The non-adherence to tuberculosis treatment is associated with increased infection, antibiotic resistance, increased costs and death. Our objective was to identify factors associated with lack of completion of conventional treatment for tuberculosis in Peru.
Patients and methodsAn unmatched case–control study in patients diagnosed with tuberculosis from 2004 to 2005 who completed treatment until September 2006. The cases were defined as patients who discontinued treatment for ≥30 consecutive days, while the controls were defined as those who completed treatment without interruption. The factors were identified by logistic regression, calculating odds ratios (OR) and 95% confidence intervals (CI).
ResultsWe studied 265 cases and 605 controls. The non-adherence to treatment in our study was associated with the male sex (OR=1.62; CI: 1.07–2.44), having felt discomfort during treatment (OR=1.76; CI: 1.19–2.62), a prior history of non-compliance (OR=7.95; CI: 4.76–13.27) and illegal drug use (OR=3.74; CI: 1.25–11.14). Also, if we consider the interaction of previous non-adherence history and poverty, the risk of non-completion increases (OR=11.24; CI: 4–31.62). Conversely, having been properly informed about the disease (OR=0.25; CI: 0.07–0.94) and being able to access health-care services within office hours (8am–8pm) (OR=0.52; CI: 0.31–0.87) were associated with better adherence.
ConclusionsThe non-compliance with anti-tuberculosis treatment was associated with non-modifiable factors (male sex, previous non-compliance) and with others whose control would improve compliance (malaise during treatment, illegal drug use and poverty). Likewise, providing access to the health-care system and improving the information given about tuberculosis should be the priorities.
El abandono del tratamiento antituberculoso se asocia a mayor contagio, resistencia antibiótica, aumento de costes y muerte. Nuestro objetivo fue identificar factores asociados al abandono del tratamiento antituberculoso convencional en Perú.
Pacientes y métodosEstudio de casos y controles no pareado en pacientes diagnosticados de tuberculosis durante 2004–2005 y que finalizaron tratamiento hasta septiembre de 2006. Se definieron como casos los pacientes que abandonaron el tratamiento por ≥30 días consecutivos, y como controles los que completaron el tratamiento sin interrupción. Los factores se identificaron mediante regresión logística, calculándose las odds ratios (OR) y los intervalos de confianza al 95% (IC).
ResultadosSe estudiaron 265 casos y 605 controles. El abandono del tratamiento en nuestro estudio se asoció al sexo masculino (OR=1,62; IC: 1,07–2,44), al hecho de sentir malestar durante el tratamiento (OR=1,76; IC: 1,19–2,62), al antecedente de abandono previo (OR=7,95; IC: 4,76–13,27) y al consumo de drogas recreativas (OR=3,74; IC: 1,25–11,14). Así mismo, si tenemos en cuenta la interacción antecedente de abandono previo y pobreza, el riesgo de abandono aumenta (OR=11,24; IC: 4–31,62). Por el contrario, recibir buena información sobre la enfermedad (OR=0,25; IC: 0,07–0,94) y poder acceder al sistema sanitario en los horarios ofertados (08.00–20.00h) (OR=0,52; IC: 0,31–0,87) se asociaron a un mejor cumplimiento.
ConclusionesEl abandono del tratamiento antituberculoso se asoció a factores no modificables (sexo masculino, abandono previo) y a otros cuyo control mejoraría el cumplimiento (malestar durante el tratamiento, consumo de drogas recreativas y pobreza). Así mismo, es prioritario facilitar el acceso al sistema sanitario y mejorar la información recibida sobre tuberculosis.
