The identification of asthma exacerbations (AE) seen in emergency departments and in the home is proposed as a parameter of asthma control and for monitoring environmental triggers.
Patients and methodsAll AEs seen in 2005 and 2011 in the reference hospital of the region and in the patients’ homes by the Emergency Medical Services were identified.
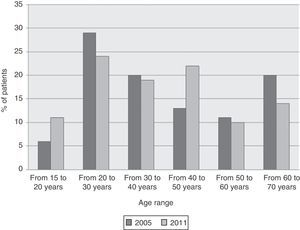
ResultsThe incidence of AE was 1.93/106inhabitants/day during 2005, and 2/106inhabitants/day in 2011. The most common triggers were slow onset common cold of more than 24h duration in 104/219 (47%) AEs in 2005 and 107/220 (49%) in 2011; prior bronchial symptoms with cough, expectoration and fever were recorded in 41/219 (19%) in 2005 and in 57/220 (26%) AEs in 2011. In total, 49% (2005) and 74% (2011) of the AEs had onset more than 24h before admission.
ConclusionsNo significant differences were observed in the rate of attendance in the emergency department due to AE between 2005 and 2011. The most common triggers were common cold and bronchial symptoms with expectoration and fever. AE had begun more than 24h previously in at least half of cases. These findings appear to suggest that there may be a scope for improvement in the outpatient care of the asthmatic patient.
Se propone la identificación de las agudizaciones asmáticas (AA) atendidas en el Servicio de Urgencias y en el domicilio como parámetro de control y vigilancia de la actuación de desencadenantes ambientales.
Pacientes y métodos Se identificaron todas las AA atendidas durante los años 2005 y 2011 en el hospital de referencia de la zona y en el domicilio de los pacientes por el Servicio de Emergencias Médicas.
ResultadosLa incidencia fue de 1,93AA/106habitantes/día en el año 2005 y de 2AA/106habitantes/día en el 2011. Los desencadenantes más frecuentes fueron: un catarro nasal de instauración lenta de más de 24h en 104/219 (47%) de las AA en 2005 y en 107/220 (49%) en 2011; un cuadro bronquial previo con tos, expectoración y fiebre se registró en 41/219 (19%) en el año 2005 y en 57/220 (26%) de las AA en 2011. En conjunto, el 49% (2005) y el 74% (2011) de las AA se habían iniciado más de 24h antes de su admisión.
ConclusionesNo se han observado cambios significativos de la tasa de frecuentación en los servicios de urgencias por AA entre los años 2005 y 2011. Los desencadenantes más frecuentes fueron el catarro nasal y un cuadro bronquial con expectoración y fiebre. La instauración de la AA fue de más de 24h en al menos la mitad de las AA. Estos hallazgos parecen indicar que existe un margen de mejora en la asistencia ambulatoria del paciente asmático.
Asthma exacerbations (AE) are considered serial, either due to poor baseline control, or to the activation of a trigger.1 It is therefore believed that proper treatment and avoidance of known triggers will lead to good disease control and prevent flare-ups.1
Several studies in recent years have concluded that following international recommendations on background therapy averts flare-ups and reduces the use of healthcare resources.2 In fact, a study by Molfino et al.3 showed that a follow-up program for asthmatic patients that included optimal treatment and self-monitoring was associated with better survival, which is directly related with avoidance of AEs. Similarly, the continuous use of inhaled steroids is known to be associated with a decrease in exacerbations and reduction in mortality.4,5 In short, appropriate background therapy and a written action plan to deal with flare-ups (that includes oral corticosteroids) is known to improve patient control and prevent AEs.6 It was also recently shown that after adjusting treatment to GINA recommendations, just 2 short educational campaigns reduced the number of visits to the family doctor and the emergency department.7
Given the difficulty of identifying all AEs as a parameter of the degree of control in a particular population, we followed the protocol of previous studies (ASMAB I8 and II9) and only identified a proportion of exacerbations: those treated in the emergency department of a tertiary hospital and those treated in the patient's home by the emergency medical service (EMS). In fact, our group had already carried out this research in Barcelona in the ASMAB I study8 (autumn 2001 to winter 2002) and the ASMAB II study (autumn of 2003),9 where we were able to show that the daily AE rate was 0.53 and 0.37 exacerbations per 105 inhabitants/day, respectively, i.e. between 4 and 5 patients treated daily per million inhabitants.
