To evaluate the chest computed tomography (CT) findings of patients with isolated bronchial anthracofibrosis confirmed by bronchoscopy and histopathology.
MethodologyFifty-eight patients with isolated bronchial anthracofibrosis (29 females; mean age, 70 years) were enrolled in this study. The diagnosis of bronchial anthracofibrosis was made based on both bronchoscopy and pathology findings in all patients. The various chest CT images were retrospectively reviewed by two chest radiologists who reached decisions in consensus.
ResultsCentral peribronchial soft tissue thickening (n=37, 63.8%) causing bronchial narrowing (n=37, 63.8%) or obstruction (n=11, 19%) was identified as an important finding on imaging. Multiple bronchial stenoses with concurrent involvement of 2, 3, and 5 bronchi were seen in 12 (21%), 9 (15%), and 2 (3.4%) patients, respectively. Segmental atelectasis and lobar or multilobar collapse were detected. These findings mostly occurred in the right lung, predominantly in the right middle lobe. Mosaic attenuation patterns, scattered parenchymal nodules, nodular patterns, and calcified or non-calcified lymph nodes were also observed.
ConclusionsOn chest CT, isolated bronchial anthracofibrosis appeared as peribronchial soft tissue thickening, bronchial narrowing or obstruction, segmental atelectasis, and lobar or multilobar collapse. The findings were more common in the right side, with simultaneous involvement of multiple bronchi in some patients.
Evaluar los resultados de la tomografía computarizada (TC) de tórax en pacientes con antracofibrosis bronquial aislada demostrada broncoscópica y anatomopatológicamente.
MetodologíaSe incluyó en el estudio a un total de 58 pacientes con antracofibrosis bronquial aislada (29 mujeres; media de edad, 70 años). El diagnóstico de antracofibrosis bronquial se estableció en función de las observaciones broncoscópicas y anatomopatológicas en todos los pacientes. Los diversos aspectos observados en la TC torácica fueron revisados retrospectivamente por 2 radiólogos torácicos, que tomaron las decisiones por consenso.
ResultadosResaltamos el engrosamiento del tejido blando peribronquial central (n=37, 63,8%) como un hallazgo importante en las exploraciones de imagen, que causa estenosis (n=37, 63,8%) u obstrucción bronquial (n=11, 19%). Se observaron múltiples estenosis bronquiales con afectación simultánea de 2, 3 y 5 bronquios en 12 (21%), 9 (15%) y 2 (3,4%) pacientes, respectivamente. Se detectaron atelectasias segmentarias y colapsos lobulares y multilobulares. Estas observaciones se realizaron sobre todo en el pulmón derecho, con un predominio del lóbulo medio derecho. Se observaron también patrones de atenuación en mosaico, nódulos parenquimatosos diseminados, patrones nodulares y ganglios linfáticos calcificados o no calcificados.
ConclusionesEn la TC de tórax, la antracofibrosis bronquial aislada se observa en forma de engrosamiento de tejido blando peribronquial, estenosis u obstrucción bronquiales, atelectasia segmentaria o colapso lobular o multilobular. Estas observaciones fueron más frecuentes en el lado derecho, con múltiples bronquios afectados de manera simultánea en algunos pacientes.
Anthracosis has been regarded as black pigmentation in bronchial mucosa visible at bronchoscopy or based on histological findings, and is characteristically related to the presence of pneumoconiosis or heavy exposure to atmospheric carbon or soot particles. Chung et al. described the term “anthracofibrosis” as dark pigmentation in mucosal layer of bronchi, leading to bronchial narrowing or stenosis.1
Given the prevalence of anthracofibrosis in elderly patients and some similarities in imaging features to those of lung cancer, differentiation may be difficult. Furthermore, causative association between anthracofibrosis and tuberculosis is an issue of ongoing debate, and their imaging findings may interfere with each other.1,2 Hence, familiarity with anthracofibrosis with no concomitant diseases may shed light on the imaging features of this little-known lung disease.
