The accommodation of diverse student learning approaches and maintenance of good academic outcomes are often difficult to achieve in university courses, particularly where large classes are concerned.1•3 These issues become even more significant when dealing with first-year students in science and medicine courses with high levels of factual and conceptual content.4•10 Nowadays, the majority of scientific societies, including physiology and medicine, are using video-based lectures for teaching and improving skills of members for several reasons, such as costs of travelling to attend conferences, lack of participation time, elevated costs of organizing conferences, disability of some members, among others (for example, see http://www.ers-education.org/home.aspx). University education programs, such as those offered by University Pierre and Marie Curie (known as UPMC Paris 6), are faced with the challenge of finding innovative ways to accommodate growing interest in medical programs. One of these challenges has been (and still is) to implement video-based lectures for teaching medicine (and physiology). Bearing in mind that the current UPMC-Paris 6 medical educational system is based almost entirely on face-to-face teaching methods, the question arises as to whether video-based lectures could be used to complement and corroborate traditional classroom-based courses and small-group tutorials, or to replace them to a certain extent in special circumstances (cost of travelling to attend classes, disability of some students, among others). Video-based lectures could also be used to help medical students prepare for tests (written and/or oral), as well as the National Board and Post-graduate Specialty Examinations (which give access to medical postgraduate specialties, such as cardiology, pulmonology, internal medicine and others) by effectively refreshing the student's knowledge of medicine and physiology.
Twenty second-year volunteer graduate medical students were recruited from a teaching unit (UE) coordinated by Prof. Christian Straus and Pierantonio Laveneziana (UPMC Paris 6) and held in April 2015 at the Faculty of Medicine of University Paris 6 (Sorbonne Universitèc)s, Universitèc) Pierre et Marie Curie • Paris 6). The choice of the topic “respiratory physiology” was based on a common observation that teaching (from the professors tm) point of view) and learning (from the students tm) point of view) respiratory physiology is at times more complicated than other disciplines.
The medical students who participated in the UE had previously attended the traditional classroom-based courses/lectures in respiratory physiology (from September to November 2014 of the second year of the graduate medical education program), where these items were fully explored. During the second year of medicine, at least at UPMC in Paris, professors teach 12h of respiratory physiology, of which 30•45min are dedicated to spirometry and lung volumes in healthy individuals. It should be noted that the students did not receive any medical education or courses over the summer preceding the video evaluation.