Insight into the incidence of AEs may serve 2 purposes: first, to determine the degree of control of a local asthmatic population, and secondly, to evaluate and compare incidence of AEs due to an environmental triggering agent with that of ordinary days. This was the case in Barcelona in 1981–1987, when a cargo of soybeans unloaded in the port resulted in high numbers of patients attending emergency departments for an AE.10 This same type of study could be used, for example, to determine whether AEs increase on days with a high level of pollution in cities.
We conducted 2 new studies in 2005 and 2011 with the primary objective of re-determining the incidence of AEs. Both were carried out using the same data collection protocol, in the same area and at the aforementioned care levels: home and hospital emergency department. As secondary objectives, AE triggering factors and the characteristics of the onset were also examined.
Materials and MethodsStudy DesignThe present study included 2 prospective studies conducted in 2005 (ASMAB III) and 2011 (ASMAB IV). Both were designed to calculate the rate of AEs in individuals aged between 14 and 70 years, who had been seen in the emergency department of the only tertiary hospital in the area. AEs treated in the patients’ own homes during the same period were also identified. Patient data was treated confidentially in accordance with the Spanish Data Protection Act in force at that time. The study was approved by the hospital Ethics Committee.
Study PopulationAccording to the census of the city of Barcelona, 453,196 inhabitants were registered in the catchment area of the tertiary hospital in 2005. The population aged under 14 years accounted for 10.9%, and those over 70 years for 15.52%; therefore, the population aged between 14 and 70 years was made up of 333,462 individuals. In 2011, there were a total of 404,972 inhabitants, of which the population aged under 14 years accounted for 12.3% and those over 70 years for 15.77%, giving a catchment population of 291,296 inhabitants.11
Methods for Identifying Patients With Asthma Exacerbation Seen in the Hospital and Inclusion CriteriaThe data collection protocol designed for the previous studies (ASMAB I and ASMAB II) was used to identify the AEs seen in the hospital.8,9 This consisted of an ad hoc list containing the personal details of each patient, date, time from onset to treatment in the emergency department, and the main trigger. Details of patients attended in their own home were provided by the EMS, as in the previous studies.
In summary, all AE episodes seen in the emergency department were identified weekly by the physicians in charge of both studies (TG in 2005 and IO in 2011). The medical records of individuals who presented any of the following diagnoses were reviewed: bronchial asthma, bronchospasm, bronchial hyperresponsiveness, asthmatic bronchitis, spastic bronchitis, wheezing, status asthmaticus, acute or severe asthma attack and severe asthma exacerbation. The diagnosis of asthma was accepted if the patient, in addition to the diagnosis of asthma made in the emergency department, met the clinical criteria established by GINA,1 i.e. history of episodes of dyspnea, wheezing and chest tightness, as well as variability in these symptoms; a family history consistent with asthma and atopy supported the diagnosis. Relapse criterion was readmission within 15 days of discharge from the emergency department; if readmission was after this period, it was counted as a new episode.
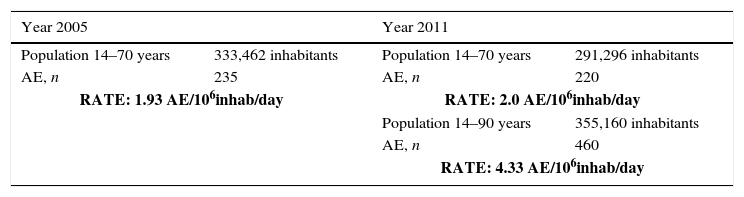
Statistical AnalysisThe incidence rate for AEs seen in the emergency department of the hospital in 2005 and 2011 was calculated using the following formula:
The population at risk was 333,462 individuals in 2005, and 291,296 in 2011. The percentage of asthmatic patients in Barcelona city was estimated at 6.5%,12 which represents a total of 19,030 individuals in 2005 and 18,934 in 2011. The follow-up time in both periods was 365 days.
The difference in AE rates between 2005 and 2011 was analyzed and the statistical significance calculated. The clinical characteristics of AE episodes in the home and in hospital in 2005 and 2011 are expressed as absolute frequencies and their corresponding percentages. The characteristics of episodes and patients in the 2 periods were compared using the Chi square test. Results were considered statistically significant if P<.05. Statistical analysis was performed using SPSS®, version 17. 0.
