Cáncer de Pulmón con TBDR de Pamplona (P-IELCAP) viene reclutando individuos de manera activa desde el año 2000 siguiendo el protocolo IELCAP. Se incluyen individuos ≥40 años de edad, fumadores o ex fumadores (consumo acumulado ≥10 paquetes-año). Los resultados se comparan con los de otros estudios europeos.
ResultadosUn total de 2.989 participantes fueron reclutados hasta marzo de 2014 (73% varones), realizando una mediana de 2 (IQR 1-3) rondas de cribado por individuo. Se detectaron 60 cánceres de pulmón en 53 participantes (73% en estadio i). Adenocarcinoma fue el tipo histológico más frecuente. La proporción de prevalencia e incidencia de cáncer de pulmón fue del 1,0 y del 1,4%, respectivamente, con una tasa de detección anual de 0,41. La tasa de supervivencia a 10 años de los pacientes con cáncer de pulmón fue del 70%. La enfermedad pulmonar obstructiva crónica y el enfisema son importantes factores de riesgo para desarrollar cáncer de pulmón.
ConclusionesLa experiencia del programa de cribado de cáncer de pulmón más largo de España es comparable con lo descrito en el resto de Europa y confirma la viabilidad y la eficacia del cribado mediante TBDR.
Lung cancer screening studies using low-dose chest computed tomography (LDCT) began almost two decades ago, when initial results suggested that screening was useful in detecting lung cancer at early stages.1–4 The International Early Lung Cancer Action Program (I-ELCAP), a single arm trial that screened more than 30,000 individuals with LDCT, found that 85% of their lung cancer cases were in clinical stage I, with an estimated 10-year survival rate of 88%.5 Subsequently, results from the randomized National Lung Screening Trial (NLST) showed a significant reduction in lung cancer-specific mortality in the LDCT screening arm.6 These studies encouraged the United States Preventive Task Force (USPSTF) to recommend LDCT screening for lung cancer.7
Many studies have analyzed the results of lung cancer screening in Europe; initial results from a German cohort were published in 2002, and in 2012 the LUSI (Lung Cancer Screening Intervention trial) study was presented.2,8 Other European countries, such as the Netherlands,9 Belgium,9 France,10 Denmark,11 and Italy,12,13 have also been active in this field with their respective trials [NELSON (NEderlands Leuvens longkanker Screenings ONderzoek),9 DEPISCAN,10 DLCST (Danish Lung Cancer Screening Trial),11 DANTE (Detection and Screening of Early Lung Cancer by Novel Imaging Technology and Molecular Essays)12 and ITALUNG13].
Until recently, when the Institute of Oncology of Valencia (IVO) became an I-ELCAP member site and started recruiting participants into this ongoing lung cancer screening program, experience in Spain was limited to a single center in Pamplona, also part of I-ELCAP,5 in which lung cancer screening has been ongoing since 2000. Preliminary data from the early years of screening have been described previously, although they focused on the value of emphysema and chronic obstructive pulmonary disease (COPD) as risk factors for lung cancer and the use of F-18-fluorodeoxyglucose positron emission tomography (PET).14,15 More than a decade later, the number of patients screened and cancers diagnosed has doubled, prompting us to reanalyze the data from our entire cohort to describe the results of the longest ongoing lung cancer screening program in Spain.
Materials and MethodsParticipantsStudy subjects are participants enrolled in the Pamplona International Early Lung Cancer Detection Program (P-IELCAP), part of the I-ELCAP,5 between September 2000 and April 2014. Details regarding individual enrollment, LDCT characteristics, lung cancer detection protocol, emphysema and airway obstruction assessments have been described elsewhere.14,16 Briefly, we included men and women, 40 years of age or older, who were current or former smokers with a smoking history of ≥10 pack-years, with no lung cancer symptoms. In contrast to our previous study, we expanded our baseline data by including smoking status (current or former smoker), body mass index (BMI, calculated by dividing subjects’ weight in kilograms by the square of their height in meters), family history of lung cancer (present or absent), and time since smoking cessation in years.
LDCT and spirometry were performed at baseline and at a follow-up visit up to 1 year later, according to the established I-ELCAP protocol.16 Participants with no nodules or with non-calcified nodules <5mm on LDCT were invited to an annual repeat screening. Positive results (non-calcified nodule ≥5mm) required further study, including any of the following, depending on nodule size and characteristics: PET, antibiotics, three-month repeat LDCT or percutaneous needle or surgical biopsy.16 Individuals whose tests did not suggest or confirm malignancy were invited to continue annual screening. Participants diagnosed with lung cancer were also followed up annually. There was no limit on the number of screening rounds. Emphysema was measured qualitatively and airway obstruction was determined according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommendations (forced expiratory volume in 1s/forced vital capacity (FEV1/FVC) ratio <70%).17 The University of Navarra's ethics committee approved the study protocol and all subjects signed an informed consent prior to enrollment.