Tuberculosis (TB) is still a public health problem the world over, with a great part of its morbidity and mortality concentrated in developing countries.1 Since 1999, Peru is among the 23 countries with the greatest TB load, according to the WHO classification. In 2002, Vietnam and Peru were removed from this list because, according to the reports of these countries, they were able to meet the objectives of the millennium for the detection and treatment of cases: 70% of cases detected and 85% of cases cured.1,2 However, despite these achievements, Peru still maintains the highest rate of incidence of TB in Latin America together with Bolivia and Ecuador.1 Likewise, it is the country with the greatest number of multidrug-resistant TB (MDR-TB) cases and extremely drug-resistant TB (XDR-TB) cases in the continent.1,3 One of the main causes of this problem has been the high rates of treatment non-compliance before the 1990s (50%). Moreover, even though the prevalence of non-compliance in the last five years has been less than 5%,4 this average is not representative of the high rates of several cities and provinces or departamentos.
Non-adherence to anti-tuberculosis treatment is defined as not coming to the clinic for treatment for more than thirty consecutive days.4 It is an important barrier for controlling TB because it is related with treatment failure, the development of drug resistances, dissemination of the infection and increased treatment costs.5 Among the possible reasons for non-compliance are: the prolonged duration of the treatment (6–8 months), the high number of pills (minimum of 11), adverse reactions to anti-tuberculosis medicine and lack of information about the disease and its treatment.
The identification of factors that influence the probability of discontinuing the treatment is the first step in designing interventions that improve treatment adherence and the control of the disease. Therefore, the objective of this study was to identify the risk factors associated with non-compliance of anti-tuberculosis treatment in the four Peruvian provinces with the highest incidence.
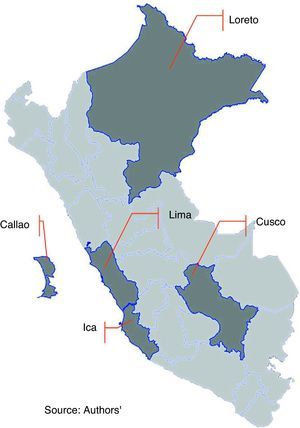
Patients and MethodsWe carried out a study of unmatched cases and controls (1:2). The study sample was randomly selected from among patients who initiated treatment in 2004–2005 and who completed treatment up until September 2006 in four Peruvian provinces (Loreto, Cusco, Ica and Lima (Callao)). Together, these provinces accumulated 80% of the total number of patients who had abandoned treatment. In order to select the provinces, the Pareto method was used because, due to logistical and economic difficulties, all the provinces of the country could not be covered (Table 1 and Fig. 1). The data collection was done from January 2007 to January 2008 (basically due to the difficult geographic accessibility in the provinces).
Distribution of the Cases and Control Subjects by Departamentos.
| Province | Patients Admitted to ESNPyCTBC, 2003 | Patients did not Comply With ESNPyCTBC, 2003 | Non-compliance Rate, 2003 | Percentage of the Sample Assigned to 2004 | Cases Needed for the Study, per Departamento, 2004 | Controls Needed for the Study, per Departamento, 2004 |
| Lima | 4018 | 256 | 5.6 | 75.29 | 200 | 444 |
| Callao | 534 | 29 | 4.1 | 8.53 | 23 | 50 |
| Loreto | 451 | 20 | 3.8 | 5.88 | 16 | 35 |
| Ica | 287 | 20 | 5.6 | 5.88 | 16 | 35 |
| Cusco | 282 | 15 | 4.6 | 4.41 | 12 | 26 |
| Total | 5572 | 340 | 5.3 | 100.00 | 265 | 590 |
The sample size was calculated based on the number of patients treated the previous year.
The sample size was determined based on a pilot study that had evaluated different variables, among these being previously discontinued treatments. This variable was what allowed us to obtain a larger sample size. The prevalence in this pilot study for the controls was 0.02 (patients who did not abandon) and when we considered a power of 80%, an odds ratio of 3.14 and a 95% confidence interval, we obtained a sample size of 265 cases and 530 controls.