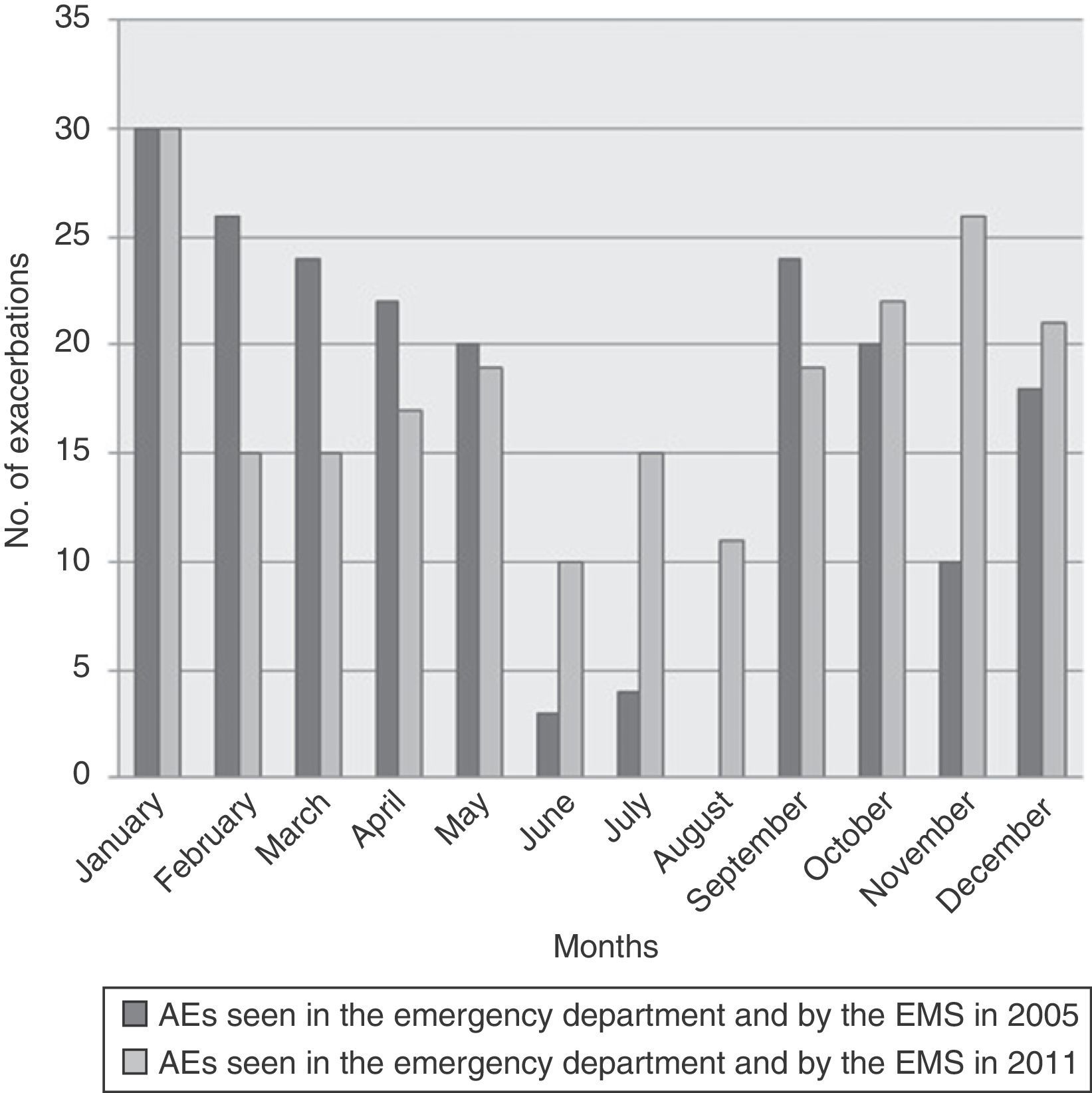
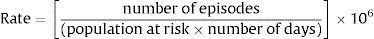
ResultsRate (Table 1)A total of 235 AEs were identified in 2005 during the 365 days of the study, treated in both the hospital emergency department and by the EMS, giving an incidence rate of 1.93 AE/106 inhabitants/day. The incidence rate during the same 365-day period in 2011 was 2.0 AE/106 inhabitants/day. Taking into account the asthmatic population alone,12 this gives a rate of 34 and 31 AE/106 asthmatic patients in 2005 and 2011, respectively. In 2011, 260 asthmatics aged over 70 years were seen in the emergency department; therefore, if we also take into account AEs in patients aged up to 90 years, as in the ASMAB I and II studies, the total population would be 355,160 inhabitants and the rate would be 4.4 AE/106. Frequency by months in 2005 and in 2011 is shown in Fig. 1.