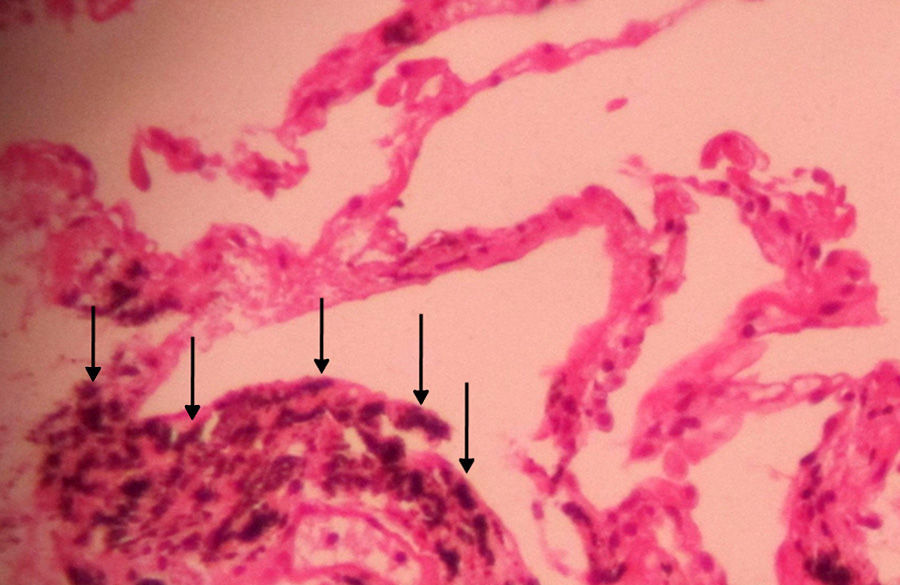
The authors used the term “isolated bronchial anthracofibrosis” to describe bronchial dark tattoos found at bronchoscopic assessment and black pigmentation within the macrophages of bronchial mucosa in patients whose pulmonary evaluation for tuberculosis, neoplasm, or any other apparent lung pathologies was negative. In this study, we attempted to determine and describe the imaging characteristics of bronchoscopically and pathologically proven “isolated bronchial anthracofibrosis” on computed tomography (CT).
MethodologyThis retrospective study was approved by an institutional review board, and informed consent requirement was waived.
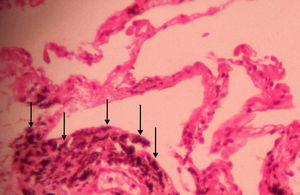
Study SubjectsWe identified 111 consecutive patients with bronchial black pigmentation and bronchial stenosis or obstruction on bronchoscopic examination and bronchial anthracotic pigmentation findings in the histological examination of bronchial biopsy specimens (Fig. 1) from January 2007 to March 2013. Of these, 11 cases were excluded from the study; 7 patients with malignant neoplasm, based on transthoracic (n=2) or transbronchial (n=4) lung biopsy, or pleural biopsy (n=1), 3 with usual interstitial pneumonia, and 1 coal mine worker with a history of anthracosilicotuberculosis. In addition, patients with a medical history, pathologic findings of tuberculosis with or without attributable radiological findings of pulmonary tuberculosis, as well as those with positive sputum smear, culture, or nucleic acid amplification test results for Mycobacterium tuberculosis were excluded. Also, patients with a positive Mantoux test were excluded from the study. Consequently, 25 patients with coexistent active tuberculosis and 17 cases with a history of previous tuberculosis were also excluded from the study. Thereafter, we retrospectively reviewed the imaging findings of the remaining 58 patients; all of them had an available chest CT scan within 0–30 days (mean, 7 days) of bronchoscopic sample. Information about each patient's presenting symptoms and the history of smoking, biomass or dust exposure was obtained from reviewing the medical records.