The participants were patients treated with Directly Observed Treatment (DOT) with treatment schemes I and II (I: indicated for never-treated patients; and II: indicated for relapses and those who had previously discontinued treatment, then returned). Scheme I included: Isoniazid (H), Rifampicin (R), Pyrazinamide (Z) and Ethambutol (E). The duration was 6 months, until 82 doses were completed, divided into two stages: Phase 1: 50 doses (daily from Monday to Saturday with HRZE); Phase 2: 32 doses (2 times a week, with RH). Scheme II included: Rifampicin (R), Isoniazid (H), Pyrazinamide (Z), Ethambutol (E) and Streptomycin (S). The duration was 8 months (approximately 32 weeks), until 125 doses were completed, divided into two stages: Phase 1: 75 doses (2 months, daily, from Monday to Saturday with RHZES, followed by one month daily from Monday to Saturday with RHZE); Phase 2: 40 doses (intermittent, 2 times per week, with RHE). We excluded unconfirmed transfer patients because their actual condition was unknown (potential non-compliers or possible controls) and those patients with irregular treatment.
We defined cases (non-compliers) as those patients who stopped taking the treatment for a period of 30 consecutive days and controls as those patients who completed the treatment satisfactorily and were discharged from the National Health-Care Strategy for the Prevention and Control of Tuberculosis (in Spanish, ESNPyCTBC) as cured.
The cases were selected randomly, without any substitutions, and there were no patient deaths among the selected cases. The controls were selected from the same health-care center where the cases had been identified, using the patient registry of the ESNPyCTBC, obtaining data about the initial patient condition, clinical evolution, punctuality when taking treatment and Adverse Drug Reactions (ADR). Prior to the enrollment of the patients, informed consent was given by all the participants. Later, they answered a field survey that was designed according to the Lalonde Laframboise model2,4 that classifies risk factors into 4 groups: health-care service factors, human biology factors, lifestyle factors and environmental factors (including physical, social and psychological setting). The survey was applied at the participants’ homes and/or at the health-care centers, and the majority of the questions were closed. The interviewers were physicians and nurses who worked at the health-care establishments and had been trained.
Poverty was divided into three categories: extremely poor, poor and non-poor (according to the Peruvian National Institute for Statistics – INEI).6 For the evaluation of any possible alcoholism, the CAGE questionnaire proposed by the WHO was used, which classifies alcohol use into: no alcohol consumption, low risk for alcoholism (social drinker) and high risk of alcoholism (prejudicial consumption), the said test was modified in order to be used in retrospect. In order to evaluate the satisfaction of the subjects with the information received, we used the ISQ-1 test,7,8 which classifies this perception as either excellent, good, acceptable, unsatisfied and very unsatisfied. Last of all, to measure family support, the Olson and Wilson family satisfaction scale was used to classify the levels of satisfaction as high, average or low.9
For the statistical analysis, the data collected were subjected to a quality control, followed by a bivariate analysis comparing the distribution of variables between cases and controls. The resulting significant variables were input in a multivariate logistic regression analysis. The analyses were done with the SPSS 16.0 software package.
This study was completed and financed by the Epidemiology Agency of the Peruvian Health Ministry and was approved by the Ethics Committee of the Hospital Dos de Mayo in Lima.
ResultsWe analyzed 870 patients, 265 of which were cases and 605 controls. Out of the total number of patients, 60% were men, the predominant age group was between 21 and 30 (40%), 50.9% were single and 61% had completed secondary school.
As for their poverty level, 55% were not considered poor, 27% poor and 17% extremely poor. 70% of the patients were recruited from the outpatient consultations, and the remainder was identified by means of an active search (identification of patients with respiratory symptoms in the community). 15.2% had a previous history of non-compliance (35.8% [95] of the cases and 6.8% [41] of the controls) and 57.7% felt discomfort during the treatment (66.9% of cases and 54.2% of the controls). Likewise, 24.9% consumed alcohol, 4.3% addictive drugs (marihuana, cocaine, crack) and 3.6% recreational drugs (terokal, ecstasy).
At the bivariate level, we observed that the factors associated with risk of discontinuing treatment were: being male, feeling malaise during treatment, expressing some sort of fear about the treatment and not having a good family environment, considering the quantity of medication excessive, having a bad relationship with health-care workers, doubting the capability of the health-care personnel, presenting a history of previous non-compliance, not being satisfied with the information received, as well the consumption of alcohol, recreational drugs and addictive drugs.