Data AnalysisQuantitative data with normal distribution is presented as mean±standard deviation (SD), and non-normal data is presented as median and the interquartile range (IQR). Categorical data were described using relative frequencies. Details of measures of inter-reader reliability and the κ coefficient for visual assessment of emphysema by LDCT are described in our previous study.14
Lung cancer prevalence and incidence rates were calculated according to whether the diagnosis was based on the results of the baseline evaluation or on one of the follow-up screening rounds, respectively. Calculations were based on the number of individuals diagnosed with lung cancer. The incidence rate divided by the median follow-up time yielded the annual lung cancer detection rate, and the inverse of this rate estimated the number of people who needed to be screened in 1 year to detect 1 case of lung cancer (NND).18
The Cox proportional hazards method was used to assess the risk of developing lung cancer using several variables, with special emphasis on COPD and emphysema. Variables used for adjustment in the multivariate analysis included age, sex, pack-years of smoking, BMI, family history of lung cancer and smoking status at baseline.
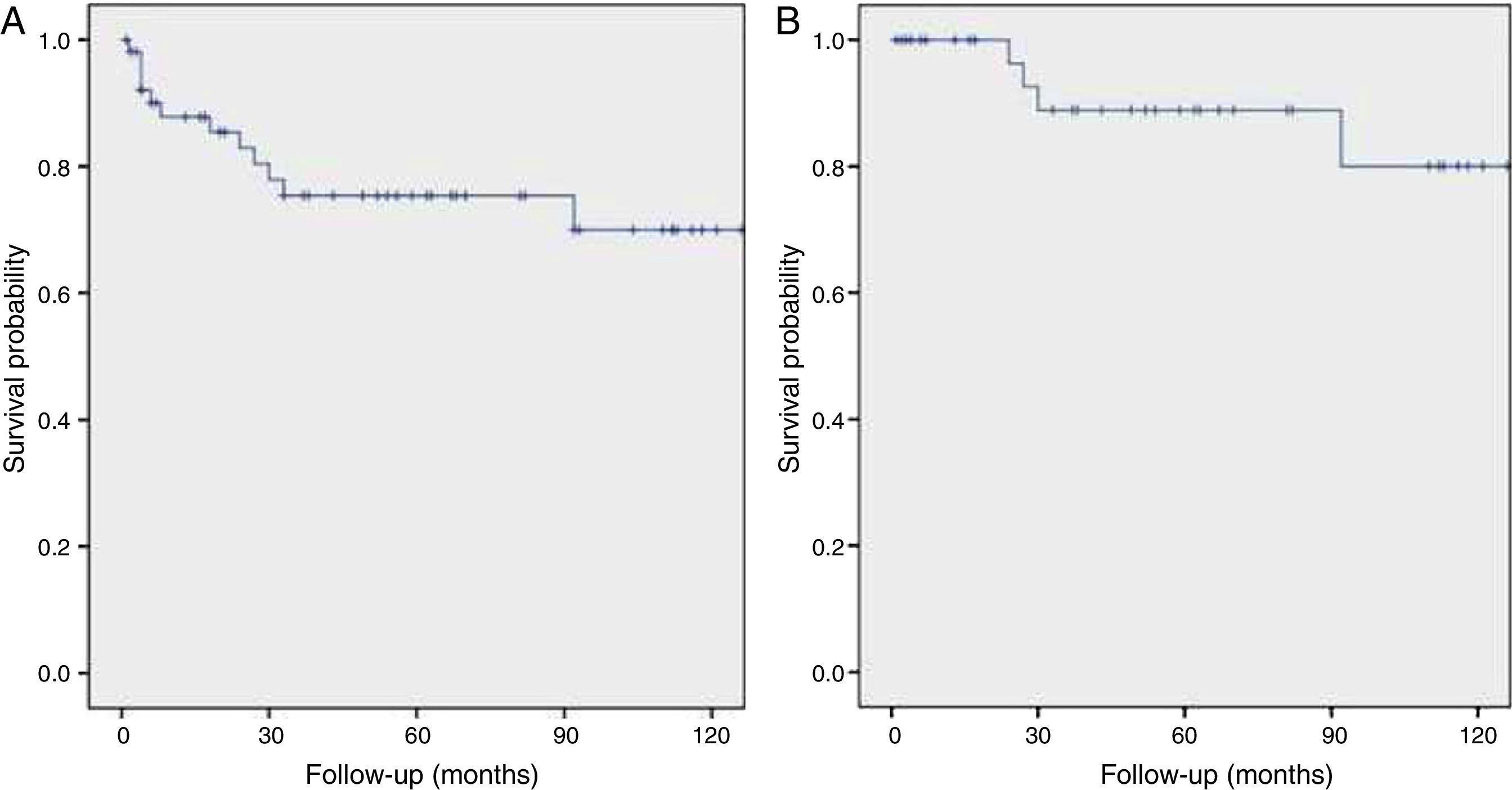
Medical records were reviewed to obtain mortality data on patients with lung cancer and a Kaplan–Meier survival curve was constructed.
