Between 15 and 27% of patients admitted to Spanish hospitals are smokers. Hospitalization is an ideal time for a smoker to decide to quit.
We performed a MEDLINE search of controlled, randomized or observational studies associated with helping hospitalized patients quit smoking, published between January 1, 2002 and September 30, 2015. On the basis of the results of those studies, we have issued some recommendations for the treatment of smoking in hospitalized patients. The recommendations were drawn up according to the GRADE system. Offering the smoker psychological counselling and prolonging follow-up for at least 4 weeks after discharge is the most effective recommendation for helping hospitalized patients to quit.
Entre el 15 y el 27% de los pacientes que ingresan en los hospitales españoles son consumidores de tabaco. La hospitalización es un momento idóneo para que el fumador se plantee el abandono del tabaco.
Se ha realizado una búsqueda bibliográfica en MEDLINE entre el 1 de enero de 2002 y el 30 de septiembre de 2015, de estudios, controlados y aleatorizados u observacionales, relacionados con la ayuda para dejar de fumar a pacientes ingresados en el hospital. Basándose en los resultados de dichos estudios se han emitido unas recomendaciones para el tratamiento del tabaquismo en pacientes hospitalizados. Las recomendaciones han sido formuladas de acuerdo con el sistema GRADE. Ofrecer al fumador asesoramiento psicológico más tratamiento farmacológico mientras está ingresado en el hospital y prolongar el seguimiento durante al menos 4 semanas después del alta es la recomendación más efectiva para ayudar a dejar de fumar a los pacientes ingresados.
In 2013, a total of 4,637,427 patients were admitted to Spanish hospitals. The main reasons for hospitalization were cardiovascular (13.3%), gastrointestinal (12.2%), and respiratory tract (10.9%) diseases.1 Between 15% and 27% of patients hospitalized in Spain are smokers.2,3
Smoking is one of the main factors that contribute to worsening of the disease causing hospital admission. The hospital is an ideal place for an individual to give up smoking.
These guidelines on the treatment of smoking in hospitalized patients will address 3 main aspects: hospitalization as an opportunity for smoking cessation; the effectiveness of healthcare interventions to help hospitalized patients stop smoking; and the proposed recommendations for the treatment of smoking in these patients. These recommendations will be based on strength of evidence, according to the GRADE system.4
MethodologyThis document has been drawn up using the following methodology.
- 1)
A MEDLINE search was performed for studied published between 1 January, 2002 and 30 September, 2015. Key words for the patient population were “hospital”, “hospitalization”, “inpatients” and “hospital care”. Key words for smoking cessation interventions were “smoking”, “smoking cessation”, “tobacco”, “tobacco use cessation”, “smoking cessation program” and “tobacco use cessation products”. Inclusion criteria were: (a) studies related to smoking cessation support offered to patients admitted to a hospital; (b) randomized, controlled trials or observational studies; (c) studies evaluating an intervention for smoking cessation; and (d) studies published in English or Spanish.