The protection factors that lowered non-adherence were: higher education, having a spouse/partner, trusting the treatment, having an adequate family relationship, not considering the quantity of medication excessive, having a good relationship with the health-care personnel, having received a home visit after three days of absence and considering the information received between good and excellent (Table 2).
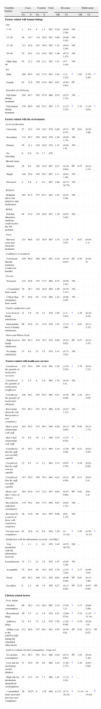
Factors Associated With Non-compliance of Anti-tuberculosis Treatment in Peru.
| Variables Studied | Cases | Controls | Total | Bivariate | Multivariate | ||||||
| No. | % | No. | % | OR | CI | OR | CI | ||||
| Factors related with human biology | |||||||||||
| Age | |||||||||||
| 7–14 | 1 | 0.4 | 8 | 1.3 | 855 | 0.28 | (0.04–2.29) | NS | … | ||
| 15–20 | 38 | 14.7 | 119 | 20.0 | 855 | 0.69 | (0.46–1.03) | NS | … | ||
| 21–30 | 113 | 43.6 | 231 | 38.8 | 855 | 1.22 | (0.91–1.64) | NS | … | ||
| 30–40 | 52 | 20.1 | 112 | 18.8 | 855 | 1.09 | (0.75–1.57) | NS | … | ||
| Older than 40 | 55 | 21.2 | 126 | 21.1 | 855 | 1.01 | (0.7–1.44) | NS | … | ||
| Sex | |||||||||||
| Male | 180 | 68.4 | 342 | 57.0 | 863 | 1.64 | (1.2–2.22) | a | 1.62 | (1.07–2.44) | a |
| Female | 83 | 31.6 | 258 | 43.0 | 863 | 0.61 | (0.45–0.83) | PF | … | ||
| Sensation of well-being | |||||||||||
| Felt better during treatment | 249 | 94.7 | 585 | 97.0 | 866 | 0.55 | (0.27–1.12) | NS | … | ||
| Felt malaise during treatment | 176 | 66.9 | 326 | 54.2 | 865 | 1.71 | (1.27–2.32) | a | 1.76 | (1.19–2.62) | a |
| Factors related with the environment | |||||||||||
| Level of education | |||||||||||
| University | 27 | 10.2 | 116 | 19.2 | 870 | 0.48 | (0.31–0.75) | PF | 0.61 | (0.36–1.06) | |
| Secondary | 174 | 65.7 | 362 | 59.8 | 870 | 1.28 | (0.95–1.73) | NS | … | ||
| Primary | 56 | 21.1 | 102 | 16.9 | 870 | 1.32 | (0.92–1.9) | NS | … | ||
| No schooling | 0 | 0.0 | 10 | 1.7 | 870 | ||||||
| Marital status | |||||||||||
| Married | 26 | 9.8 | 102 | 16.9 | 867 | 0.53 | (0.34–0.84) | PF | 0.75 | (0.42–1.31) | |
| Single | 140 | 52.8 | 303 | 50.3 | 867 | 1.11 | (0.83–1.48) | NS | … | ||
| Divorced | 5 | 1.9 | 4 | 0.7 | 867 | 2.88 | (0.77–10.79) | NS | … | ||
| Religion | |||||||||||
| Religion allows the patient to take medication | 254 | 97.3 | 577 | 97.3 | 854 | 1.01 | (0.41–2.48) | NS | … | ||
| Beliefs | |||||||||||
| Felt that alternative medicine could resolve the TB problem | 84 | 32.4 | 170 | 28.6 | 853 | 1.20 | (0.87–1.64) | NS | … | ||
| Fears | |||||||||||
| Showed some fear about the treatment | 131 | 49.6 | 233 | 38.9 | 863 | 1.55 | (1.16–2.07) | a | 0.87 | (0.58–1.3) | |
| Confidence in treatment | |||||||||||
| Convinced that the medicine would cure him/her | 239 | 90.9 | 580 | 96.7 | 863 | 0.34 | (0.19–0.63) | PF | 0.76 | (0.29–2) | |