Image AcquisitionAll examinations were performed with a 4-detector row scanner (LightSpeed QX/I; GE Medical Systems, Milwaukee, USA), and noncontrast helical CT scans were obtained at 5-mm collimation with a helical pitch of 3, 5-mm image intervals, 120kV and 160mAs. All scans were performed from the lung apices to the lung bases, and all images were reviewed using window settings appropriate for mediastinum [window width, 300–450 Hounsfield units (HU); window level, 30–50HU] and lung parenchyma (window width, 1000–1500HU; window level, −600 to −700HU).
Imaging ReviewImaging features were reviewed by two radiologists, each with more than 8 years’ experience interpreting chest CT, in consensus.
Central peribronchial soft tissue thickening, intraparenchymal peribronchial cuffing, bronchial narrowing or obstruction, atelectasis, collapse, lymph node enlargement, consolidation, nodule, nodular pattern, mosaic attenuation pattern, parenchymal band, reticular pattern, pleural effusion or thickening, and any other visible imaging findings as well as the distribution of lesions were included in CT analysis.
Central peribronchial soft tissue thickening was defined as peribronchial wall thickening with soft tissue attenuation at both sides of the bronchus on axial images; while intraparenchymal peribronchial cuffing was regarded as the increased bronchial wall thickness from a segmental level onwards. Visible non-calcified and calcified mediastinal and peribronchial lymph nodes were recorded, and those with a diameter of more than 10mm in short axis were regarded as lymphadenopathies. Pressure effect on immediately adjacent airway by the calcified lymph nodes was also evaluated and recorded. Atelectasis, collapse, consolidation, nodule, nodular pattern, bronchiectasis, parenchymal band, mosaic attenuation pattern, and reticular pattern were defined according to the recommendations of the Nomenclature Committee of the Fleischner Society.3
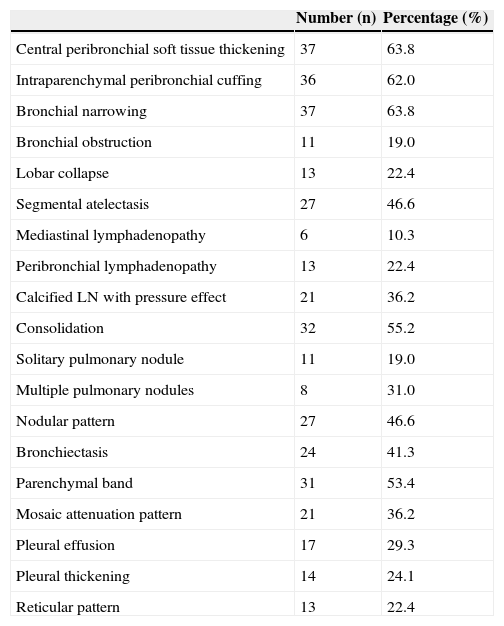
ResultsA total of 58 patients with a mean age of 70 years (range, 29–95 years) and no sex predilection (29 male and 29 female) were included in this study. All patients had cough and/or dyspnea, but no pathological evidence of chronic bronchitis. Twelve patients (20.7%) were active smokers; the others were neither active nor passive smokers. None of the patients had a history of exposure to either biomass or known occupational dust; however, all patients have been living in a city with a large population. The different CT findings of our patients with isolated bronchial anthracofibrosis are summarized in Table 1.
CT Findings in 58 Patients With Isolated Bronchial Anthracofibrosis.
| Number (n) | Percentage (%) | |
|---|---|---|
| Central peribronchial soft tissue thickening | 37 | 63.8 |
| Intraparenchymal peribronchial cuffing | 36 | 62.0 |
| Bronchial narrowing | 37 | 63.8 |
| Bronchial obstruction | 11 | 19.0 |
| Lobar collapse | 13 | 22.4 |
| Segmental atelectasis | 27 | 46.6 |
| Mediastinal lymphadenopathy | 6 | 10.3 |
| Peribronchial lymphadenopathy | 13 | 22.4 |
| Calcified LN with pressure effect | 21 | 36.2 |
| Consolidation | 32 | 55.2 |
| Solitary pulmonary nodule | 11 | 19.0 |
| Multiple pulmonary nodules | 8 | 31.0 |
| Nodular pattern | 27 | 46.6 |
| Bronchiectasis | 24 | 41.3 |
| Parenchymal band | 31 | 53.4 |
| Mosaic attenuation pattern | 21 | 36.2 |
| Pleural effusion | 17 | 29.3 |
| Pleural thickening | 14 | 24.1 |
| Reticular pattern | 13 | 22.4 |
LN: lymph node.
