Studies on the relationship of chronic obstructive pulmonary disease (COPD) prevalence and altitude have reported contrasting results. The aim of this COPD case-finding study was to include a larger number of geographical sites to determine if there is an association between altitude and COPD prevalence.
Patients and methodsIndividuals aged 40 or older with known COPD risk factors, whether symptomatic or not, were referred by primary-care physicians. After obtaining written informed consent, they were invited to answer a questionnaire and undergo pre- and post-bronchodilator spirometry.
ResultsSubjects were recruited in 27 Mexican cities, within an altitude range from 1 to 2680m above sea level. We found a weak (−0.31; P<.0001) although significant negative correlation between altitude and COPD prevalence. The COPD rate for cities located ≤1000m was 32.7% vs 16.4% for cities located >1000m (P<.0001); the rate for cities located at ≤2000m was 22.7% vs 15.6% for those >2000m; in the multiple logistic regression analysis, older age, male sex, tobacco habit, pack-years of smoking, years of exposure to biomass smoke, and city altitude over sea level were significantly associated with COPD prevalence.
ConclusionsOur data shows a significant inverse correlation between prevalence/severity of COPD and altitude.
Los estudios sobre la relación entre la prevalencia de la enfermedad pulmonar obstructiva crónica (EPOC) y la altitud han presentado resultados contradictorios. El objetivo de este estudio de identificación de casos de EPOC fue incluir un número elevado de localizaciones geográficas para determinar si hay una asociación entre la altitud y la prevalencia de la EPOC.
Pacientes y métodosLos pacientes de edad igual o superior a 40 años con factores de riesgo conocidos para la EPOC, sintomáticos o no, fueron remitidos por los médicos con quienes tenían el primer contacto. Tras obtener un consentimiento informado por escrito, se les invitó a responder a un cuestionario y se les realizó una espirometría previa y posterior a la administración de broncodilatador.
ResultadosLos participantes fueron reclutados en 27 ciudades de México, con un rango de altitudes que iba de 1 a 2.680m sobre el nivel del mar. Observamos una correlación negativa débil (–0,31; p<0,0001) aunque significativa entre la altitud y la prevalencia de la EPOC. La tasa de EPOC en las ciudades situadas a ≤1.000m fue del 32,7%, frente al 16,4% observado en las ciudades situadas a >1.000m (p<0,0001); la tasa observada en las ciudades situadas a ≤2.000m fue del 22,7%, frente al 15,6% de las situadas a >2.000m; en el análisis de regresión logística múltiple, la edad creciente, el sexo masculino, el haber fumado en algún momento, los paquetes-años de tabaquismo, los años de exposición al humo de la biomasa y la altitud de la ciudad sobre el nivel del mar mostraron una asociación significativa con la prevalencia de la EPOC.
ConclusionesNuestros datos muestran una correlación inversa significativa entre la prevalencia/gravedad de la EPOC y la altitud.
Chronic obstructive pulmonary disease (COPD) is an important cause of morbidity and mortality throughout the world that is frequently underdiagnosed and undertreated.1 Male sex, older age, cigarette consumption, work exposure, and low income level are well-known independent risk factors for COPD.2
It has been said that altitude above sea level may be a significant factor that influences the prevalence of COPD. However, studies about the relationship between the prevalence of COPD and altitude have presented contradictory results. The PLATINO study, in which 5 Latin American cities participated, observed a perfect negative correlation between COPD and altitude, demonstrating that the highest rate was Montevideo (19.7%), at 35m above sea level, and the lowest was Ciudad de México (78%), at 2240m above sea level.1 Apart from this, the PREPOCOL study, which included 5 Colombian cities with altitudes between 18 and 2640m above sea level, indicated that the higher altitude was associated with a higher prevalence of COPD.2 Thus, the role of altitude in the appearance of COPD and its later evolution is a field in which more research could be beneficial.3
Our objective was to determine the association between altitude and the prevalence and severity of COPD in individuals with risk factors and/or symptoms that are compatible with COPD in 27 Mexican cities.
Patients and MethodsThe methodology used for this study has been previously published.4 Briefly, the study was carried out between March and October 2008. The participants were recruited in 27 cities in 20 different Mexican states. The cities were chosen according to the availability of a licensed respiratory therapist who could administer a questionnaire and perform a spirometry.
In each city, family physicians were invited to participate in a strategy in order to identify cases of individuals with possible COPD. We decided to make a selection through the primary care physicians in order to reduce selection bias associated with a selection done by pulmonologists.