| Poverty | |||||||||||
| Non-poor | 134 | 50.6 | 347 | 57.5 | 868 | 0.75 | (0.56–1.01) | NS | … | ||
| 1 Unsatisfied basic needs | 76 | 28.7 | 162 | 26.9 | 868 | 1.09 | (0.79–1.51) | NS | … | ||
| 2 More than unsatisfied basic needs. | 55 | 20.8 | 94 | 15.6 | 868 | 1.42 | (0.98–2.05) | NS | … | ||
| Family satisfaction scale | |||||||||||
| Low level of family satisfaction | 21 | 7.9 | 19 | 3.1 | 870 | 2.65 | (1.4–5.03) | a | 1.29 | (0.38–4.32) | |
| Intermediate level of family satisfaction | 66 | 24.9 | 91 | 15.0 | 870 | 1.87 | (1.31–2.68) | a | 0.85 | (0.31–2.32) | |
| Olson and Wilson Scale | |||||||||||
| High level of family satisfaction | 165 | 62.3 | 474 | 78.3 | 870 | 0.46 | (0.33–0.62) | PF | 0.57 | (0.22–1.47) | |
| No family satisfaction | 13 | 4.9 | 21 | 3.5 | 870 | 1.43 | (0.71–2.91) | NS | … | ||
| Factors related with health-care services | |||||||||||
| Considered the quantity of medication excessive | 132 | 50.4 | 208 | 34.6 | 864 | 1.92 | (1.43–2.58) | a | 1.76 | (0.43–7.21) | |
| Considered the quantity of medications insufficient | 4 | 1.5 | 6 | 1.0 | 864 | 1.54 | (0.43–5.5) | NS | … | ||
| Considered the quantity of medication adequate | 126 | 48.1 | 387 | 64.3 | 864 | 0.51 | (0.38–0.69) | PF | 1.24 | (0.3–5.05) | |
| Knowledge about the risk that produces non-compliance | 233 | 88.3 | 551 | 91.5 | 866 | 0.70 | (0.43–1.12) | NS | … | ||
| Had a good relationship with staff | 242 | 94.2 | 573 | 98.3 | 840 | 0.28 | (0.12–0.64) | PF | 0.59 | (0.21–1.71) | |
| Had a bad relationship with staff | 15 | 5.8 | 10 | 1.7 | 840 | 3.55 | (1.57–8.02) | a | … | ||
| Considered that the staff was not fully capable | 97 | 36.7 | 128 | 21.3 | 864 | 2.14 | (1.56–2.94) | PF | 0.21 | (0.01–3.83) | |
| Considered that the staff was not capable | 12 | 4.5 | 13 | 2.2 | 864 | 2.15 | (0.97–4.78) | a | 0.39 | (0.02–8.82) | |
| Considered that the staff was fully capable | 153 | 58.0 | 458 | 76.3 | 864 | 0.43 | (0.31–0.58) | PF | 0.13 | (0.01–2.4) | |
| Home visit after 3 days of absence | 165 | 63.0 | 417 | 72.5 | 837 | 0.64 | (0.47–0.88) | PF | 0.91 | (0.6–1.4) | |
| Recruited by outpatient consultation | 179 | 70.5 | 441 | 73.3 | 856 | 0.87 | (0.63–1.21) | NS | … | ||
| Recruited by a search of those with respiratory symptoms | 38 | 15.0 | 99 | 16.4 | 855 | 0.90 | (0.6–1.35) | NS | |||
| Previous non-compliance | 95 | 35.8 | 41 | 6.9 | 856 | 7.50 | (5–11.24) | a | 7.95 | (4.76–13.27) | a |
| Satisfaction with the information received – test ISQ-1 | |||||||||||
| Very unsatisfied with the information received | 3 | 1.1 | 2 | 0.3 | 870 | 3.45 | (0.57–20.78) | NS | … | ||
| Unsatisfactory | 15 | 5.7 | 21 | 3.5 | 870 | 1.67 | (0.85–3.29) | NS | … | ||