Rate of Asthma Exacerbations Seen in the Emergency Department and at Home by the Emergency Medical Service.
| Year 2005 | Year 2011 | ||
|---|---|---|---|
| Population 14–70 years | 333,462 inhabitants | Population 14–70 years | 291,296 inhabitants |
| AE, n | 235 | AE, n | 220 |
| RATE: 1.93 AE/106inhab/day | RATE: 2.0 AE/106inhab/day | ||
| Population 14–90 years | 355,160 inhabitants | ||
| AE, n | 460 | ||
| RATE: 4.33 AE/106inhab/day | |||
In 2005, 17 patients treated by the EMS in their home did not require subsequent referral to hospital, while in 2011, all patients seen by the EMS were sent to the emergency department.
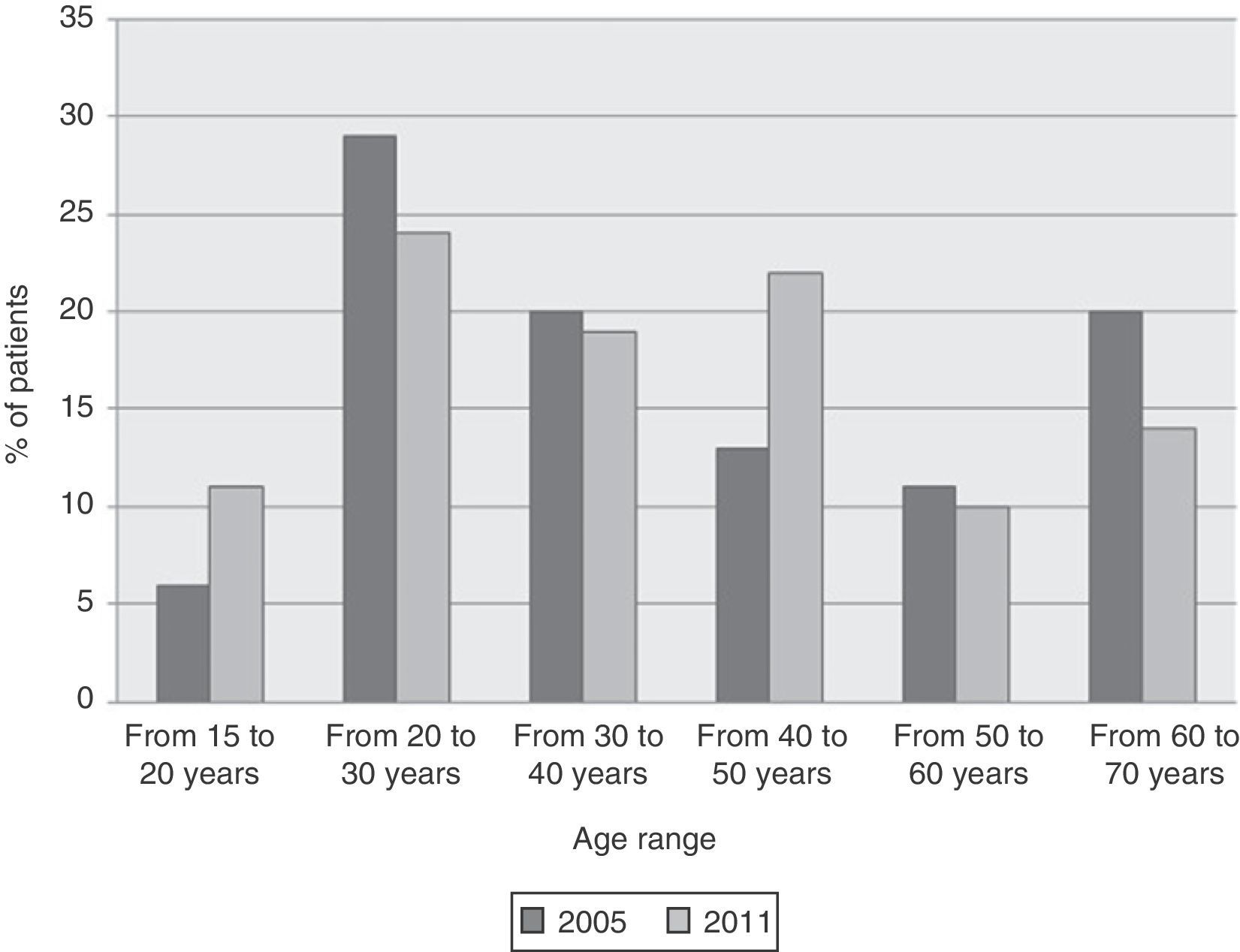
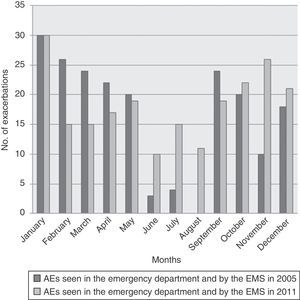
Distribution of the AEs by age is described in Fig. 2. Of the 219 asthmatic patients seen at hospital, 149 (68%) in 2005 and 149/220 (68%) in 2011 were women. In 2005, 62/204 (30%) patients were smokers, 115/204 (57%) were non-smokers, and 27/204 (13%) were former smokers. In 2011, these figures were 61/215 (28%), 139/215 (63%) and 15/215 (7%), respectively.