We contacted family physicians from each city through the corresponding local medical society. Telephone calls were made to contact the patients and make appointments for the spirometry and questionnaire. The participants responded to a self-administered, 4-question survey about COPD risk factors (smoking, exposure to biomass smoke, and/or dust) and COPD symptoms (cough, sputum production, and dyspnea). The individuals who gave one or more affirmative answers were remitted for spirometry. The study was approved by the ethics committee of the health-care services of the state of Baja California (México).
After obtaining written informed consent, the patients were invited to answer the Spanish version of the PLATINO questionnaire.5 The following information was collected for all participants: demographic characteristics, occupational exposure to dust, history of smoking, passive smoking, and domestic exposure to biomass smoke. For consumption of cigarettes, both current and previous uses were registered. The history of occupational exposure to dust was registered as either present or absent; for those with positive histories, the number of years of exposure was also registered. The history of passive smoking was registered as either present or absent; for those with positive histories, the number of years of exposure was also registered.
Exposure to biomass smoke was registered as either present or absent; for those with positive histories, the hours per day and years of exposure were registered.
Dyspnea was evaluated with the Medical Research Council (MRC) dyspnea scale.6
Spirometric determinations before and after the administration of a bronchodilator were done with a battery-run portable spirometer (Easy-One; NDD Medical Technologies, Chelmsford, MA, USA and Zurich, Switzerland). Spirometries were done according to the quality criteria of the American Thoracic Society and the European Respiratory Society (ATS/ERS).7 The post-bronchodilator (PBD) test was done after 4 doses of 100μg of albuterol. The reference equations used were those by NHANES III for North Americans of Mexican origin.8 We used the GOLD criteria9 for PBD FEV1/FVC<0.7 to define COPD.
The cases were stratified according to PBD FEV1 as either mild (FEV1≥80% predicted), moderate (FEV1 50%≤FEV1<80% predicted), severe (FEV1 30%≤FEV1<50% predicted) or very severe (FEV1<30%).
SpO2 was determined with a pulse-oximeter (Diagnostix™ 2100 Digital Fingertip Pulse Oximeter, Hauppauge, NY, USA). The oximeter was placed on the right index finger of the patient and all the patients breathed room air during the test. The average of 3 determinations was taken. The data on the altitude above sea level of the cities was obtained from the National Institute of Statistics and Geography (INEGI).10 For the analysis, a mean of the topographic data for each city was used.
Statistical AnalysisThe descriptive statistics were calculated (for example, distributions of frequencies for the discrete variables as well as mean, standard deviation, and ranges for the continuous variables) in order to describe the characteristics of the participants. Student's t and χ2 tests were used to evaluate the differences among the groups. Means±standard deviation of the mean (with 95% confidence intervals [CI95%]) is presented as well as the odds ratios (OR) and the CI95%, when appropriate. All the comparisons are bilateral and a result was considered to reach statistical significance if the P value was less than .05.
Multivariable Logistic RegressionAfter carrying out a univariate analysis, a logistic regression model was constructed with the variables that showed a P value <.1 in the univariate analysis. A scaled multivariable logistic regression test was used to evaluate diverse variables (both numerical as well as discrete) with the aim of finding the best model for predicting the presence or absence of airway obstruction (defined as PBD FEV1/FVC<70%). The factors included in the regression model are the following: age, sex (males vs females), body mass index (BMI), MRC dyspnea score, smoking (at some time vs never), cigarettes smoked per day, hours per day exposed to biomass smoke, years exposed to biomass smoke and altitude of the city above sea level in meters. The statistical analyses were done with the SPSS® program (version 18.0; SPSS Corporation, Chicago, IL, USA).
ResultsThe participants were recruited in 27 Mexican cities, with an altitude above sea level ranging between 1 and 2680m (Table 1).