- 2)
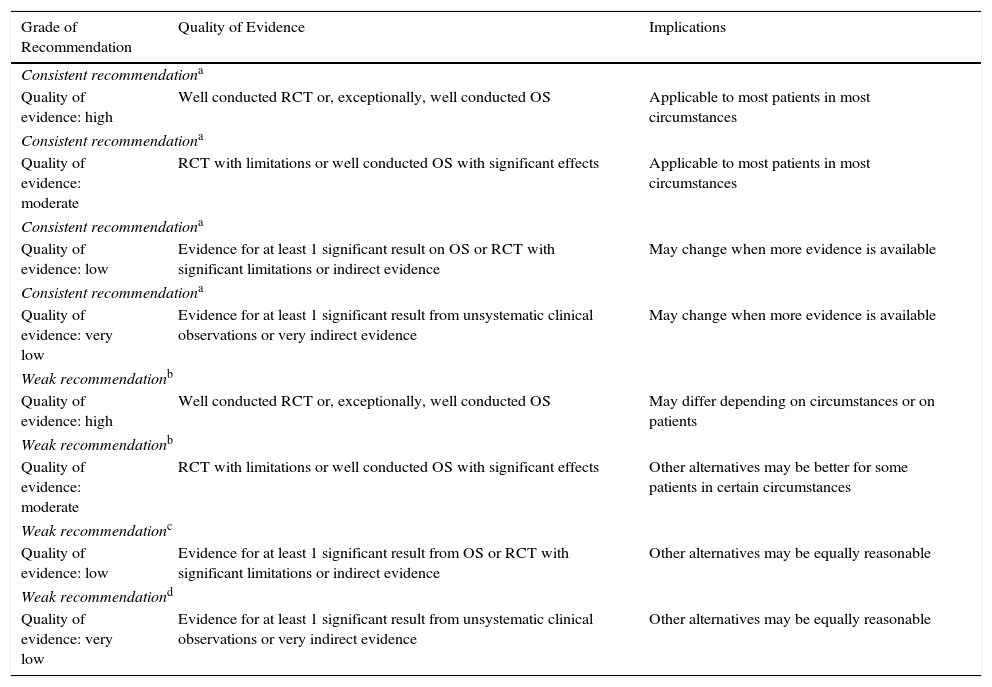
On the basis of the studies included, the first manuscript was drafted and the recommendations were formulated according to the GRADE system (Table 1).4 All members of the expert group reviewed the document, adding comments and suggestions, and the second version of the document was prepared.
Table 1.Classification of Recommendations and Quality of Evidence According to the GRADE System.
Grade of Recommendation Quality of Evidence Implications Consistent recommendationa Quality of evidence: high Well conducted RCT or, exceptionally, well conducted OS Applicable to most patients in most circumstances Consistent recommendationa Quality of evidence: moderate RCT with limitations or well conducted OS with significant effects Applicable to most patients in most circumstances Consistent recommendationa Quality of evidence: low Evidence for at least 1 significant result on OS or RCT with significant limitations or indirect evidence May change when more evidence is available Consistent recommendationa Quality of evidence: very low Evidence for at least 1 significant result from unsystematic clinical observations or very indirect evidence May change when more evidence is available Weak recommendationb Quality of evidence: high Well conducted RCT or, exceptionally, well conducted OS May differ depending on circumstances or on patients Weak recommendationb Quality of evidence: moderate RCT with limitations or well conducted OS with significant effects Other alternatives may be better for some patients in certain circumstances Weak recommendationc Quality of evidence: low Evidence for at least 1 significant result from OS or RCT with significant limitations or indirect evidence Other alternatives may be equally reasonable Weak recommendationd Quality of evidence: very low Evidence for at least 1 significant result from unsystematic clinical observations or very indirect evidence Other alternatives may be equally reasonable OS: observational studies; RCT: randomized, controlled trials.
- 3)
The second version of the manuscript was also reviewed by all the experts.
- 4)
The final document was approved by the entire group. This document was also approved by the Scientific and Research Committee of the Spanish Society of Pulmonology and Thoracic Surgery.
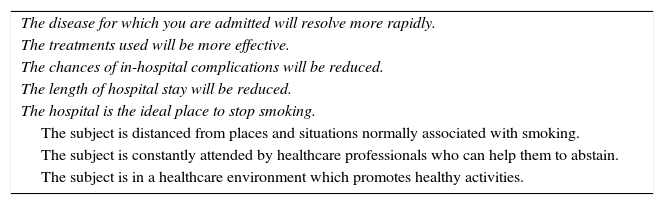
Smoking is one of the main causes of diseases that lead to hospitalization.1,5 Hospitalization is a good opportunity for a smoker to give up the habit. There are many reasons why this situation is ideal, the most important of which are listed in Table 2.1,6–9 The strongest of these reasons are the smoking ban in hospital facilities and the particular willingness of the patient to give up during hospitalization.
Reasons to Stop Smoking During Hospitalization.
| The disease for which you are admitted will resolve more rapidly. |
| The treatments used will be more effective. |
| The chances of in-hospital complications will be reduced. |
| The length of hospital stay will be reduced. |
| The hospital is the ideal place to stop smoking. |
| The subject is distanced from places and situations normally associated with smoking. |
| The subject is constantly attended by healthcare professionals who can help them to abstain. |
| The subject is in a healthcare environment which promotes healthy activities. |
It is important to understand that helping the hospitalized smoker to give up is the responsibility of all hospital personnel, including healthcare and non-healthcare staff, so it is important that all receive the appropriate training.