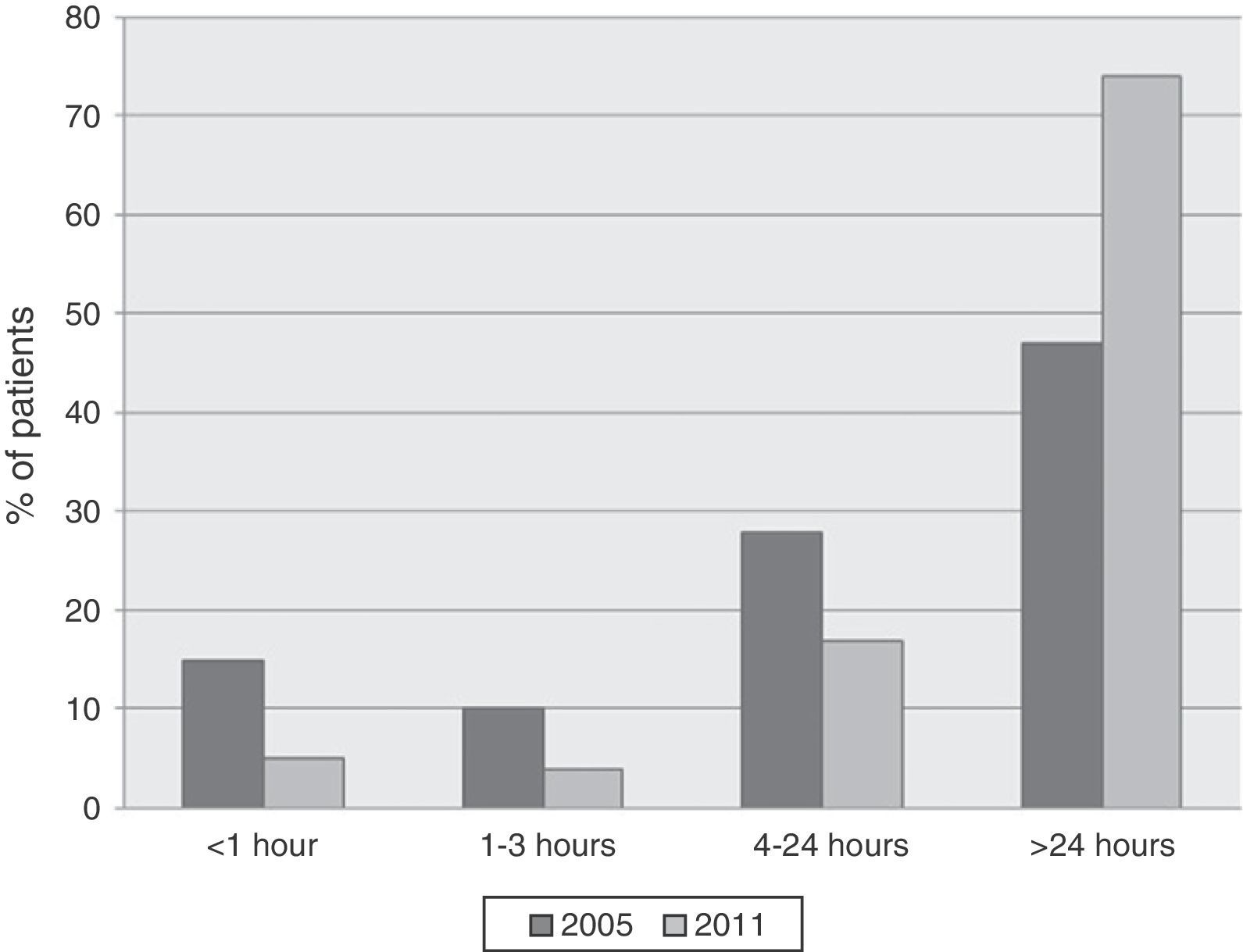
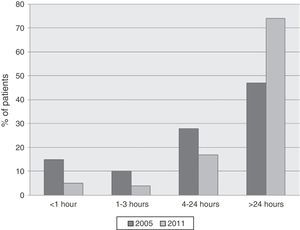
Onset of the ExacerbationThe time of onset of the AE in 2005 (Figure 3) was sudden (less than 1h) in 13%; acute (1–3h) in 10%; between 4 and 24h in 28% and greater than 24h in 49% of patients. In 2011, these figures were 5%, 4%, 17% and 74%, respectively.