A P value of less than .05 was considered statistically significant, and all statistical analyses were performed using SPSS Statistics 20.0 for Windows (IBM, Chicago, IL).
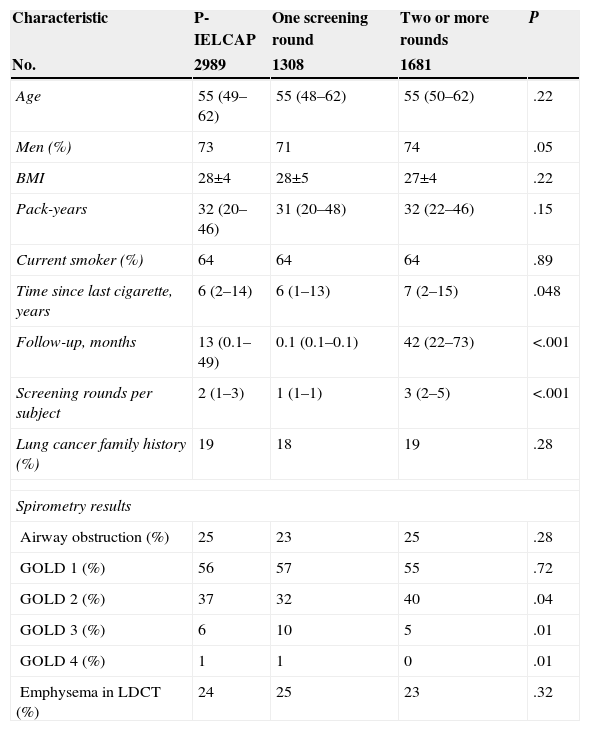
ResultsA total of 2989 individuals were screened, and their baseline characteristics are shown in Table 1. Participants were predominantly men (73%) with a median age of 55 (49–62). Most were current smokers with a history of 32 (20–46) pack-years. Twenty-five percent of the screened population had COPD, 93% with mild or moderate disease (GOLD grades 1 or 2), and 24% had evidence of emphysema on the baseline LDCT. More than half of the sample underwent 2 or more screening rounds. There were no significant differences in baseline characteristics between participants who underwent 1, 2 or more rounds except for COPD severity distribution (Table 1). Participants who complied with screening had a median follow-up of 42 (22–73) months and 3 (2–5) screening rounds.
Baseline Characteristics of the Study Population.
| Characteristic | P-IELCAP | One screening round | Two or more rounds | P |
|---|---|---|---|---|
| No. | 2989 | 1308 | 1681 | |
| Age | 55 (49–62) | 55 (48–62) | 55 (50–62) | .22 |
| Men (%) | 73 | 71 | 74 | .05 |
| BMI | 28±4 | 28±5 | 27±4 | .22 |
| Pack-years | 32 (20–46) | 31 (20–48) | 32 (22–46) | .15 |
| Current smoker (%) | 64 | 64 | 64 | .89 |
| Time since last cigarette, years | 6 (2–14) | 6 (1–13) | 7 (2–15) | .048 |
| Follow-up, months | 13 (0.1–49) | 0.1 (0.1–0.1) | 42 (22–73) | <.001 |
| Screening rounds per subject | 2 (1–3) | 1 (1–1) | 3 (2–5) | <.001 |
| Lung cancer family history (%) | 19 | 18 | 19 | .28 |
| Spirometry results | ||||
| Airway obstruction (%) | 25 | 23 | 25 | .28 |
| GOLD 1 (%) | 56 | 57 | 55 | .72 |
| GOLD 2 (%) | 37 | 32 | 40 | .04 |
| GOLD 3 (%) | 6 | 10 | 5 | .01 |
| GOLD 4 (%) | 1 | 1 | 0 | .01 |
| Emphysema in LDCT (%) | 24 | 25 | 23 | .32 |
Abbreviations: P-IELCAP, Pamplona International Early Lung Cancer Detection Program; BMI, body mass index; GOLD, global initiative for chronic obstructive lung disease; LDCT, low-dose chest computed tomography.