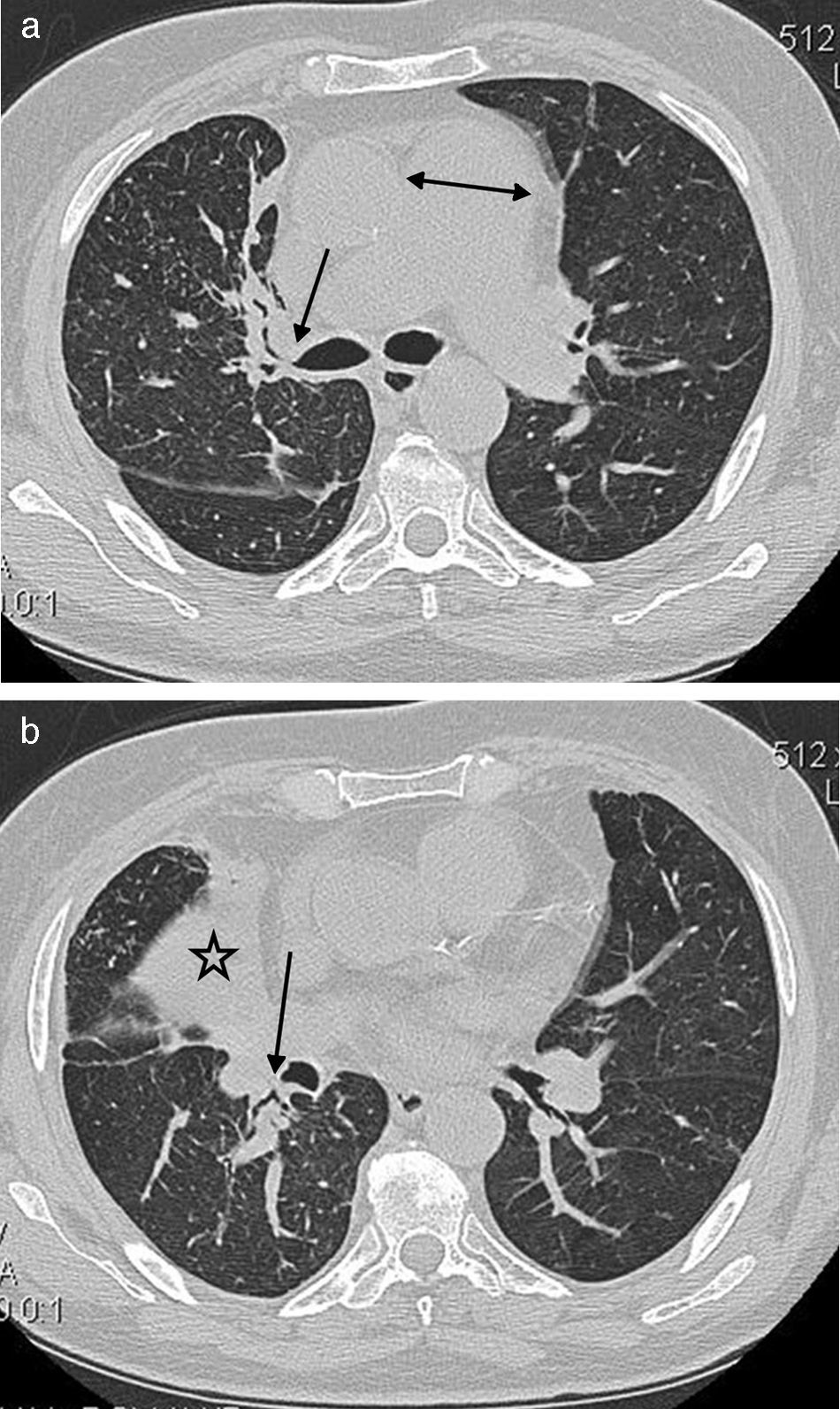
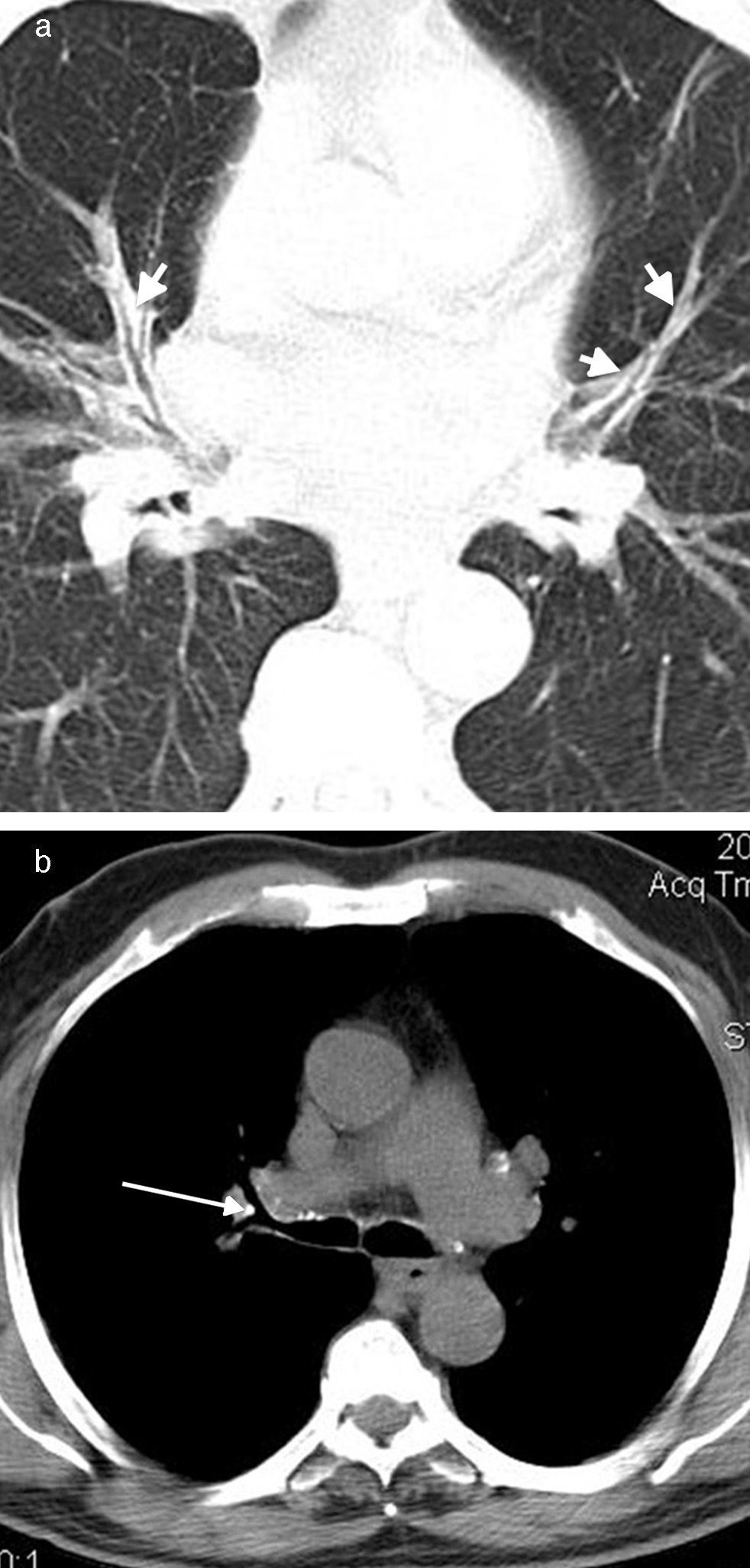
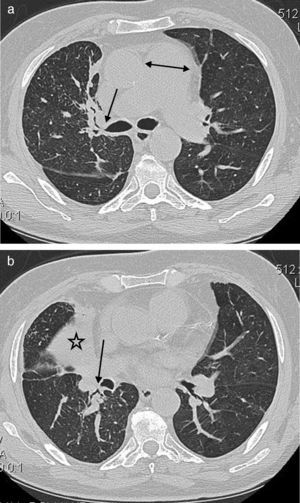
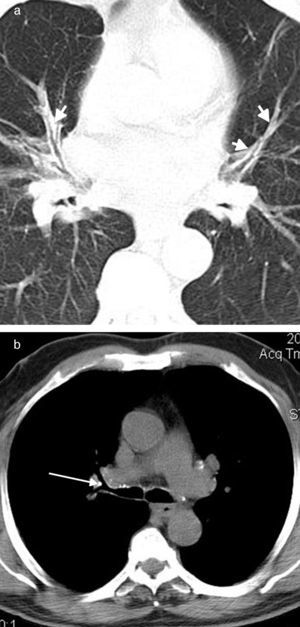
Central peribronchial soft tissue thickening (Fig. 2) was found in 37 (63.8%) cases. It occurred predominantly on the right side [right upper lobe (RUL), n=14; left upper lobe (LUL), n=9; right middle lobe (RML), n=23; lingula, n=7; right lower lobe (RLL), n=19; left lower lobe (LLL), n=10]. Intraparenchymal peribronchial cuffing (Fig. 3a) was seen in 36 (62%) patients with a proclivity to occur on the right side (RUL, n=12; LUL, n=11; RML, n=24; lingula, n=14; RLL, n=27; LLL, n=18). Central peribronchial soft tissue thickening and intraparenchymal peribronchial cuffing were most common in RML and RLL bronchi, respectively.