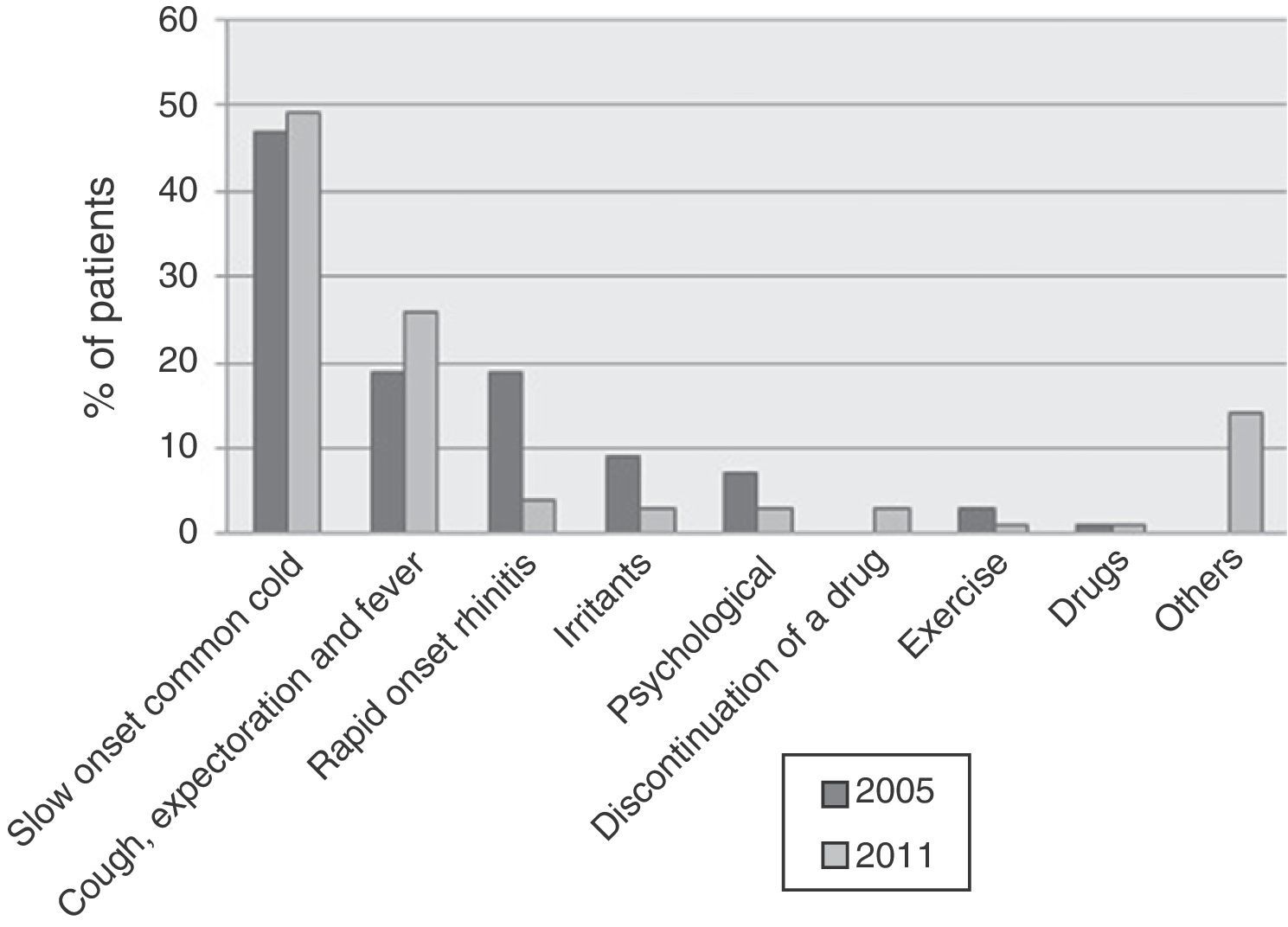
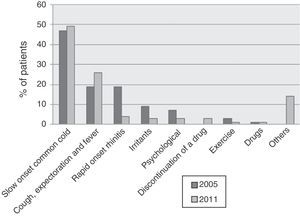
With respect to identification of an AE triggering factor, in 2005 (Fig. 4), 104/219 (47%) had previously suffered a slow onset common cold; 34/219 (16%) had bronchial symptoms with cough, green or yellow expectoration and fever; 33/219 (15%) had rapid onset rhinitis symptoms and sneezing; and 19/219 (9%) had been exposed to an irritant. Seven out of 219 (3%) patients were exercising at the time the AE started. In 19/219 (9%) patients, the trigger was a stressful event, and only 2/219 (1%) patients related the onset of the AE with previously taking medication. None of the flare-ups were attributed to interruption of the anti-asthma medication hours/days earlier. No trigger could be identified in only 1 patient (0.5%). The same data were analyzed in 2011 and are shown in Fig. 4.
DiscussionData from the current study show that the rates of AEs seen in 2005 and 2011, both in the hospital and by the EMS, were 1.93 and 2.0 AE/106 inhabitants/day, respectively, i.e. around 2/106 inhabitants/day. This figure is somewhat lower than the rate found in the earlier studies: 5.3 AE/106 in 20018 and 3.7 AE/106 in 2003.9 However, these latter studies were conducted from November 2001 to February 2002 (ASMAB I),8 and from October to November 2003 (ASMAB II9), both periods with a higher incidence of AEs, while the current studies were both conducted over the course of a year, from January to December. Indeed, the current study, together with ASMAB III and ASMAB IV confirms that the incidence of AEs in the months of November to February and October to November (Fig. 1) is higher than the mean attendance for both years, which, logically, might partly explain the higher rates found in 2001 and 2003. Furthermore, in the studies conducted in 2005 and 2011, patients over 70 years of age were excluded (as it was considered a population in which an AE would be more likely to be confused with an exacerbation of COPD), which would also help to explain in part the low incidence of AE in 2005 and 2011. In fact, 240 AEs were reported in patients aged over 70 years in 2011; therefore, inclusion of this subgroup would give a rate of 4.4 AE/10,6 similar then to the rate obtained in ASMAB I and II. Thus, we can conclude that the incidence of AE remained very similar between 2005 and 2011, and was even comparable to rates found in 20018 and 2003.9
This rate, especially if it has been determined repeatedly over the years (a study which to our knowledge has not been conducted in other cities), could be a useful tool for measuring the degree of control of an asthmatic population. It could also be correlated with the quality of care in a particular area, as better clinical control of patients is known to reduce the number of AEs.12 The difference in the AE rates found in 2005 and 2011 is not significant (P=.960), which could perhaps suggest that asthma control in this population has room for improvement. In fact, despite attempts to restructure services in the primary care sector, even with the establishment of new emergency centers at this level (some even equipped to admit patients for a few hours), the rate of attendance of asthmatic patients in the tertiary hospital remains similar to that in 2005, and even similar to 2001 and 2003.8,9