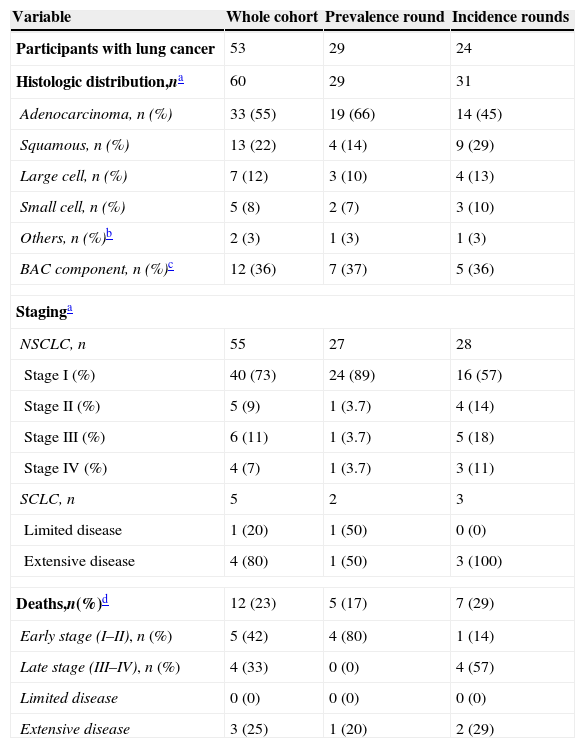
A total of 53 participants were diagnosed with lung cancer: 29 on the first screening round (1.0% prevalence), and 24 on subsequent rounds (1.4% incidence). After the baseline round of screening, the annual lung cancer detection rate was 0.41, and the number of individuals needed to be screened in 1 year in order to detect 1 lung cancer was 245. Two synchronous tumors were found in one participant at his eighth annual screening round (squamous cell carcinoma and adenocarcinoma), and 6 individuals with prevalent lung cancers had a new lung cancer diagnosis in one of the follow-up visits (metachronous tumor). The median difference between the two diagnoses was 48 (34–75) months. All of the metachronous tumors had the same histologic pattern and disease stage, except for 2, where more advanced disease was found on the second cancer. Based on the 60 available samples, the great majority of lung cancers were non-small cell lung carcinomas (NSCLC, 92%), where 55% were adenocarcinomas, followed by squamous cell carcinomas (22%). More than one-third of the identified adenocarcinomas had a bronchioloalveolar component. Eighty-two percent were early stage lung cancers (stages I and II) and 7% were in stage IV. Four of the 5 small cell lung carcinomas (SCLC) were extensive disease. Table 2 shows the lung cancer characteristics of the entire cohort and stratified by screening round.
Characteristics of Lung Cancer Diagnoses.
| Variable | Whole cohort | Prevalence round | Incidence rounds |
|---|---|---|---|
| Participants with lung cancer | 53 | 29 | 24 |
| Histologic distribution,na | 60 | 29 | 31 |
| Adenocarcinoma, n (%) | 33 (55) | 19 (66) | 14 (45) |
| Squamous, n (%) | 13 (22) | 4 (14) | 9 (29) |
| Large cell, n (%) | 7 (12) | 3 (10) | 4 (13) |
| Small cell, n (%) | 5 (8) | 2 (7) | 3 (10) |
| Others, n (%)b | 2 (3) | 1 (3) | 1 (3) |
| BAC component, n (%)c | 12 (36) | 7 (37) | 5 (36) |
| Staginga | |||
| NSCLC, n | 55 | 27 | 28 |
| Stage I (%) | 40 (73) | 24 (89) | 16 (57) |
| Stage II (%) | 5 (9) | 1 (3.7) | 4 (14) |
| Stage III (%) | 6 (11) | 1 (3.7) | 5 (18) |
| Stage IV (%) | 4 (7) | 1 (3.7) | 3 (11) |
| SCLC, n | 5 | 2 | 3 |
| Limited disease | 1 (20) | 1 (50) | 0 (0) |
| Extensive disease | 4 (80) | 1 (50) | 3 (100) |
| Deaths,n(%)d | 12 (23) | 5 (17) | 7 (29) |
| Early stage (I–II), n (%) | 5 (42) | 4 (80) | 1 (14) |
| Late stage (III–IV), n (%) | 4 (33) | 0 (0) | 4 (57) |
| Limited disease | 0 (0) | 0 (0) | 0 (0) |
| Extensive disease | 3 (25) | 1 (20) | 2 (29) |
Abbreviations: BAC, bronchioloalveolar carcinoma; NSCLC, non-small cell lung carcinoma; SCLC, small cell lung carcinoma.