Cities and Altitude Above Sea Level.
| City | State | Altitude, m | Number of Participants |
| Aguascalientes | Aguascalientes | 1987 | 59 |
| Campeche | Campeche | 40 | 52 |
| Cancún | Quintana Roo | 8 | 50 |
| Celaya | Guanajuato | 1730 | 58 |
| Ciudad de México | Distrito Federal | 2240 | 413 |
| Ciudad Madero | Tamaulipas | 5 | 20 |
| Ciudad Victoria | Tamaulipas | 320 | 59 |
| Cuernavaca | Morelos | 1480 | 92 |
| Culiacán | Sinaloa | 54 | 51 |
| Hermosillo | Sonora | 210 | 57 |
| Ciudad Obregón | Sonora | 40 | 112 |
| Guadalajara | Jalisco | 1586 | 257 |
| Irapuato | Guanajuato | 1730 | 115 |
| León | Guanajuato | 1800 | 58 |
| Mazatlán | Sinaloa | 1 | 69 |
| Mérida | Yucatán | 9 | 75 |
| Monterrey | Nuevo León | 537 | 132 |
| Morelia | Michoacán | 1921 | 84 |
| Pachuca | Hidalgo | 2395 | 59 |
| Puebla | Puebla | 2175 | 154 |
| Puerto Vallarta | Jalisco | 10 | 53 |
| Querétaro | Querétaro | 1825 | 128 |
| Saltillo | Coahuila | 1700 | 131 |
| San Luis Potosí | San Luis Potosí | 1860 | 106 |
| Tampico | Tamaulipas | 5 | 59 |
| Tepic | Nayarit | 930 | 53 |
| Toluca | Estado de México | 2600 | 57 |
A total of 2617 individuals were remitted for evaluation. In 2293 (87.6%), acceptable spirometer maneuvers were recorded (at least 3 reproducible FVC and FEV1 maneuvers with differences of less than 150ml) and 472 of them (20.6%) presented an FEV1/FVC value <70%. According to the GOLD classification, 20.3% had mild COPD, 46.0% moderate COPD, 26.1% severe COPD, and 7.6% presented very severe COPD.
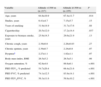
Upon comparing the demographic and clinical characteristics of the participants who lived at an altitude of less than 1300m (average altitude) with the characteristics of participants who lived above 1300m, we observed that the individuals with COPD who lived at an altitude <1300m had FEV1, FVC, and FEV1/FVC values that were significantly lower than those of individuals who lived at altitudes ≥1300. Meanwhile, the oxygen saturation was significantly lower in individuals who lived at higher altitudes (Table 2A).
Demographic Characteristics and Clinical Variables According to the Altitude Above Sea Level in Patients With Chronic Obstructive Pulmonary Disease (COPD) (Average Height, 1300m).
| Variable | Altitude <1300m (n=217) | Altitude ≥1300m (n=255) | P |
| Age, years | 64.8±10.9 | 67.4±11.7 | .014 |
| Studies, years | 6.41±4.7 | 7.15±5.7 | .15 |
| Years of smoking | 31.9±14.9 | 31.7±17.6 | .88 |
| Cigarettes/day | 20.5±12.0 | 17.2±14.4 | .037 |
| Exposure to biomass smoke, years | 25.9±14.5 | 29.6±21.9 | .13 |
| Chronic cough, years | 2.38±0.8 | 2.28±0.83 | .27 |
| Chronic sputum, years | 2.39±0.7 | 2.24±0.8 | .07 |
| Dyspneaa | 2.27±1.1 | 1.82±1.1 | .07 |
| Body mass index, BMI | 26.5±5.2 | 26.5±5.1 | .98 |
| Oxygen saturation, % | 92.8±4.8 | 89.8±6.1 | <.001 |
| PBD FEV1, % predicted | 54.7±20.4 | 66.4±21.6 | <.001 |
| PBD FVC, % predicted | 74.1±12.5 | 83.9±14.1 | <.001 |
| PBD FEV1/FVC, % | 56.3±11.6 | 59.8±10.2 | <.001 |
PBD: post-bronchodilator.
These results were similar in individuals without airway obstruction, except those for the PBD FEV1/FVC ratio (Table 2B).
Demographic Characteristics and Clinical Variables According to Altitude Above Sea Level in Individuals Without Chronic Obstructive Pulmonary Disease (COPD) (n=1821; Average Altitude, 1300m).