Analysis Of Interventions For Smoking Cessation In Hospitalized PatientsThe different studies that have evaluated the effectiveness of different interventions to help hospitalized patients stop smoking are described below. These include health counselling on smoking cessation, pharmacological treatment, or a combination of both. The recommendations of these guidelines are based on the outcomes and conclusions of these studies.
Health Counselling On Smoking CessationHealth counselling has been shown to be effective for helping hospitalized smokers to quit. Counselling, which may vary in intensity and duration, should clearly explain the benefits associated with giving up smoking and discuss the risks. In general, the greater the intensity, duration and frequency of counselling, the more effective the intervention.
It also seems that counselling provided in the hospital by different healthcare professionals, along with self-help materials, is more effective than standard treatment, particularly when it continues for at least 1 month after hospital discharge (relative risk [RR] 1.7, 95% CI 1.27–1.48).10,11 A metaanalysis found that when the intervention was conducted by 2 types of healthcare professionals, rates of abstinence increased compared to when it was conducted by only 1 (RR 2.5; 95% CI 1.9–3.4). Efficacy increased even further when the intervention was conducted by 3 healthcare professionals (RR 2.4; 95% CI 2.1–2.9).12
Different activities that prolong the healthcare intervention beyond the period of hospitalization have been proposed, the most important being personal contact between the healthcare professional and the patient, sending letters, SMS, emails, proactive telephone contact, etc., all of which help increase the efficacy of the interventions offered during the hospital stay.11–13
Pharmacological TreatmentOther studies have analyzed the efficacy of combining pharmacological treatment with health counselling in hospitalized smokers. The results of a metaanalysis of 6 studies indicate that the efficacy of intensive health counselling (counselling during the hospital stay that continues for at least 1 month after discharge) increases significantly with the addition of nicotine replacement therapy (NRT) (RR 1.54; 95% CI 1.34–1.79).10 One of the advantages of NRT in hospitalized smokers is its rapid onset of action.
Three studies compared the efficacy of varenicline and health counselling compared to counselling alone.13–15 One of these reported greater efficacy in the group that received varenicline compared to the control group (31.1 vs 21.4%; RR 1.45; 95% CI 1.03–2.03; P=.03).13 Another found no significant differences,14 while the third, which analyzed a group of 302 patients admitted for acute coronary syndrome, found greater efficacy in the group that received varenicline compared to the control group (47.3 vs 32.5%, P=.012).15