A 64-year-old male with cough and dyspnea. (a) CT image at the level of main pulmonary artery shows the central peribronchial soft tissue thickening (arrow) and narrowing of RUL bronchus. Also noted is the enlargement of main pulmonary artery (double head arrow). (b) Chest CT with lung window reveals the collapse of RML (star) as well as RLL peribronchial soft tissue thickening (arrow) with obliteration of the apical segmental bronchus of the right lower lobe.
Bronchial narrowing and obstruction were found in 37 (63.8%) and 11 (19%) patients, respectively. Multiple bronchial stenoses occurred in 23 (39.7%) patients (two bronchi, n=12; three bronchi, n=9; five bronchi, n=2). Bronchial stenosis was more prevalent in the right lobes compared to their contralateral counterparts (RUL, n=16; LUL, n=6; RML, n=21; lingula, n=7; RLL, n=14; LLL, n=10).
Likewise, bronchial obstruction was more commonly seen on the right side (RUL, n=3; LUL, n=1; RML, n=7). No bronchial obstruction was detected in lingula, right, or left lower lobes. Interestingly, RML bronchus was most commonly affected by anthracofibrosis with either stenosis or obstruction.
The aforementioned bronchial involvement caused lobar collapse in 13 (22.4%) patients; 2 patients had collapse of two different lobes. Segmental atelectasis was seen in 27 (46.6%) cases, with multisegment involvement being detected in 3 patients.
Visible mediastinal and peribronchial lymph nodes were detected in 56 (96.5%) and 46 (79.3%) patients, respectively; 47 and 39 of whom showed calcified lymph nodes, respectively. Six (10.3%) and 13 (22.4%) patients had mediastinal and peribronchial lymphadenopathies, respectively, with a short axis diameter of more than 10mm. Pressure effect on adjacent bronchi by the calcified lymph nodes was detected in 21 (36.2%) cases (Fig. 3b).