| Variable | Altitude <1.300m (n=473) | Altitude ≥1.300m (n=1.348) | P |
| Age, years | 55.1±24.8 | 55.7±11.7 | .56 |
| Studies, years | 9.73±4.8 | 8.55±5.3 | <.001 |
| Years of smoking | 25.1±10.8 | 22.3±12.5 | .001 |
| Cigarettes/day | 18.6±10.6 | 11.2±9.6 | <.001 |
| Exposure to biomass smoke, years | 19.2±11.5 | 20.3±24.4 | .58 |
| Chronic cough, years | 2.13±0.87 | 1.90±0.86 | <.01 |
| Chronic sputum, years | 2.67±6.8 | 2.24±0.8 | .07 |
| Dyspneaa | 2.27±1.1 | 1.83±0.85 | .002 |
| Body mass index, BMI | 29.1±5.9 | 28.3±4.8 | .008 |
| Oxygen saturation, % | 95.4±2.9 | 92.8±4.0 | <.001 |
| PBD FEV1, % predicted | 87.2±17.5 | 93.1±18.6 | <.001 |
| PBD FVC, % predicted | 85.7±16.3 | 90.3±16.9 | <.001 |
| PBD FEV1/FVC, % | 80.4±7.93 | 81.4±27.6 | .45 |
PBD: post-bronchodilator.
We observed a weak although significant negative correlation (−0.31; P<.0001) between altitude and the prevalence of COPD. The COPD rate in the cities situated at <10m above sea level (Cancun, Ciudad Madero, Mazatlan, Merida, and Puerto Vallarta) was 31.3%, compared with 15.7% of the cities situated at more than 2000m above sea level (Puebla, Mexico City, Pachuca, and Toluca; P<.0001). Globally, the COPD rate in cities situated at ≤1000m was 32.7%, vs 16.4% for cities situated at >1000m (P<.0001); the rate observed in cities situated at ≤2000m was 22.7%, vs 15.6% in the cities situated at >2000m (Tables 3 and 4).
Altitude and Prevalence of Chronic Obstructive Pulmonary Disease (COPD) in México. Cities at an Altitude <1000m vs ≥1000m.
| Variable | Absence of COPD | COPD | Total |
| Altitude <1000m | 413 (67.9%) | 195 (32.1%)a | 608 |
| Altitude ≥1000m | 1408 (83.6%) | 277 (16.4%) | 1685 |
| Total | 1821 (79.4%) | 472 (20.6%) | 2293 |
Altitude and Prevalence of Chronic Obstructive Pulmonary Disease (COPD)in Mexico. Cities at Altitudes <2000m vs ≥2000m.
| Variable | Absence of COPD | COPD | Total |
| Altitude <2.000m | 1238 (77.3%) | 364 (22.7%)a | 1602 |
| Altitude ≥2.000m | 583 (84.4%) | 108 (15.6%) | 691 |
| Total | 1821 (79.4%) | 472 (20.6%) | 2293 |
The oxygen saturation determined with pulse-oximetry showed a significant negative correlation with altitude (Spearman's rho: −0.410, P<.001). The ANOVA analysis showed a significant reduction in oxygen for the progressively higher levels of COPD severity (mild: 92.7%; moderate: 91.8%; severe: 89.5%; very severe: 88.6, P<.001).
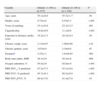
In the multiple logistic regression analysis, the variables of age, male sex, smoking at some time, pack-years, years of exposure to biomass smoke, and altitude of the city above sea level showed a significant association with the prevalence of COPD (Table 5).
Multivariate Logistic Regression Analysis: Predictive Factors of the Airway Obstruction (Post-Bronchodilator FEV1/FVC Ratio <70%).
| Variable | Adjusted OR (95% CI) | P value |
| Age, in 10-year increments | 2.0 (1.2–2.5) | <.001 |
| Sex (males–females) | 1.8 (1.4–2.6) | .02 |
| Smoker at some time vs never | 2.3 (1.6–2.6) | <.01 |
| Pack-years, 10-year increment | 1.6 (1.3–2.0) | .02 |
| Exposure to biomass smoke, 10-year increments | 1.3 (1.1–2.0) | .03 |
| Altitude above sea level, m | 1.1 (1.0–1.3) | <.05 |
CI: confidence interval; OR: odds ratio.
As mentioned, the PLATINO study showed a perfect correlation between the order of altitude of the 5 cities included in the study and gross COPD rates.1 Conversely, Caballero et al.2 indicated that higher altitude was associated with a greater prevalence of COPD. The logistic regression analysis showed positive association between altitude and the prevalence of COPD (higher altitude, greater prevalence); however, when Bogota, the city at the highest altitude (2640m), was compared with Barranquilla, the city at the lowest altitude (18m), the association was not significant.