It is also important to point out that the use of varenicline in hospitalized patients, some of whom have chronic diseases, is as safe as placebo, and nausea was the only event that appeared more frequently in the active treatment group (16.3 vs 1.5%).14,16 Even in the group of subjects admitted for acute coronary syndrome, varenicline was shown to be as safe as placebo. The rate of severe cardiovascular adverse effects 30 days after completing the treatment period was similar in both groups: 4% for varenicline and 4.6% for placebo.15
Three studies have compared the efficacy of the combination of bupropion and intensive health counselling in hospitalized patients, compared to the usual interventions for helping individuals to stop smoking. None of these studies found that this medication was useful for helping patients to quit.17–19 A metaanalysis of these 3 studies was also performed, which also failed to demonstrate efficacy (RR 1.04; 95% CI 0.75–1.45). Interestingly, 2 of these studies were performed in patients who had been admitted for acute cardiovascular disease (myocardial ischaemia), and no short or long-term adverse cardiovascular effects appeared in the group of subjects that used bupropion, compared to the group that received standard care.18,19 These data were confirmed in a recent metaanalysis and in a new randomized, controlled clinical trial.20,21
A recent randomized, double-blind, controlled clinical trial examined the efficacy of a smoking treatment programme in a group of smokers who received intensive counselling for smoking cessation during admission, followed by continued counselling with automated interactive voice response telephone calls after discharge, as well as the treatment of their choice for a period of 3 months (NRT, bupropion or varenicline). The results showed that this programme after 6 months of follow-up was significantly more effective than standard care (27 vs 16%, RR 1.70; 95% CI 1.15–2.51; P=.007).22
Of note is a Spanish study which included a total of 2560 hospitalized smokers. The authors reported that intensive psychological counselling was more effective than minimal counselling, and that its efficacy increased even further when combined with NRT.23