Eight professors of physiology were each asked to record a video-based lecture on spirometry and lung volumes in healthy individuals lasting 3•5min. In order to standardize and homogenize the content of these video-based lectures, each professor was also informed about the content of the multiple choice questions (MCQ) that students would be tested on. None of the students was directly instructed by any of the volunteer lecturers. The learning objectives were the understanding of flow-volume loop and lung volumes. The objective was not to evaluate the performance of the professors, but rather to assess the impact, if any, of a different pedagogical teaching/approach to such a difficult topic as flow-volume loop and lung volumes measurements on learning outcomes, and whether this process may or may not help in preparing for oral and/or written exams such as the National Board and the Specialty Examinations. The 8 videos were peer reviewed by the authors of this editorial for consistency and quality of content.
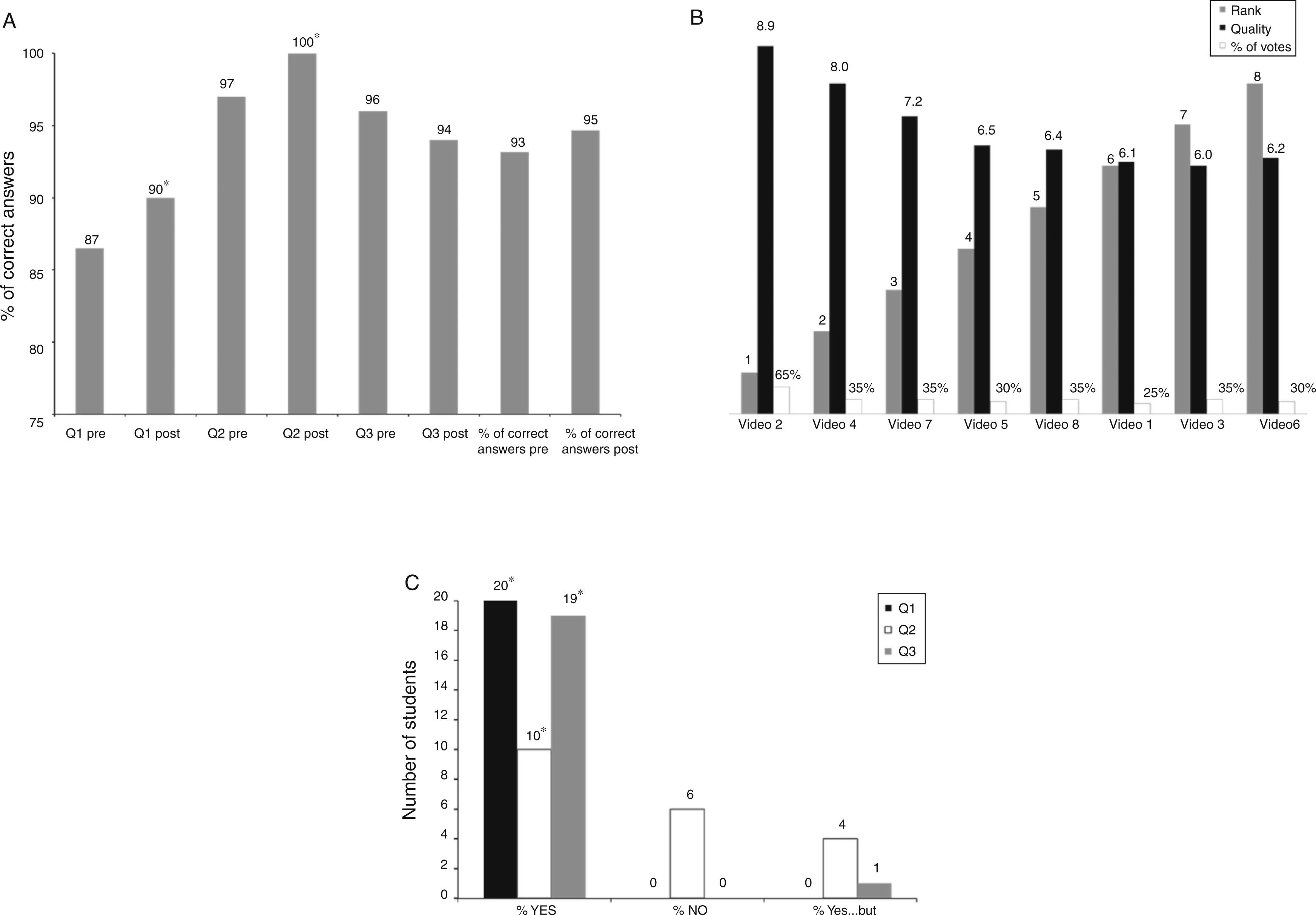
At the end of each teaching session, students were asked to assess each video-based lecture, as shown in Fig. 1B.
Panel A: The percentage of correct answers to multiple choice questions after watching the videos statistically improved in Question 1 (Q1) and Question 2 (Q2) but not in Question 3 (Q3). Globally, the percentage of total correct answers to multiple choice questions after watching the videos did not statistically improve, although there was a tendency towards improvement. Please refer to the text for more detailed information. *p<0.05 (McNemar's exact test) comparison between pre and post videos; panel B: evaluation of the video-based lectures. The quality of the content/information of each video-based lecture was scored from 0=inacceptable to 10=excellent, while the pedagogical and teaching quality of each video-based lecture was scored in descending order from 1=the best to 8=the worst. The quality (black columns) of the content/information of each video-based lecture was above 5. The pedagogical and teaching quality assessment (i.e. grey columns from 1 to 8) is shown: for privacy reason the first/last name and institution of each teacher have been removed and replaced by the order in which the videos were showed to the students. This evaluation revealed that video-based lecture #2 was ranked first in terms of pedagogical and teaching quality. White columns show the percentage (%) of votes that each video obtained from the students. Video-based lecture #2 was voted by 65% of the medical students as being the best. This was corroborated by the highest score the concomitant video-based lecture obtained; panel C: questionnaire evaluating the value of the project. At the end of the eight video-based lectures, each medical student was asked to fill in a questionnaire composed of the following questions (Q): Q1: Do you find the video-based lecture helpful in the teaching of physiology?; Q2: Do you think the video-based lectures could eventually replace traditional classroom-based courses?; Q3: Do you find the video-based lecture helpful in the preparation of the National Board and Post-graduate Specialty Examinations for accessing medical postgraduate studies? The figure shows that all the recruited medical students (n=20) found the video-based lectures helpful in the teaching of respiratory physiology. Half of the medical students (n=10) thought that the video-based lectures could eventually replace official and traditional classroom-based courses, while 6 students thought the opposite (video-based lectures could never replace traditional classroom-based courses), and 4 students thought that video-based lectures could complement and eventually help elucidate the content covered by traditional classroom-based courses. Almost all (19) students found the video-based lecture helpful in the preparation of the National Board and Post-graduate Specialty Examinations.