In the PLATINO study, the 5 sites were in different countries, while in PREPOCOL they were all cities of the same country. Therefore, in the PLATINO study there is the possibility that differences between the countries may be partially responsible for what was perceived as a difference related with altitude.3 As in the PLATINO study, this present study has observed, with 27 reference points for altitude in the same country, a significant negative correlation (although much weaker) between altitude and COPD prevalence.
The reasons for the lower prevalence of COPD at higher altitudes have still not been established. Altitude could induce a greater growth of the airways compared with lung size, giving rise to an increase of the FEV1/FVC proportion.1 In addition, in individuals studied at different altitudes, there is some evidence that indicates that the lower density of the air existing at a greater altitude could modify the results of the lung function tests, as researchers have observed that the FVC is slightly lower and the FEV1 is slightly higher.11 This would have a net effect of increasing the FEV1/FVC ratio with altitude, with the net result of a lower COPD rate at higher altitudes. Another study has also suggested that asthma rates are also lower at higher altitudes.12
On the other hand, it is also possible that the lower atmospheric pressure and relative hypoxemia may contribute to other comorbidities, such as pulmonary hypertension and congestive heart failure in patients who live at great altitudes, with the possible consequence of earlier mortality in that population.13
Altitude is one of the main determining factors of hypoxemia.14 Sherpas, who live at an average altitude of 4000m, have spirometric values that are significantly higher than Caucasians, with a relative increase of approximately 12%. Over time and many generations, Sherpas have developed physiological and genetic modifications, and they now show spirometric values higher than populations that live at lower altitudes; this could be part of their respiratory adaptation to extreme heights in response to chronic hypoxia and usually high levels of exercise.15
Lung function studies have also been done in individuals of Ladakhi and Tibet who live at altitudes between 3300 and 4500m. The spirometric results of both groups showed higher values of maximum mid-expiratory flow (MMEF), which were between 130 and 150% of the predicted value, compared with 85% in control subjects, with an FEV1/FVC ratio of 115%, compared with 98% in the controls. These results could constitute an important adaptation to a life-long sustained increase of ventilation at rest.16
An alternative explanation would be that this observation corresponded with auto-selection phenomena, meaning that COPD patients (especially those affected by more advanced disease) moved to lower altitudes with higher oxygen pressure. As our study is cross-sectional, we cannot establish causal inferences for this hypothesis.
The study has certain limitations.4 We did not use a random population sample, as the patients were remitted by primary-care physicians due to suspicion of COPD. However, as was indicated, we had opted for this approach with the aim of reducing the selection bias associated with a selection done by pulmonologists.
Moreover, the number of individuals recruited in the different cities would seem to be unbalanced; however, this distribution was designed in order to have percentages that were more representative of the population of each city (for example, Mexico City has a population of 8 million, while the population of Ciudad Madero is only 200000). The number of participants who lived at an altitude <1000m constitutes only one-third of the total sample; this is due to the fact that almost all the larger cities in México are situated on a plateau that is >1500m above sea level.
We used the set FEV1/FVC ratio to define the presence of COPD according to the GOLD guidelines,9 a definition which continues to be current. There is intense controversy regarding the spirometric definition to choose for the diagnosis of COPD. It has been argued that the use of a set FEV1/FVC ratio could lead to overdiagnosis of COPD. An alternative approach consists in using the lower limit of normal (LLN). However, recent studies have indicated that this argument may not be exact. The COLD initiative,17 a national Canadian epidemiologic study, compared the exactness of the GOLD stage II criterion with that of the LLN. The results demonstrate that the GOLD stage II+ criterion was, in fact, stricter than the LLN criterion (P<.001). In another study,18 when the symptoms of the different groups defined with these 2 criteria were compared, there were no differences for the distance walked in 6min, frequency of bronchitis symptoms, St. George's Respiratory Questionnaire score, MRC scale score or SF-36 (Short-Form Health Survey) score. The LLN and the set ratio give similar results when differentiating the respiratory symptoms of a high-risk population. These results endorse the continued use of GOLD stage II+ for detecting the chronic limitation of airflow that is clinically important in the management of COPD.
ConclusionsOur data shows a significant inverse correlation between the prevalence/severity of COPD and altitude. Altitude could induce a greater growth of the airways compared with lung size, resulting in an increase of the FEV1/FVC ratio. This could be an adaptation mechanism as a response to the chronic hypoxia.
Please cite this article as: Laniado-Laborin R, et al. Gran altitud y prevalencia de la enfermedad pulmonar obstructiva crónica: ¿ relación casual o causal? Arch Bronconeumol. 2012;48:156–60.