Interstitial pulmonary edema is a functional lung disorder that limits diffusing capacity. It causes changes in the alveolocapillary barrier,1,2 and has been described in athletes who perform long-duration, high-intensity activities, particularly divers,3 all types of swimmers,4 and mountaineers.5 It is also very well characterized in race horses.6 Its prevalence in sport is unknown, although it is in all likelihood underestimated, and it is now called “swimming-induced pulmonary edema” (SIPE)4 because of its association with various water sports. The condition is caused by overload of the pulmonary capillary bed due to exercise that demands high cardiac output, by the need to redistribute that volume due to the temperature of the water, by the position of the chest, and sometimes by unnecessary overhydration.7 It is also reasonable to suppose that the presence of certain inflammatory processes that modify lung tissue permeability8 coupled with overtraining might facilitate the development of pulmonary edema in these athletes.
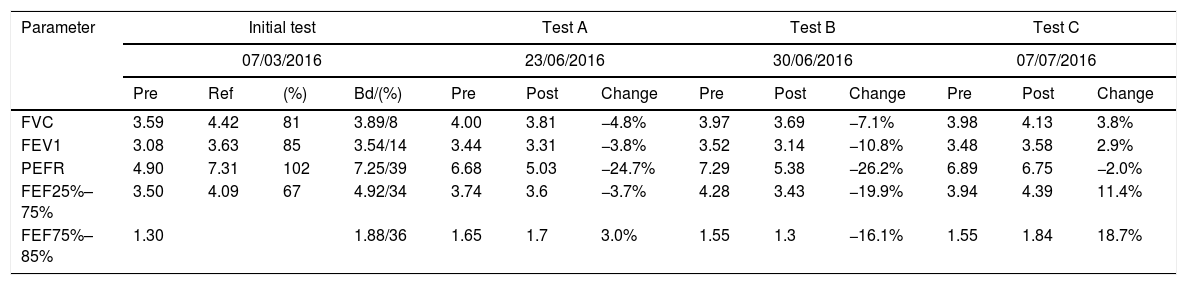
We report the case of an Olympic-class swimmer, 21 years of age, with mild intermittent asthma in childhood for which she now only occasionally requires preventive treatment for exercise-induced asthma. She presented with incongruous symptoms, despite correct treatment for her asthma. The patient complained of a marked sensation of dyspnea that was “different” from her usual asthma, with progressive onset, associated with the intensity of exercise, causing clear limitation at a moderate swimming speed. The syndrome also involved greater peripheral upper limb fatigue than would usually correspond to the type of effort made, which would resolve after a brief rest, only to reappear when the same type of effort was made. Previous clinical history and physical examination were normal, with no symptoms suggestive of respiratory tract infection, and no exposure to environmental pollutants or allergens. Forced spirometry was performed, showing lower values than expected in a swimmer9 and an obstructive pattern with a positive bronchodilator (initial test in Table 1). Standard core treatment began with a combination of budesonide/formoterol 320/9μg in dry powder, twice a day, administered in a schedule adjusted to her training sessions, i.e., first dose before the morning session and second dose before the evening session. After 3 months of treatment, the swimmer's symptoms and performance limitation were somewhat less intense, but continued to affect her training sessions. Spirometry before and after the training session at that time showed some bronchoconstriction on exertion (test B in Table 1). Auscultation after the session only revealed heavy, intense breathing with an elongated expiration; pulse oximetry showed values between 95% and 98%. Given the suspicion of a possible overload of the vascular bed due to interstitial pulmonary edema and the difficulty of evaluating and monitoring changes in DLCO, a post-exertion pulmonary parenchyma ultrasound was performed, in which the B-lines (comet tail signs) typical of pulmonary edema were observed.10 proBNP levels were evaluated before and after exertion, showing values of 8.3 and 8.5pg/ml, respectively, considered normal. Believing that this could be a case of exercise-limiting pulmonary edema, we requested permission from the Spanish Anti-doping Agency to use a short, 1-week course of a carbonic anhydrase,11 acetazolamide, for preventive and diagnostic purposes: the presence of diuretics in a urine sample in a doping test is considered an adverse result under section S5, as this substance might be used to improve performance or change an outcome (e.g., losing weight to change category), or to mask the use of other prohibited substances.12 During the waiting period, the swimmer discontinued preventive treatment; her symptoms remained the same and greater bronchoconstriction was seen on spirometry. Acetazolamide 250mg p.o. was administered in a single morning dose for 1 week, as planned, with no combined preventive treatment. As can be seen in test C of Table 1, on completion of this period, post-exertion spirometric values even showed bronchodilation in the post-training procedure, with a total absence of signs or symptoms of respiratory distress and a normal post-exercise ultrasound.
Forced spirometry performed before training (Pre) and 30min after training (Post). Test A is the procedure performed after 1 week of budesonide and formoterol, test B is after 1 week without treatment, and test C is after 1 week of acetazolamide.
| Parameter | Initial test | Test A | Test B | Test C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 07/03/2016 | 23/06/2016 | 30/06/2016 | 07/07/2016 | ||||||||||
| Pre | Ref | (%) | Bd/(%) | Pre | Post | Change | Pre | Post | Change | Pre | Post | Change | |
| FVC | 3.59 | 4.42 | 81 | 3.89/8 | 4.00 | 3.81 | −4.8% | 3.97 | 3.69 | −7.1% | 3.98 | 4.13 | 3.8% |
| FEV1 | 3.08 | 3.63 | 85 | 3.54/14 | 3.44 | 3.31 | −3.8% | 3.52 | 3.14 | −10.8% | 3.48 | 3.58 | 2.9% |
| PEFR | 4.90 | 7.31 | 102 | 7.25/39 | 6.68 | 5.03 | −24.7% | 7.29 | 5.38 | −26.2% | 6.89 | 6.75 | −2.0% |
| FEF25%–75% | 3.50 | 4.09 | 67 | 4.92/34 | 3.74 | 3.6 | −3.7% | 4.28 | 3.43 | −19.9% | 3.94 | 4.39 | 11.4% |
| FEF75%–85% | 1.30 | 1.88/36 | 1.65 | 1.7 | 3.0% | 1.55 | 1.3 | −16.1% | 1.55 | 1.84 | 18.7% | ||
Based on the available information, and in the absence of a DLCO determination that would be decisive, we can validate the presence of exercise-induced mild interstitial edema in this swimmer, that resolved with the administration of acetazolamide. This case is an illustration of the usefulness of spirometry as a simple, practical tool to support the clinical history in this serious disorder, especially in the practice of open-water swimming13; it also highlights the need to decide if a patient is a candidate for a medication that is considered a positive doping agent, and thus requires a request for therapeutic authorization. We know that lung diffusion improves with training,14 and that it is one of factors that can determine differences in sports performance.15,16 Each case must be studied separately to determine if SIPE is a specific adaptation problem caused by associated physiopathological factors rather than inflammatory processes, or if it a response to definitive functional limitation in some individuals. A therapeutic intervention must never be targeted solely at sports performance. In this respect, the sports authorities should be cautious in deciding whether to permit an athlete to use a substance, depending on whether its use is considered to be a preventive measure for a pathological response or a measure for overcoming a limitation to exertion. This decision should be based on reports and tests that are adapted to our knowledge of these entities, and we must continue to develop these strategies.16
Please cite this article as: Drobnic F, García-Alday I, Banquells M, Bellver M. Edema pulmonar intersticial en el deporte de alta competición y acetazolamida: a propósito de un caso. Arch Bronconeumol. 2018;54:584–585.