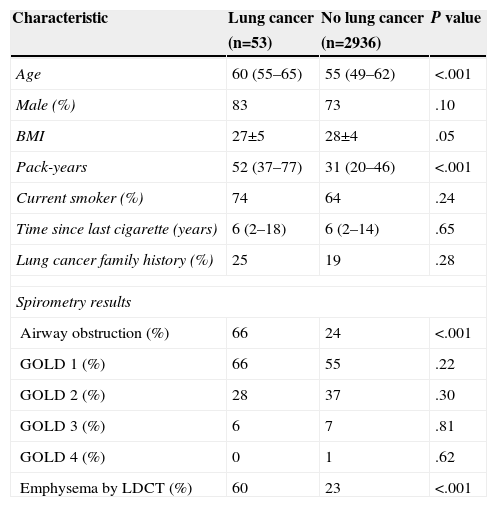
Differences between individuals with and without lung cancer are shown in Table 3. Those with lung cancer were significantly older (5-year difference, P<.001), had a greater smoking history (20 pack-year difference, P<.001), and a significantly higher proportion of airway obstruction and emphysema. Worse lung function, expressed as a lower percent predicted FEV1 and a lower FEV1/FVC ratio, was also observed in participants who developed lung cancer.
Differences in Baseline Characteristics Between Individuals With and Without Lung Cancer.
| Characteristic | Lung cancer | No lung cancer | P value |
|---|---|---|---|
| (n=53) | (n=2936) | ||
| Age | 60 (55–65) | 55 (49–62) | <.001 |
| Male (%) | 83 | 73 | .10 |
| BMI | 27±5 | 28±4 | .05 |
| Pack-years | 52 (37–77) | 31 (20–46) | <.001 |
| Current smoker (%) | 74 | 64 | .24 |
| Time since last cigarette (years) | 6 (2–18) | 6 (2–14) | .65 |
| Lung cancer family history (%) | 25 | 19 | .28 |
| Spirometry results | |||
| Airway obstruction (%) | 66 | 24 | <.001 |
| GOLD 1 (%) | 66 | 55 | .22 |
| GOLD 2 (%) | 28 | 37 | .30 |
| GOLD 3 (%) | 6 | 7 | .81 |
| GOLD 4 (%) | 0 | 1 | .62 |
| Emphysema by LDCT (%) | 60 | 23 | <.001 |
Definition of abbreviations: BMI, body mass index; GOLD, global initiative for chronic obstructive lung disease; LDCT, low-dose chest computed tomography. Data are expressed as mean±standard deviation (SD) or median (interquartile range, IQR).
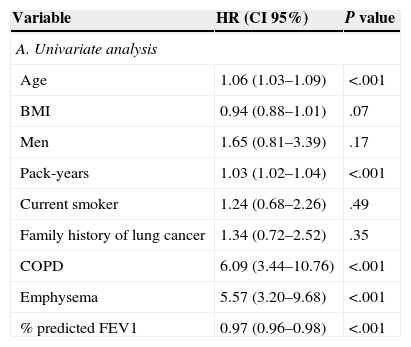
Results from univariate analysis are shown in Table 4A. Age, number of pack-years, COPD, emphysema, and baseline percent predicted FEV1 were significantly associated with lung cancer. On multivariate analysis, after adjusting for age, sex and pack-years of smoking (Model 1), COPD and emphysema were significant risk factors for lung cancer (HR 4.52; 95% CI 2.50–8.18, P<.001; HR 4.52; 95% CI 2.56–7.95, P<.001, respectively). After adding BMI, smoking status at baseline and family history of lung cancer to the previous model, the risk was slightly attenuated without loss of significance. In Model 3, where COPD and emphysema were included in a single model, both were still significant risk factors: HR 3.41; 95% CI 1.85–6.29, P<.001, and HR 3.26; 95% CI 1.82–5.85, P<.001 for COPD and emphysema, respectively (Table 4B).