| Acceptable | 78 | 29.4 | 98 | 16.2 | 870 | 2.16 | (1.53–3.04) | a | 1.17 | (0.46–3.01) | |
| Good | 163 | 61.5 | 436 | 72.1 | 870 | 0.62 | (0.46–0.84) | PF | 0.81 | (0.33–1.98) | |
| Excellent | 6 | 2.3 | 48 | 7.9 | 870 | 0.27 | (0.11–0.64) | PF | 0.25 | (0.07–0.94) | PF |
| Lifestyle-related factors | |||||||||||
| Toxic habits | |||||||||||
| Alcohol consumption | 96 | 36.2 | 121 | 20.2 | 865 | 2.25 | (1.63–3.1) | a | 1.17 | (0.66–2.06) | |
| Recreational drugs | 20 | 7.5 | 11 | 1.8 | 870 | 4.41 | (2.08–9.34) | a | 3.74 | (1.25–11.14) | a |
| Addictive drugs | 22 | 8.3 | 15 | 2.5 | 870 | 3.56 | (1.82–6.98) | a | 0.70 | (0.26–1.9) | |
| Ability to go to the ESNPyCTBC during the scheduled office hours | 212 | 80.0 | 527 | 88.1 | 863 | 0.54 | (0.36–0.8) | PF | 0.52 | (0.31–0.87) | PF |
| Scale to evaluate alcohol consumption – Cage test | |||||||||||
| No alcohol consumption | 181 | 68.3 | 501 | 83.1 | 868 | 0.44 | (0.31–0.61) | PF | 1.02 | (0.48–2.16) | |
| Low risk for alcoholism (social drinker) | 51 | 19.2 | 58 | 9.6 | 868 | 2.24 | (1.49–3.37) | a | 1.28 | (0.61–2.68) | |
| High risk for alcoholism (prejudicial consumption) | 33 | 12.5 | 44 | 7.3 | 868 | 1.81 | (1.12–2.91) | a | … | ||
| 1 unsatisfied basic need and previous non-compliance | 28 | 10.57 | 6 | 1.02 | 856 | 11.52 | (4.71–28.18) | a | 11.24 | (4–31.62) | b |
OR, odds ratio; CI, confidence interval.
The multivariate analysis confirmed the influence of the variables of being male, presenting some type of malaise during treatment, having a history of previously discontinuing treatment and use of recreational drugs. The protective factors were: presenting an excellent level of satisfaction with the information received and considering the patient care hours at the health-care centers adequate.
On the other hand, it has been observed that the risk for non-compliance among patients with a history of previous treatment discontinuation is 7.95 (4.76–13.27). This risk increases to 11.24 (4–31.62) if, in addition to presenting a history of previous non-adherence, the patient is also poor.
DiscussionThe control of TB largely depends on its being treated successfully. In this study of four Peruvian provinces, we have identified that non-compliance with anti-tuberculosis treatment is still relatively frequent and associated with non-modifiable factors (such as masculine sex, from a biological standpoint, and a history of previous non-compliance) and other factors whose control would improve adherence (malaise during treatment, consumption of recreational drugs, poverty, lack of satisfaction with the information received and the patient-care schedule). We should mention that sex could also be considered a modifiable factor as it may be influenced by either cultural or other factors.