Safety and Efficacy of Interventions for Smoking Cessation in Hospitalized Patients With ComorbiditiesIn their meta-analysis, Rigotti et al. included a total of 14 clinical trials conducted in patients admitted for acute cardiovascular problems in which the efficacy of an intensive intervention to quit smoking in the hospital was compared with standard care.10 The results showed that the intensive intervention was more effective than standard care (RR 1.42; 95% CI 1.29–1.56).10 Moreover, one of the studies also analyzed all-cause mortality and readmission rates over a 2-year period. The results showed that the intervention in patients with cardiovascular disease led to a reduction in the RR of all-cause mortality (RR 0.77; 95% CI 0.27–0.93; P=.014) and readmission (RR 0.44; 95% CI 0.16–0.63; P=.007).24
Five studies have analyzed the efficacy of the interventions for smoking cessation in patients admitted with respiratory diseases.25–29 In 2 of these, NRT (chewing gum in 1, patches in the other) was offered in addition to smoking cessation counselling.25,26 The study that offered patches found that in the active group, rates of continuous abstinence between months 3 and 12 were higher than in the placebo group (21% vs 14%, respectively), although the difference was not significant.25 The other 3 studies compared the efficacy of intensive counselling interventions without the use of medication, compared to standard care in patients with chronic obstructive pulmonary disease.27–29 One of the studies found that, after 1 year of follow-up, patients who had received intensive interventions showed an almost 3-fold increase in abstinence compared to those who had received standard care (RR 2.83; 95% CI 1.40–5.74).29 No significant differences were found in the other 2.27,28 However, it must be taken into account that the intervention received by the active group was not very intensive.27,28
Cost-efficacy of Interventions for Smoking Cessation in Hospitalized PatientsA recent study reported that a hospital intervention consisting of cessation counselling during admission, pharmacological treatment, and follow-up after discharge had a cost per quality-adjusted life year of 1386 Canadian dollars, and that providing this type of treatment to 15,326 hospitalized smokers would lead to 4689 individuals giving up, which would help avoid 116 readmissions, 923 days of hospital stay, and 119 deaths.30
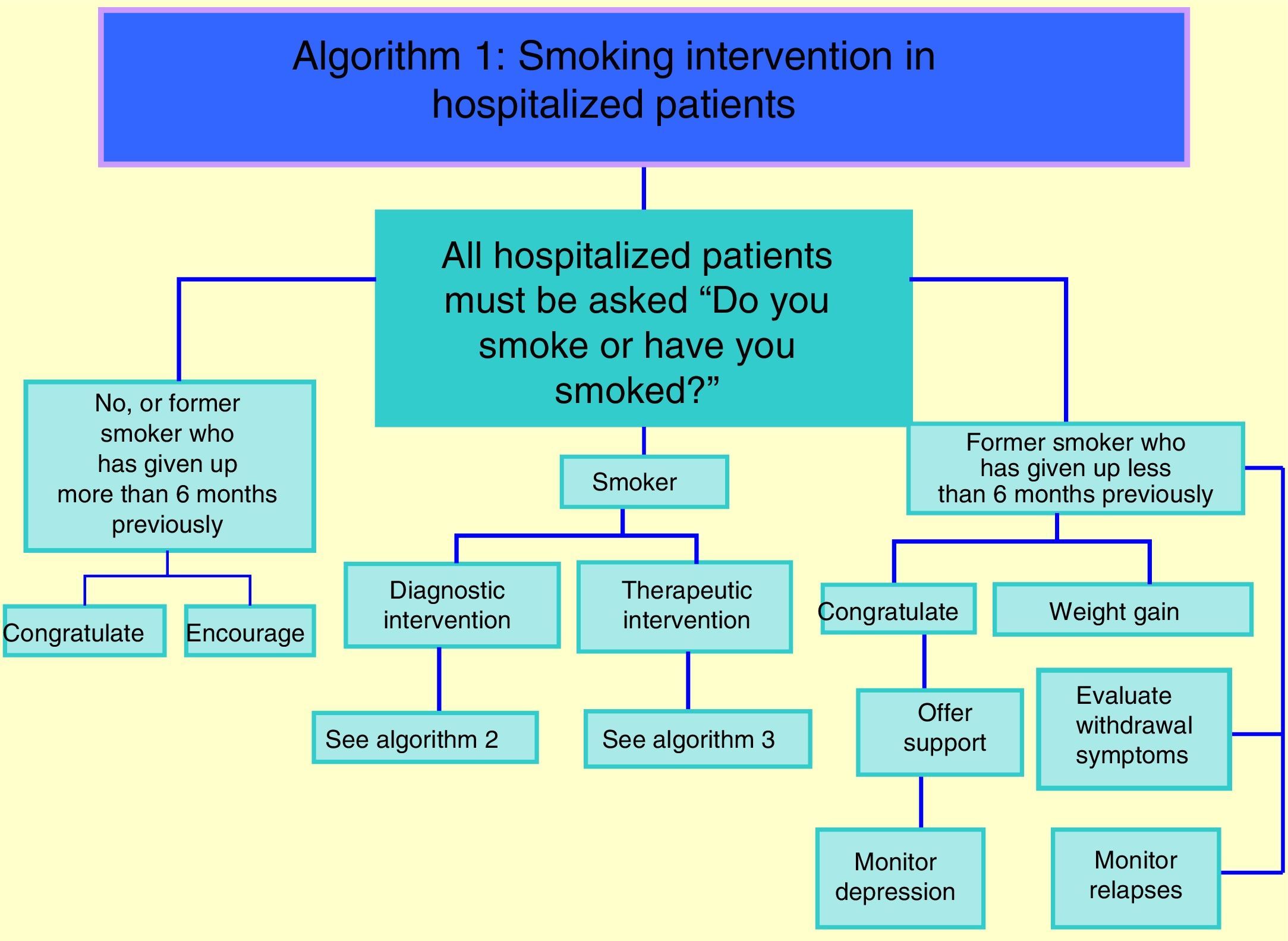
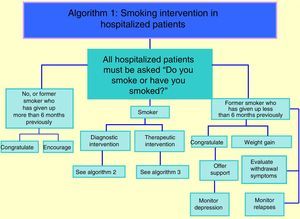
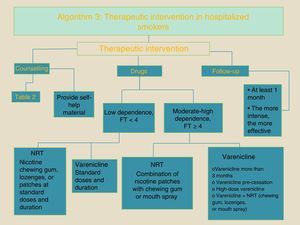
Recommendations for Smoking Interventions Among Hospitalized PatientsThese recommendations are aimed at patients admitted to hospital. Fig. 1 shows a protocol which should be followed in all hospitalized patients. The following is a discussion of the items in this protocol and the corresponding recommendations drawn up by our working group. These recommendations will be classified according to the GRADE system4 (Table 3).
Recommendations for Intervention in Smoking Among Hospitalized Patients.
