Congenital lung abnormalities encompass a broad, heterogeneous spectrum of malformations, including bronchial atresia, congenital lobar emphysema, bronchogenic cyst, cystic adenomatoid malformation, and pulmonary sequestration (PS). The vast majority of these developmental abnormalities are diagnosed in the pediatric age group, especially neonates and infants, but a small proportion are detected at later stages, mainly during adolescence or young adulthood.1 We report a case of PS detected incidentally in a 77-year-old patient.
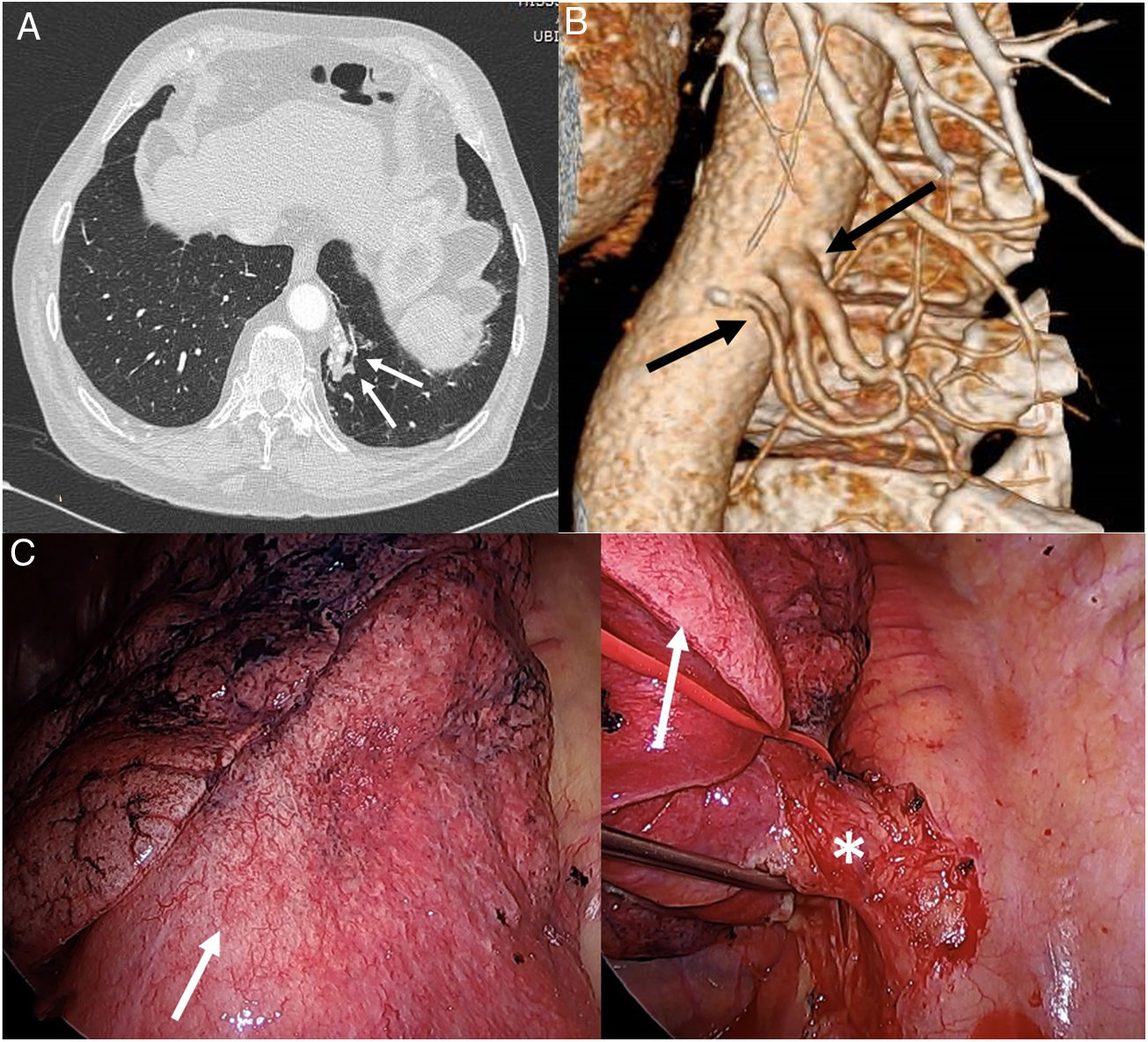
Our patient was a male never-smoker and with no history of interest, who consulted in our hospital after several self-limiting episodes of scant hemoptysis accompanied at times by low-grade fever. He had no chest pain or dyspnea. Despite the fact that the chest X-ray showed no apparent radiological alterations, he received empiric treatment with antibiotics, leading to the resolution of symptoms. However, 4 weeks later the patient experienced another episode of hemoptysis, so we decided to perform a chest computed tomography (CT). Chest CT with intravenous contrast revealed a pseudonodular opacity in the para-aortic region of the left lower lobe (Fig. 1A), that showed characteristic systemic arterial irrigation consisting of 2 arteries that originated in the descending thoracic aorta (Fig. 1B), and venous drainage to the left inferior pulmonary vein, resulting in a diagnosis of PS. The patient was successfully treated by biportal video-guided thoracoscopy, with resection of the PS after dissecting the arterial branch of the thoracic aorta that vascularized it (Fig. 1C). Subsequent progress was good, and the patient has not experienced any more episodes of hemoptysis to date.