Cox Univariate and Multivariate Regression Analysis to Assess Lung Cancer Risk.
| Variable | HR (CI 95%) | P value |
|---|---|---|
| A. Univariate analysis | ||
| Age | 1.06 (1.03–1.09) | <.001 |
| BMI | 0.94 (0.88–1.01) | .07 |
| Men | 1.65 (0.81–3.39) | .17 |
| Pack-years | 1.03 (1.02–1.04) | <.001 |
| Current smoker | 1.24 (0.68–2.26) | .49 |
| Family history of lung cancer | 1.34 (0.72–2.52) | .35 |
| COPD | 6.09 (3.44–10.76) | <.001 |
| Emphysema | 5.57 (3.20–9.68) | <.001 |
| % predicted FEV1 | 0.97 (0.96–0.98) | <.001 |
| Variable | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| HR (CI 95%) | HR (CI 95%) | HR (CI 95%) | |
| B. Multivariate analysis | |||
| COPD | 4.52 (2.50–8.18) | 4.42 (2.44–7.99) | 3.41 (1.85–6.29) |
| Emphysema | 4.52 (2.56–7.95) | 4.20 (2.37–7.44) | 3.26 (1.82–5.85) |
Abbreviations: BMI, body mass index; COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1s; HR, hazard ratio. Adjustment models: Model 1: age, sex, pack-years of smoking; Model 2: age, sex, pack-years, BMI, current smoker and family history of lung cancer; Model 3: age, sex, pack-years, COPD and emphysema.
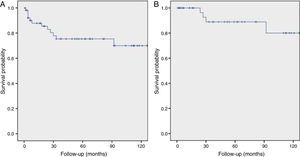
Twelve patients diagnosed with lung cancer died (23%). Most of them (58%) had advanced disease (lung cancer stages III–IV or extensive disease in SCLC). The 10-year lung cancer survival rate among the 53 individuals with lung cancer was 70%. Considering only those with stage I lung cancer, the 10-year survival rate improved to 80%. Mean survival time was 110 (95% CI 93–127) months and 127 (95% CI 111–143) months for all of the individuals diagnosed with lung cancer and those with stage I disease, respectively (Fig. 1).
DiscussionThis study describes the use of LDCT in lung cancer screening in the longest ongoing screening program in Spain, and contributes to European experience in this area.
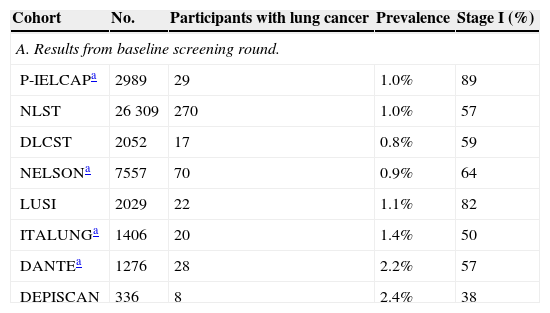
Our results are comparable to those published in other countries in terms of lung cancer prevalence, incidence, histology and staging. Considering only the baseline screening round, our lung cancer prevalence rate was 1.0%. While in the NLST trial (United States) prevalence was 1.0%,19 in Europe these rates varied widely among studies, from 0.8% in the DLCST up to 2.4% in DEPISCAN10,11 (Table 5A). P-IELCAP had the highest proportion of stage I lung cancers in the baseline screening round, with a 30% mean difference with respect to the other studies. Only the LUSI trial showed similar results to ours, probably because their evaluation algorithm, like ours, was based on ELCAP, highlighting the value of using a standard protocol.1,8 Differences in prevalence rates compared to other cohorts could be explained by the inclusion criteria used in each study. For instance, P-IELCAP recruited younger participants with a lower smoking history threshold than other studies.
Differences in Lung Cancer Prevalence and Incidence Rates Between Studies.
