Chlamydophila pneumoniae is known to affect the immune response of hosts, but this bacteria has not been described as a cause of autoimmune leukopenia. To our knowledge, this is the first report of a patient with C. pneumoniae pneumonia who developed antineutrophil IgG antibodies.
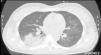
A 37-year-old woman presented with a 1-week history of cough, bloody sputum and fever. Physical examination showed temperature of 38°C and crackles in right lung field. Chest X-ray showed bilateral alveolar infiltrates, corresponding with computed tomography findings of right lower lobe consolidation, and ground glass opacities in left upper lobe and both lower lobes (Fig. 1). ECG was normal. Arterial blood gases: pH: 7.52, PaCO2 34mmHg, PaO2 67mmHg. Clinical laboratory tests: blood glucose 95mg/dl, urea 18mg/dl, creatinine 0.77mg/dl, sodium 139mmol/l, potassium 2.8mmol/l, chloride 98mmol/l, GOT 44U/l, GPT 44U/l, LDH 510U/l, C-reactive protein 287mg/l, procalcitonin 0.18ng/ml, leukocytes 3080μl, neutrophils (76.7%), hemoglobin 10.1g/dl, platelets 222,000μl. Quick time 68%. Microbiology: sputum, blood culture, and pneumococcal and Legionella urinary antigen tests negative. C. pneumoniae serology was positive in acute-phase serum, with elevated antibody titer with seroconversion (17/4/2013 IgG negative [0.157], IgM negative [0.307]; 2/5/2013 IgG indeterminate [0.992], IgM positive [1.428]) on micro-immunofluorescence. During hospitalization, leukopenia worsened to 1770/μl with neutrophil count of 850/μl in the presence of IgG-positive antineutrophil antibodies. Antineutrophil antibodies were detected with fluorescence-labeled polyclonal rabbit anti-human IgM and IgG antibodies (fluorescein isothiocyanate [FITC]) (DAKO). Cell suspension was analyzed using flow cytometry (FACS®, Becton Dickinson). The patient received levofloxacin for 3 weeks, resulting in radiological resolution of the pneumonia and normalization of blood panels.
C. pneumoniae is a Gram-negative bacteria, previously known as Taiwan acute respiratory agent (TWAR). It causes 10% of community-acquired pneumonias (CAP) in Europe (12% of CAPs that do not require hospitalization and 3% of those that do).1,2 It may be responsible for immunological phenomena related to coronary arteriosclerosis,3 but it is unusual for it to cause autoimmune leukopenia associated with antineutrophil IgG antibodies, as occurred in our case.
In autoimmune neutropenia, antibodies develop that act directly against cell membrane antigens, causing peripheral destruction of neutrophils. These antineutrophil antibodies promote phagocytosis of neutrophils opsonized by splenic macrophages.4 Autoimmune neutropenia may be primary or secondary and is more common in adults. It is often related to autoimmune diseases (primary biliary cirrhosis, Sjögren syndrome, lupus erythematosus, and rheumatoid arthritis), as well as to exposure to medication (fludarabine, rituximab), solid tumors and blood cancers, neurological diseases, such as multiple sclerosis, or infections. Viral infections, such as human immunodeficiency virus, es Parvovirus¸ or Epstein–Barr virus, bacteria, such as Helicobacter pylori, Escherichia coli, Neisseria meningitidis, Brucella ssp., Salmonella spp. and Mycobacterium tuberculosis, and other pathogens, including Toxoplasma gondii, Leishmania spp. and malaria, have also been implicated. However, a review of the literature did not yield any report of autoimmune neutropenia developing as a result of C. pneumoniae infection.5
Please cite this article as: Rosario Martín C, Navarro Cubells B, Carrión Valero F. Leucopenia inmunomediada secundaria a neumonía por Chlamidophila pneumoniae. Arch Bronconeumol. 2015;51:663–664.