For proper adherence to anti-tuberculosis treatment, it is important for several factors to interact.10 In this study, the male sex has been identified as a risk factor for treatment discontinuation. This coincides with other studies mainly due to the fact that in countries like Peru men are more actively employed, although the precarious working conditions often entail: lack of formalized work, lack of unemployment benefits, contracts without vacation time and lack of subsidies for illness, all of which make adherence to treatment even more difficult.11–13 No association was identified between the age groups, although other studies mention that patients in extreme age groups (older than 54 and younger than 15) presented a greater tendency towards non-adherence; this was not observed in our study, possibly due to the homogeneity of the sample.14
Another risk factor for non-compliance was feeling malaise during the treatment; this aspect was assessed in another study that recognizes there being a greater percentage of patients with side effects among the non-complier patients.15 Previous lack of adherence was also identified as a risk factor (OR=7.9).16 Likewise, it is known that people who have abandoned another treatment and those who have presented difficulties for caring for themselves are considered at high risk for discontinuing treatment.17 If the variable for previous non-compliance interacts with poverty, this risk increases to 11.24, which is a worrying fact because the large majority of patients in Peru are poor and many have a history of previous non-compliance.
In the drug use analysis, there was a demonstrated association between recreational drugs and risk of non-compliance. In this case it must be kept in mind that TB patients are a low-income population, and therefore the most widely accessible drug in the country is terokal (adhesive). In the literature, we have found no articles associating this type of drug with non-compliance; however, subjects addicted to other drugs in Nicaragua18 were identified as having a risk that was five times higher. This was also observed in cocaine addicts in New York,19 and in heroin addicts in Barcelona.20 Furthermore, alcohol consumption has also been related with risk of non-compliance,18 although this relationship was not confirmed in the multivariate analysis.
Among the protective factors that were identified, it was observed that the patients who presented an excellent level of satisfaction with the information received had less of a probability of discontinuing treatment, as observed in other studies.19,21 Another protective factor was considering the patient-care hours adequate, (in Peru the primary-care centers offer a minimum of 12h of patient care per day). Likewise, in another study it was mentioned that the flexibility of the timetable and the comfortable setting of the health-care center were related with better treatment adherence.22 Contrarily, risk for non-compliance is three times higher among those who find it difficult to go to the health-care centers.18
In the literature, we found associations between non-adherence and lower levels of education,18 lack of confidence in the treatment23,24 and absence of a stable family environment.14,15,24 Nevertheless, none of these variables related with the patient environment was confirmed in the multivariate analysis. In the same manner, the variables depending on the health-care services related with non-compliance, such as considering the number of medications to be excessive,25 having a negative opinion of the care provided,26 or a poor relationship with the health-care professionals27,28 did not present any association.
The results of this study should be interpreted while considering some limitations: retrospective data collection is a complex task affected by memory biases; the interviewers were conscious of the conditions of the cases and could have influenced the collection of the information; our study did not obtain samples from all the provinces of the country, although it did include four departamentos that represent 80% of cases with discontinued treatment, and in this manner our results could be generalized to the majority of the affected population in Peru. Last of all, despite the delay in data collection and the analysis of these results, the technical regulations for the administration of treatment have not undergone any important changes; therefore, the results are still current and valid.
In conclusion, this study identified that the profile of Peruvian patients who do not comply with anti-tuberculosis treatment are subjects who are usually male, report some type of malaise during treatment, have a history of previous non-compliance, use recreational drugs, do not demonstrate an excellent level of satisfaction with the information received and also feel that they do not have enough time to go to the ESNPyCTBC (National Health-care Strategy for the Prevention and Control of Tuberculosis). On the other hand, it has been observed that the risk for discontinuing treatment in patients with a previous history of non-adherence increases substantially with the presence of poverty. The contribution of our study should be of particular interest to health-care professionals working with TB patients in the ESNPyCTBC as it demonstrates that special care should be taken in patients who present some of the mentioned factors.
Source of FundingDirección General de Epidemiología, Peruvian Ministry of Health.
Conflict of InterestThe authors declare no conflicts of interest.
To Dr. Eduardo Gotuzzo Herencia for his contributions in the drafting and analysis of this document.
Please cite this article as: Culqui DR, et al. Factores asociados al abandono de tratamiento antituberculoso convencional en Perú. Arch Bronconeumol. 2012;48:150–5.