| Cohort | No. | Participants with lung cancer | Prevalence | Stage I (%) |
|---|---|---|---|---|
| A. Results from baseline screening round. | ||||
| P-IELCAPa | 2989 | 29 | 1.0% | 89 |
| NLST | 26309 | 270 | 1.0% | 57 |
| DLCST | 2052 | 17 | 0.8% | 59 |
| NELSONa | 7557 | 70 | 0.9% | 64 |
| LUSI | 2029 | 22 | 1.1% | 82 |
| ITALUNGa | 1406 | 20 | 1.4% | 50 |
| DANTEa | 1276 | 28 | 2.2% | 57 |
| DEPISCAN | 336 | 8 | 2.4% | 38 |
| Cohort | No. | Participants with lung cancer | Incidence | Duration (years) | Annual detection rate | Stage I (%) |
|---|---|---|---|---|---|---|
| B. Results from the second and/or subsequent screening rounds. | ||||||
| P-IELCAPa | 1681 | 24 | 1.4% | 3.5 | 0.41 | 57 |
| NLST | 24715 | 379 | 1.5% | 6.5 | 0.24 | 65 |
| DLCST | 1976 | 52 | 2.6% | 4 | 0.66 | 73 |
| NELSONa | 7294 | 130 | 1.8% | 4 | 0.45 | 74b |
| ITALUNGa | 1263 | 18 | 1.4% | 4 | 0.36 | 76 |
| DANTEa | 1114 | 32 | 2.9% | 2.81 | 1.02 | 53 |
| LUSI | NA | NA | NA | NA | NA | NA |
| DEPISCAN | NA | NA | NA | NA | NA | NA |
Abbreviations: P-IELCAP, Pamplona Early Lung Cancer Detection Program; NLST, National Lung Screening Trial; DLCST, Danish Lung Cancer Screening Trial; NELSON (NEderlands Leuvens longkanker Screenings ONderzoek; LUSI, German Lung Cancer Screening Intervention trial; DANTE, Detection and Screening of Early Lung Cancer by Novel Imaging Technology and Molecular Essays; NA, data not available for calculation.
When considering lung cancer diagnoses during annual screenings, incidence determined from P-IELCAP data was 1.4% (Table 5B). This result was comparable to ITALUNG (1.4%), but much lower than that observed in the DLCST (2.6%) and DANTE (2.9%).20–22 When incidence rates were adjusted for the duration of each study (annual detection rate), the results were more homogenous. The P-IELCAP annual detection rate (0.41) was comparable to the results from the NELSON (0.45) and ITALUNG trials (0.36),20,23 while the difference with DLCST was slightly less.21 Possible explanations for the differences between studies could be related to the inclusion criteria employed in each trial, the methods used for recruitment (such as mass mailing used in other studies), the LDCT protocol (slice collimation and thickness), number of screening rounds and the interval between each round, the pulmonary nodule/lung cancer assessment protocol (nodule diameter or nodule volume and volume-doubling times), among others. Participants’ inherent characteristics according to the geographical areas they belong to could also have influenced results.
Adenocarcinoma was the most frequent histological pattern found in our study, consistent with observations from other screening cohorts.8,10,19–21
The proportion of stage I lung cancers detected on the incidence rounds decreased significantly in P-IELCAP (from 89% to 57%). From the European studies mentioned here, only the DANTE trial showed similar behavior, but not to the same extent.22 This trend, however, has also been reported in other studies,24 such as the Lung Screening Study (53%–25%),25 the Pittsburgh Lung Screening Study (58%–37%)26 and a study by Swensen and colleagues (71%–50%).27 The 57% stage I disease found in P-IELCAP incidence screening rounds is in line with other series, such as DANTE (53%) and the NLST (65%).22,28
As previously mentioned, P-IELCAP was one of the many sites involved in the I-ELCAP, and part of our cohort was included in the 2006 article, for which more than 30,000 participants were recruited from sites in North America, Europe and Asia.5 With only a fraction of participants from the latter (11%), P-IELCAP results were consistent with those from I-ELCAP, especially in the baseline screening round (1.3% prevalence and 85% stage I lung cancer in I-ELCAP, compared to the 1.0% prevalence and 89% stage I lung cancer in P-IELCAP). However, some differences were found in the incidence rounds, where even though the incidence rate was much lower in I-ELCAP (0.3% vs 1.4% in P-IELCAP), a high stage I lung cancer detection was maintained (86% vs 57% in P-IELCAP). In spite of this difference, the 10-year survival rates for patients with stage I disease were comparable in both studies (80% in P-IELCAP and 88% in I-ELCAP, respectively) (Fig. 1B).5
These results show that lung cancer screening with LDCT in a Spanish center is feasible and effective. However, this study was performed in a private center and results may not be entirely applicable to public institutions in a country where national health coverage predominates. Costs and resources’ utilization would be important limitations in this setting. Regarding cost-effectiveness, an actuarial analysis in a high-risk population in the United States suggested that offering lung cancer screening as an insurance benefit would save lives at relatively low cost.29 What is clear, and backed by most current guidelines, is that screening targeting a high-risk population should be performed in medical centers where multidisciplinary teams are available.30,31