Thirty-two (55.2%) patients showed consolidation, most commonly in the right middle (n=14), right lower (n=13), and left lower (n=13) lobes; among them, 12 patients revealed multilobar consolidations. Solitary and multiple pulmonary nodules were detected in 11 (19%) and 18 (31%) patients, respectively, and nodular pattern was seen in 27 (46.6%) patients. The latter corresponded to innumerable small rounded opacities with a widespread distribution that were discrete and range in diameter from 2 to 10mm.
In addition, bronchiectasis was seen in 24 (41.3%) patients, with the lingula being the most frequent site of involvement (n=9), and 9 (15.5%) patients had bronchiectasis in multiple pulmonary lobes. Other findings included parenchymal bands (n=31, 53.4%), mosaic attenuation pattern (n=21, 36.2%), pleural effusion (n=17, 29.3%), pleural thickening (n=14, 24.1%), and reticular pattern (n=13, 22.4%).
DiscussionTo the authors’ knowledge, the current study constitutes the first report of the CT findings in patients with both bronchoscopically and pathologically proven bronchial anthracofibrosis without any accompanying lung disease; the latter could have had its own interfering manifestations. After excluding those with active and/or old tuberculosis, neoplasm, smoking-related lung diseases, or chronic bronchitis, we described the CT features of the so-called isolated bronchial anthracofibrosis. This study provides evidence that isolated bronchial anthracofibrosis may have some related imaging findings, even in the absence of a coexisting lung disease.
The term “anthracofibrosis” was first introduced in 1997 as bronchial anthracotic pigmentation and associated bronchial stenosis or obliteration in 28 patients.1 The etiology of anthracofibrosis has been an issue of ongoing investigation. Two studies that have focused on the correlation between anthracofibrosis and tuberculosis are described as follows:
A close relation between tuberculosis and anthracofibrosis was described by Kim et al. after evaluation of the imaging features in 54 patients with anthracofibrosis; 32 patients with a history of tuberculosis.4 This hypothesis was suggested based on three evidences; the association of active or old pulmonary tuberculosis with anthracofibrosis, black anthracotic pigment formation during antituberculous treatment, and the similar imaging findings of tuberculosis and anthracofibrosis. Bronchial narrowing or atelectasis was observed in most patients, with the RML bronchus being most commonly involved.
Conversely, the causative role of tuberculosis in anthracofibrosis and consequently empiric antituberculosis treatment in patients with anthracofibrosis were questioned by Park et al.5 They evaluated 43 patients with anthracofibrosis and 32 patients with endobronchial tuberculosis who showed bronchial stenosis based on their CT findings; however, they did not exclude those with a history of old tuberculosis from the group with anthracofibrosis. Seven of 43 patients with anthracofibrosis had either active pulmonary tuberculosis or active tuberculous pleurisy. They found that in contrast to endobronchial tuberculosis, anthracofibrosis was more common among elderly patients. Peribronchial and mediastinal lymphadenopathy, involvement of more lung lobes, bilateral lung involvement, and stenosis of any lobe of the right lung were significantly more common in anthracofibrosis compared to endobronchial tuberculosis. They also found that patients with endobronchial tuberculosis showed contiguous luminal narrowing in main and lobar bronchi; whereas, main bronchus tended to be unaffected in patients with anthracofibrosis. The mentioned differences of anthracofibrosis and endobronchial tuberculosis in their CT features suggested that tuberculosis may not be a causative factor in anthracofibrosis.
With respect to the above-mentioned controversy on the relationship between anthracofibrosis and tuberculosis in the literature, as well as some of the well-described imaging findings related to bronchial involvement in tuberculosis, e.g., mosaic attenuation pattern, tree-in-bud pattern, and bronchiectasis, we excluded the patients with either active tuberculosis or a history of prior tuberculosis from our study to better evaluate the radiological findings of bronchial anthracofibrosis.