Students were simply asked to judge the overall quality of the information/content being delivered, and to classify the videos based on the ability of each video/teacher to deliver clear and non-ambiguous information on the study topic. Students were only allowed to watch the videos once.
Each student was asked to answer 3 multiple choice questions (MCQ) before and after watching the 8 study videos. The multiple choice questions were defined by consensus, and all contributors found the questions challenging enough to permit researchers to detect a meaningful improvement after viewing the video. Students answered the questions in isolation.
At the end of the 8 video-based lectures, each medical student was asked to fill in a questionnaire composed of 3 questions (Q), as shown in Fig. 1C.
Results are expressed as mean±SD, unless otherwise specified. A p<0.05 level of statistical significance was used for all analyses. McNemar's exact test was used to evaluate changes in the percentage of correct MCQ answers given by each student after watching the videos.
A statistically significant change in the percentage of correct answers to Q1 and Q2 was observed after watching the videos, but not to Q3 (Fig. 1A).
The pedagogical and teaching quality of the content/information of each video-based lecture obtained a score of over 5, as shown in Fig. 1B.
The results of the questionnaire evaluating the value of the project are summarized in Fig. 1C.
There is a growing body of empirical evidence on the influence of computer-assisted learning on academic attainment, particularly the use of video-based teaching materials within traditional classroom-based courses.1•4,9 Nowadays, the majority of scientific societies, including physiology and medicine, use video-based lectures for teaching and improving the skills of members for several reasons, such as costs of travelling to attend conferences, lack of participation time, elevated cost of organizing conferences, disability of some members, among others (for example, see http://www.ers-education.org/home.aspx). Our study revealed that teaching human respiratory physiology courses using video-based lectures was nearly as effective as classroom-based teaching in terms of test results: the video format was impactful and helped reinforce the principles already taught (Fig. 1A). The question now arises as to whether these 20 volunteers were top students in their class; if so, reviewing/refreshing respiratory physiology using the videos would have had little or no effect on their performance. This does not seem to be the case, because in these 20 students the overall average score for respiratory physiology and pulmonology as taught in the first semester was just 14/20, which is by no means an impressive achievement. This suggests that a learning ceiling effect is unlikely, because the students still had much room for improvement after watching videos.
All medical students recruited found the video-based lectures helpful in teaching respiratory physiology, and 50% of them thought that video-based lectures could eventually replace traditional classroom-based courses (Fig. 1C); this is in line with the current literature.1•4,9 However, a word of caution should be used here, since 30% of the students recruited thought the opposite (video-based lectures could never replace traditional classroom-based courses), while 20% of them thought that video-based lectures could complement and eventually help elucidate the content covered by traditional classroom-based courses. Almost all (95%) study students found the video-based lecture helpful in the preparation of the National Board and Post-graduate Specialty Examinations (Fig. 1C). This, albeit in a very preliminary way, shows that video-based lectures might be more effective than the traditional method of teaching human respiratory physiology for medical students, and is in line with the current literature.1•3
Finally, there is ample evidence that different teaching styles and/or approaches may influence student academic performance in different ways. Specifically, it has been suggested that video-based technology may enhance the student learning pattern.4•10 This was apparently the case in this study, and was reflected by the evaluation of the quality of the content/information and the pedagogical and teaching quality of each video-based lecture (Fig. 1B).
These findings, albeit preliminary, are highly relevant not only for UPMC-Paris 6 but also for the international higher education community, because we provide valuable insight into the potential role of self-directed technology-based learning (in this case 3•5min videos on spirometry and lung volumes) at a time when medical curricula and assessments are being redesigned in Europe and the United States of America.
In addition, a dedicated platform for accessing on line applications/websites where professors can be consulted by students is a feasible and promising application for supporting e-learning.
As such, this project may pave the way for European and worldwide university medical programs relying more on the recording of video-based lectures to complement but not entirely replace the more traditional classroom-based courses.
AuthorshipAll authors meet all of the ICMJE criteria for authorship. All authors gave final approval to the submitted paper.
A special thanks goes to all the professors of physiology who agreed to record the video-based lectures (Thierry Perez, Bruno Degano, Gilles Garcia, Arnaud Chambellan, Marie-Hèc)lène Becquemin, Christophe Delclaux and Frèc)dèc)ric Costes) and all medical students who contributed to this project.