Our study also confirms the value of COPD and emphysema as important risk factors for lung cancer in a screening setting. None of the studies cited previously have made this assessment. However, the NLST and the Pittsburgh Lung Screening Study (PLuSS) have confirmed the value of emphysema in selecting high-risk patients.32,33 This observation is further confirmed by measuring the lung cancer incidence density, where COPD and emphysema showed a three-fold increase (23 and 21 lung cancers per 1000 person/years, respectively, when compared to the entire cohort, 7 lung cancers per 1000 person/years). Interestingly, when both COPD and emphysema were present in a single individual, the incidence density was highest (39 lung cancers per 1000 person/years). Among patients with COPD, most of the lung cancer diagnoses were made in individuals with mild disease (33 cases within GOLD grades 1 and 2; whereas only 2 lung cancer cases were detected in severe grades). Our results are consistent with those from the BODE cohort, where increased risk was also observed in mild disease.34,35 However, it contrasts with data from the PLuSS, where patients with severe COPD had significantly higher risk for lung cancer.32 Studies have been consistent in describing the relationship between COPD and lung cancer over the past two decades, and its importance in lung cancer screening was confirmed.14,32,36,37 Other factors such as time between COPD diagnosis and lung cancer development have also shown a strong association.38
There are some potential limitations in our study. Firstly, P-IELCAP is a single-center, single-arm screening study, and comparisons with the aforementioned randomized trials should be interpreted cautiously. The reason for choosing these studies was to compare the Spanish experience with that of other European countries. Only the results from the NLST trial were included from outside Europe as it is a reference in the field.6 Secondly, the screening compliance in our study was low, as only 56% of participants underwent at least a second screening round, compared to more than 90% compliance observed in most of the cited trials. This would be an important limitation if we were to compare global results. We believe this limitation is minimized by measuring prevalence and incidence rates independently in those participants who underwent 1, 2 or more screening rounds, respectively. This made our compliant group comparable to the other trials in terms of follow-up and number of screening rounds. We previously assessed the issue of low adherence in our screening program, finding that it varied according to sex, distance to the referral center, participant motivation, and risk perception, among others.39 Thirdly, it is likely that a selection bias, particularly a healthy volunteer effect, could be present. The latter has been further described by Dominioni et al. in a chest X-ray lung cancer screening setting, where participants in the intervention group had higher lung cancer mortality than the control group.40 In our study, although there was no significant differences in baseline lung function (percent predicted FEV1) between those who underwent 1 or more than 1 screening round, in the subgroup of patients with COPD those with milder disease were more compliant with the scheduled visits. We do not address the issue of over-diagnosis in this study because of the lack of a control group. However, the significant reduction in lung cancer mortality found in the NLST proves that over-diagnosis is not a limiting issue.6 Finally, regarding possible unnecessary procedures or false positive results, we refer to the original I-ELCAP study, where 92% of biopsies (492 out of 535) performed after a positive LDCT resulted in a malignant diagnosis.5
We conclude that the experience in Spain's longest lung cancer screening program is comparable with findings from the rest of Europe, and confirms the feasibility and efficacy of lung cancer screening using low-dose computed tomography. COPD and emphysema are important risk factors for lung cancer and should be considered in the selection of high-risk individuals for lung cancer screening.
Contributions to the StudyThe conception of the study and its design was carried out by P.S.S., J.B., J.P.d.T., A.C., A.B.A., A.V., J.C.P., M.D.L., M.J.G.V., L.M.S., J.G., G.B., and J.J.Z. P.S.S., J.P.d.T., L.M.S., and J.J.Z. also carried out the analysis and interpretation, and drafted the manuscript for important intellectual content.
Funding SourceThis work was supported (in part) by a grant (RD12/0036/0062) from Red Temática de Investigación Cooperativa en Cáncer (RTICC), Instituto de Salud Carlos III (ISCIII), Spanish Ministry of Economy and Competitiveness & European Regional Development Fund (ERDF) “Una manera de hacer Europa”.
FIS projects: PI04/2404, PI07/0792, PI10/01652, and PI11/01626.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: Sanchez-Salcedo P, Berto J, de-Torres JP, Campo A, Alcaide AB, Bastarrika G, et al. Cribado de cáncer de pulmón: catorce años de experiencia del Programa Internacional de Detección Precoz de Cáncer de Pulmón con TBDR de Pamplona (P-IELCAP). Arch Bronconeumol. 2015;51:169-176.