Exposure to biomass was also suggested as one of the etiologies of anthracofibrosis.6–8 Kim et al. studied 333 patients with anthracofibrosis and found that all of them had a history of exposure to biomass smoke, and presented with the clinical manifestations of obstructive airway disease.7 Such a high prevalence in prior biomass exposure was not reported elsewhere in the literature. Likewise, in our study, all patients denied any prior biomass exposure; however, the reason for the difference in this regard is unclear.
Despite some suggestions of mixed mineral dust toxicity as a contributory factor for anthracofibrosis,9 a study conducted by Mirsadraee and Saeedi revealed no difference in the prevalence of dust exposure when comparing 41 patients with the simple plaques of anthracosis with 22 cases of anthracofibrosis.10 Likewise, no history of a known occupational dust exposure was elicited by our patients.
Several other studies were also performed to clarify the etiology of anthracofibrosis, and some of them revealed the imaging manifestations of anthracofibrosis; albeit, without exclusion of those with concurrent lung disease.11–20
In our study, isolated bronchial anthracofibrosis occurred predominantly in elderly patients with a mean age of 70 years with no gender predilection. The findings of our study suggest that the encroachment of anthracotic deposits on airways, even in the absence of apparent tuberculosis or other lung diseases, may produce central peribronchial soft tissue thickening or intraparenchymal peribronchial cuffing, and if severe enough, might lead to bronchial narrowing or obliteration and consequently subsegmental, segmental, or lobar atelectasis. The aforementioned findings in bronchial anthracofibrosis at least partially overlap those of lung cancer, especially in elderly patients. However, the multiple sites of involvement with the predominance of RML bronchus may increase the likelihood of anthracofibrosis, especially when the findings are accompanied by the bronchial black pigmentations, visualized at bronchoscopy.
Our study had a number of limitations. First, it was an observational retrospective study based on a relatively small study population sample. However, given the relative rarity of this entity, a prospective evaluation of a large series may not be considered practical. Secondly, the radiologists were not blinded to the bronchoscopic and pathologic findings of the patients, and this could have biased the results of this study. In addition, the bronchoscopic–radiologic correlation of the extent, location, and severity of bronchial stenosis with clinical and imaging follow up may warrant further investigation. Thirdly, biomass or dust exposure was based on patients’ history, and unknown exposure might not be ruled out. Also, as a retrospective analysis, some of the patients might have not been specifically asked about their history of biomass or dust exposure. Fourthly, 5-mm section thickness that was used in this study may be too thick to detect subtle bronchial abnormalities, and a thinner collimation and section thickness may allow a different frequency of findings. Finally, 17 cases with a history of previous tuberculosis were excluded from our study, but it may not be appropriate to rely on a history of previous tuberculosis, particularly when the study design was retrospective. In addition, tuberculosis could have been appeared later in the course of the disease, and the current study cannot indicate lack of relation between tuberculosis and anthracofibrosis; however, this was not the aim of the study. Instead, the purpose was to determine if anthracofibrosis per se could produce any imaging finding.
In conclusion, notwithstanding continuing controversy on etiology of mucosal anthracotic deposits, they may cause bronchial stenosis or obstruction even in the absence of an accompanying lung disease at the time of diagnosis; hence, chest physicians and radiologists should be aware of the imaging findings of isolated bronchial anthracofibrosis as a potential cause of bronchial stenosis or obstruction, most commonly in a multiple and bilateral pattern of involvement. In addition, familiarity with other aforementioned findings, e.g., calcified and non-calcified hilar or mediastinal lymph nodes with pressure effect on adjacent bronchi, will be helpful to reach the correct diagnosis.
Conflict of InterestsThe authors declare that they have no conflict of interests.
None.
Please cite this article as: Kahkouee S, Pourghorban R, Bitarafan M, Najafizadeh K, Makki SSM. Diagnóstico por la imagen de la antracofibrosis bronquial aislada: un análisis de tomografía computarizada de pacientes con confirmación broncoscópica e histológica. Arch Bronconeumol. 2015;51:322–327.