Gallstone ectopia in the chest cavity is a rare entity.1 Less than 20 cases have been described in the literature. It is associated with a history of manipulation of the bile duct, when gallstones pass into the peritoneal cavity and reach the chest through weak points in the diaphragm.2 Once in the lung, they generate an inflammatory reaction causing a mass effect that can begin with hemoptysis or pulmonary infiltrate.
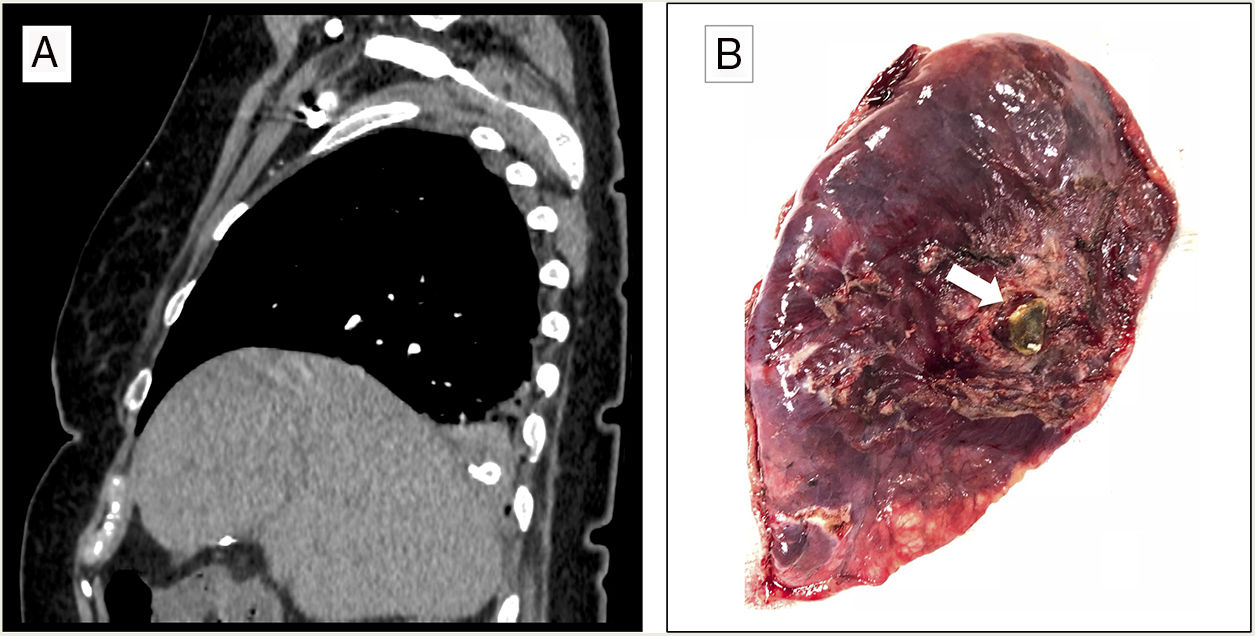
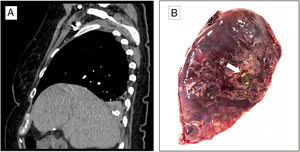
We report the case of a 73-year-old woman who presented in the emergency department of our hospital with suspected choking followed by a fit of coughing with bloody sputum. Her history was significant for complicated calculous cholecystitis 4 months previously, for which she underwent laparoscopic cholecystectomy. Her gallbladder was accidentally perforated during the surgical intervention, with spillage of gallstones to the peritoneal cavity. The initial exploration was normal, and no anomalies were detected in the analytical tests. The study was completed with a chest X-ray (normal) and a chest CT scan that revealed occupation of the right bronchial lumen and the presence of a foreign body with the density of calcium in the right lower lobe (RLL) (Fig. 1A). The patient was diagnosed with hemoptysis possibly associated with foreign body aspiration, so she was given prophylactic antibiotic therapy and a rigid bronchoscopy was performed. This technique revealed the presence of abundant blood clots and erythematous mucosa, with no foreign body in the airway. The clinical situation persisted, marked by recurrent episodes of hemoptysis. In view of this progress and the history of manipulation of the bile duct, we opted for a surgical approach to reach a definite diagnosis. RLL adhesions to the diaphragm were observed, so these were released, and an atypical resection was performed of the same lung lobe, corresponding to the site where the foreign body had been seen on the CT scan. After resection, the surgical specimen (12.5×6.5×3cm) was examined macroscopically and a gallstone was observed (Fig. 1B). The pathology study found organizing pneumonia on post-inflammatory bronchiectasis with an imbedded gallstone, along with fibrosis and chronic lymphohistiocytic inflammation with foreign-body giant-cell reaction. The postoperative period was uneventful, the patient was discharged to home, and the episodes of hemoptysis did not recur in the subsequent follow-up.
Pulmonary gallstone ectopia is not uncommon and is associated with hepatobiliary surgery. Laparoscopic cholecystectomy is the therapy of choice for symptomatic cholelithiasis, and has advantages over open surgery, including a smaller incision, less pain, and a shorter hospital stay. However, perforation of the gallbladder, with an incidence of 10%–32%, is relatively frequent during these procedures, and 2.3% of these events involve the loss of gallstones.3,4 Risk factors such as age, number and size of the gallstones, and acute cholecystitis are associated with the perforation of the gallbladder and gallstone spillage.3 Careful recovery of as many gallstones possible is recommended to avoid dissemination to hard-to-access sites and to minimize possible secondary complications.2 These complications are rare: in a series of more than 1000 patients, the authors found 5 cases with complications associated with lost gallstones.5 Most were intraperitoneal, while thoracic incidents was more infrequent. It is postulated that the gallstones access the chest through weaknesses in the diaphragm, where they go on to generate an inflammatory process in the lung tissue. Possible access routes include congenital defects of the diaphragm or transdiaphragmatic passage after an inflammatory reaction.6 The time between the manipulation of the bile duct and diagnosis ranges from 2 to 60 months.1
The most common symptom is hemoptysis, and in most of the published cases the location was the RLL (93.3%; 14 of 15 cases published).1 Hemoptysis can be isolated, persistent, or even present as massive hemoptysis.7 Other possible clinical manifestations include empyema and cholelithoptysis.8,9 The therapeutic approach depends on clinical progress. Antibiotics are only indicated when there are signs and symptoms of infection due to obstruction or process of another type, but not if the only sign is hemoptysis. In 4 of the 15 cases published, a conservative attitude was adopted with antibiotic treatment being prescribed in 3 cases, but symptoms were resolved in all cases after the patient coughed up the gallstone.1 Surgery is reserved for cases of recurrent hemoptysis or persistent symptoms. The gallstone and the inflamed tissue can be removed by atypical resection, whereas lobectomy is only indicated in more complicated cases. Some authors propose standardizing the approach and follow-up of cases when gallstones are lost during laparoscopic cholecystectomy, in order to achieve early detection and avoid complications.1,2,10
An accurate case history and review of prior medical events are important to identify the etiology of hemoptysis. Gallstone ectopia is rare, but it should be considered as a possible cause in patients with a history of biliary surgery who present hemoptysis and RLL infiltrates.
Please cite this article as: Sánchez-Moreno L, Ballesteros MA, Peña-Gómez E, Pérez Martín I. Hemoptisis como manifestación de la ectopia torácica de cálculos biliares. Arch Bronconeumol. 2019;55:498–499.