The cost of treating AEs in hospital emergency departments is known to be 5 times higher than an ordinary consultation13; therefore, at the economic level it is extremely important to determine the number of patients seen in these departments and, logically, take steps to reduce these rates. It is worth mentioning in this respect that many asthmatics believe their disease to be well controlled; however, after detailed study, their degree of control is found to be sub-optimal. This makes them susceptible to flare-ups that put their health at risk and increase the burden on healthcare resources.14 It should also be remembered here that a large majority of asthmatic patients present mild to moderate exacerbations during their lifetime, and that a small percentage of patients develop exacerbations so severe as to be life-threatening.2,15 An appropriate treatment strategy and proper prevention of triggering factors could avert these exacerbations by achieving good control in 71% of patients and complete control in 41%, as achieved the GOAL study.16 Souza-Machado et al. described an 82.3% reduction in hospital admissions for AE in a series of 18,830 patients following introduction of an educational program.17
Determining the incidence or rate of attendance at emergency departments may also be useful in the early detection of sporadic activation of some environmental AE triggering factor. In the 80s, Barcelona suffered a series of AE epidemics which, after a detailed, prospective, systematic study, were attributed to inhalation of soybean dust released during the unloading of soybeans at the city port. On that occasion, the Barcelona Asthma Epidemic Study Group were able to determine that on the non-epidemic days, the mean number of asthmatics who attended the emergency departments at the city's hospitals was around 4 per day, while on some of the epidemic days, this increased to 43,18 and sometimes more. A later case–control study showed the presence of soybean-specific IgG in 74% of asthmatics seen during an epidemic day, compared to 4.6% of those to attended the emergency department on non-epidemic days.19 After installing filters to prevent the soybean dust from being released into the atmosphere, the number of visits to the hospital emergency departments returned to 5 AE/106 inhabitants/day.20 The same monitoring system used in this study could detect AE triggers due to other factors, such as occasional or seasonal increases in atmospheric pollutants,21 which could perhaps explain the differences in the number of AEs found in the summer months of 2005 with respect to 2011.