(A) Axial image of chest CT (pulmonary parenchymal window) showing a paramediastinal lesion in the basal segment of the left lower lobe (arrows). (B) Volumetric reconstruction of chest CT revealing the presence of 2 systemic arteries (arrows) that originate in the descending thoracic aorta and irrigate the pulmonary lesion, thus confirming the diagnosis of pulmonary sequestration. (C) Intraoperative image of: (1) pulmonary sequestration (white arrow) and (2) arterial vascularization (asterisk) of the pulmonary sequestration (white arrow).
PS is a rare congenital anomaly of the lower respiratory tract consisting of a non-functional mass of lung tissue, usually without communication with the tracheobronchial tree, which receives its arterial blood supply from the systemic circulation (most often from the thoracic or abdominal aorta) instead of the pulmonary circulation.1 Several hypotheses have been proposed for its etiology, but the most accepted theory suggests that the PS originates during embryogenesis from an accessory germinal lung bud.2 It accounts for 0.15%–6.4% of all aberrant lung development. Two forms of PS have been described: intralobar (75%–93% of all PS) and extralobar (less common). Intralobar PS lacks its own pleural lining; it is located within a lung lobe (more frequently in the lower lobes, particularly in the left side), and is usually diagnosed in the pediatric age group as a result of recurrent lung infections. Extralobar PS has its own visceral pleural lining. It is usually diagnosed with ultrasound prenatally or in the first year of life, and is often associated (in up to 50% of cases) with other congenital abnormalities (thoracic and extrathoracic).3 Although the majority of patients with intralobar PS are asymptomatic, the most common symptomatic presentation after the neonatal period is lung infection. In a recent review of PS in 72 adults (16–75 years), the most common symptom on presentation was cough with expectoration (81.9%), followed by hemoptysis (29.2%), fever (25%), and chest pain (20.8%).4 Our case is unusual due to the age of the patient (77 years) and the clinical presentation (episodes of hemoptysis). Due to the increasing use of imaging techniques (especially CT), a growing number of congenital lung malformations are diagnosed incidentally in adult patients undergoing radiological studies for different reasons.5
CT angiogram has become the diagnostic method of choice for PS, as this technique can demonstrate not only the vascular anatomy of these anomalies, but also their relationship with the tracheobronchial tree and the coexistence of other congenital alterations. In spite of advances in imaging techniques and their importance in the diagnosis of this entity, most adult patients with PS are diagnosed during or after thoracic surgery, so it seems quite common in clinical practice to confuse PS with other more prevalent lung diseases.4
PS is usually treated by surgery (lobectomy or segmentectomy), especially in symptomatic patients and/or those in whom cancer cannot be ruled out6; the management of asymptomatic adults is more controversial, although most authors recommend resection of the PS to avoid recurrent infections (which would complicate a surgical intervention, should it be needed in the future).7
Despite its rarity, we believe that the PS should be included in the differential diagnosis of hemoptysis in elderly patients, especially in never-smokers, and when lung lesions are located in the lower lobes.
Please cite this article as: Velasco-Álvarez D, Gorospe-Sarasúa L, Fra Fernandez S, Rodríguez Calle C. Secuestro pulmonar intralobar: una causa excepcional de hemoptisis en un paciente septuagenario. Arch Bronconeumol. 2019;55:499–500.