As regards the clinical characteristics of the 220 asthmatic patients treated in hospital from January to December 2011, 68% were women, a proportion that was identical in the patients studied in 2005. In the studies conducted in 2001 (ASMAB I)8 and 2003 (ASMAB II9), 60% were women. In this study, most the AEs (47% in 2005 and 49% in 2011) were preceded by slow onset common cold of probable viral etiology. Similar associations between asthma and upper respiratory tract viral infections, especially rhinovirus, have been previously described in both children22 and adults.23,24 This could also correlate with the finding that 48% and 65% of patients seen in the emergency department in 2005 and 2011, respectively, claimed the episode had commenced more than 24h earlier, percentages that are somewhat higher even than those found in the studies conducted in 2001 (ASMAB I)8 and 2003 (ASMAB II).9 Salmeron et al. described a series of 3772 AEs in the emergency department, 57% of which had symptoms that had begun more than 24h previously.25
In the absence of specific data, we can only speculate that longer delay before visiting the hospital emergency department in 2011 compared to previous years could be due to some patients being seen previously in other outpatient emergency services. In fact, better health education teaches patients to use the resources closest to them.7 However, this long period prior to being seen could point to, on the one hand, the need to confirm that all asthmatics have a written self-control plan and know what to do in the case of a flare-up, and on the other, sub-optimal access to their primary care center. This suggests that effective action at this level could significantly reduce the number of asthmatic patients seen in hospital emergency departments.
In terms of triggers, in decreasing order of importance, patients reported a previous common cold in about 50% of AE; another group of about 20% reported expectoration and fever, nasal pruritus, rhinorrhea and sneezing probably related to an allergic reaction in about 10%, followed by exposure to an irritant, etc.
One possible limitation of this study may be related to our inability to ascertain whether patients with exacerbations had a rescue strategy. Data were collected from emergency reports, where this information is usually not specified. Another possible limitation may be related to the difficulty in correctly differentiating asthma from COPD, despite omitting patients over 70 years old to reduce errors in this respect.
In conclusion, the results of this study show that the scientific community and health authorities should continue to focus their efforts on improving the background therapy of asthmatic patients and their health education. This would probably reduce the number of visits to hospital emergency departments and improve waiting times. The use of these services is more inconvenient for patients and far more costly for our already overburdened healthcare system.
FundingThis study did not receive any funding.
AuthorsIO participated in the study design, data collection, statistical analysis and writing of the manuscript; TG participated in the study design, data collection, and writing of the manuscript; XM participated in the study design and writing of the manuscript; MAR participated in the statistical analysis and writing of the manuscript; EMM participated in the data collection and writing of the manuscript; FM participated in the study design, data collection, and writing of the manuscript.
Conflict of InterestsThe authors declare that they have no conflict of interests.
To the EMS for providing us with information on patients seen in their home.
Please cite this article as: Ojanguren I, Genover T, Muñoz X, Ramon MA, Moragon EM, Morell F. Incidencia y desencadenantes de las agudizaciones asmáticas atendidas en Urgencias como muestra del nivel asistencial (ASMAB III, 2005 y ASMAB IV, 2011). Arch Bronconeumol. 2016;52:82–87.