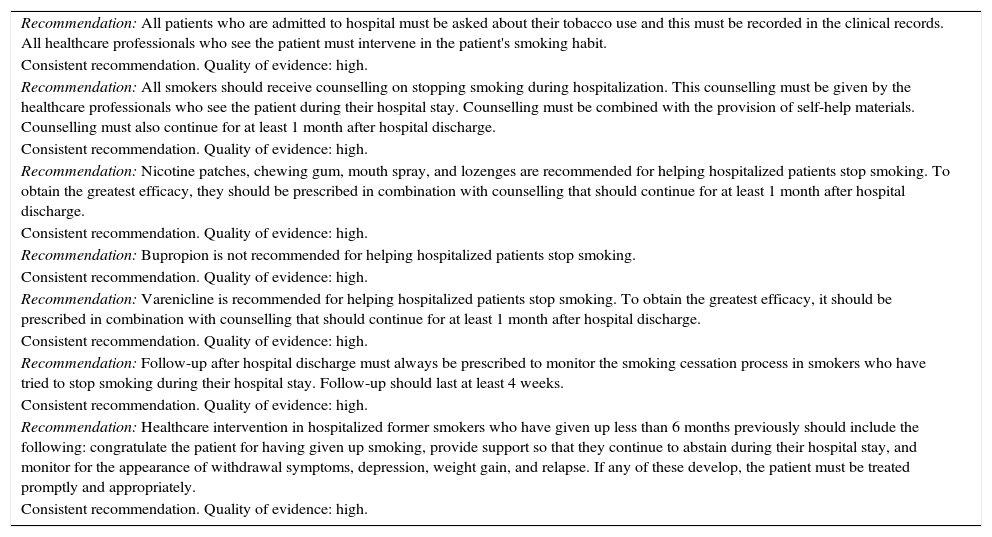
| Recommendation: All patients who are admitted to hospital must be asked about their tobacco use and this must be recorded in the clinical records. All healthcare professionals who see the patient must intervene in the patient's smoking habit. |
| Consistent recommendation. Quality of evidence: high. |
| Recommendation: All smokers should receive counselling on stopping smoking during hospitalization. This counselling must be given by the healthcare professionals who see the patient during their hospital stay. Counselling must be combined with the provision of self-help materials. Counselling must also continue for at least 1 month after hospital discharge. |
| Consistent recommendation. Quality of evidence: high. |
| Recommendation: Nicotine patches, chewing gum, mouth spray, and lozenges are recommended for helping hospitalized patients stop smoking. To obtain the greatest efficacy, they should be prescribed in combination with counselling that should continue for at least 1 month after hospital discharge. |
| Consistent recommendation. Quality of evidence: high. |
| Recommendation: Bupropion is not recommended for helping hospitalized patients stop smoking. |
| Consistent recommendation. Quality of evidence: high. |
| Recommendation: Varenicline is recommended for helping hospitalized patients stop smoking. To obtain the greatest efficacy, it should be prescribed in combination with counselling that should continue for at least 1 month after hospital discharge. |
| Consistent recommendation. Quality of evidence: high. |
| Recommendation: Follow-up after hospital discharge must always be prescribed to monitor the smoking cessation process in smokers who have tried to stop smoking during their hospital stay. Follow-up should last at least 4 weeks. |
| Consistent recommendation. Quality of evidence: high. |
| Recommendation: Healthcare intervention in hospitalized former smokers who have given up less than 6 months previously should include the following: congratulate the patient for having given up smoking, provide support so that they continue to abstain during their hospital stay, and monitor for the appearance of withdrawal symptoms, depression, weight gain, and relapse. If any of these develop, the patient must be treated promptly and appropriately. |
| Consistent recommendation. Quality of evidence: high. |
All patients admitted to hospital should be asked about their tobacco use. Responses to this question can be the following: (a) smoker; (b) former smoker who has given up less than 6 months previously, and (c) never smoker or former smoker who has given up more than 6 months previously. The response must be recorded in the patients’ clinical records.
All hospitals are recommended to use electronic alert systems to remind healthcare professionals to always record tobacco use in the clinical records of hospitalized patients. This strategy has been identified by the Clinical Practice Guideline of the US Department of Health and Human Services as effective in increasing the number of interventions by healthcare professionals on smoking in hospitalized patients.12 A meta-analysis of 9 studies found that when an alert system was used for recording patient smoking habits, the rates of smoking cessation intervention by healthcare professionals increased significantly (RR 3.1; 95% CI 2.2–4.2).12 It is also important that the smoking intervention in hospitalized patients is performed by all the healthcare professionals who see that patient during their admission, working as a group. In this respect, interventions by nursing professionals are very valuable and highly recommended.10–13
Recommendation: all patients who are admitted to hospital must be asked about their tobacco use and this must be recorded in the clinical records. All healthcare professionals who see the patient must intervene in the patient's smoking habit. This is a consistent recommendation. Quality of evidence: high.
Recommendations for Intervention in Hospitalized SmokersIntervention in hospitalized smokers consists of 2 parts: a diagnostic intervention and a therapeutic intervention.
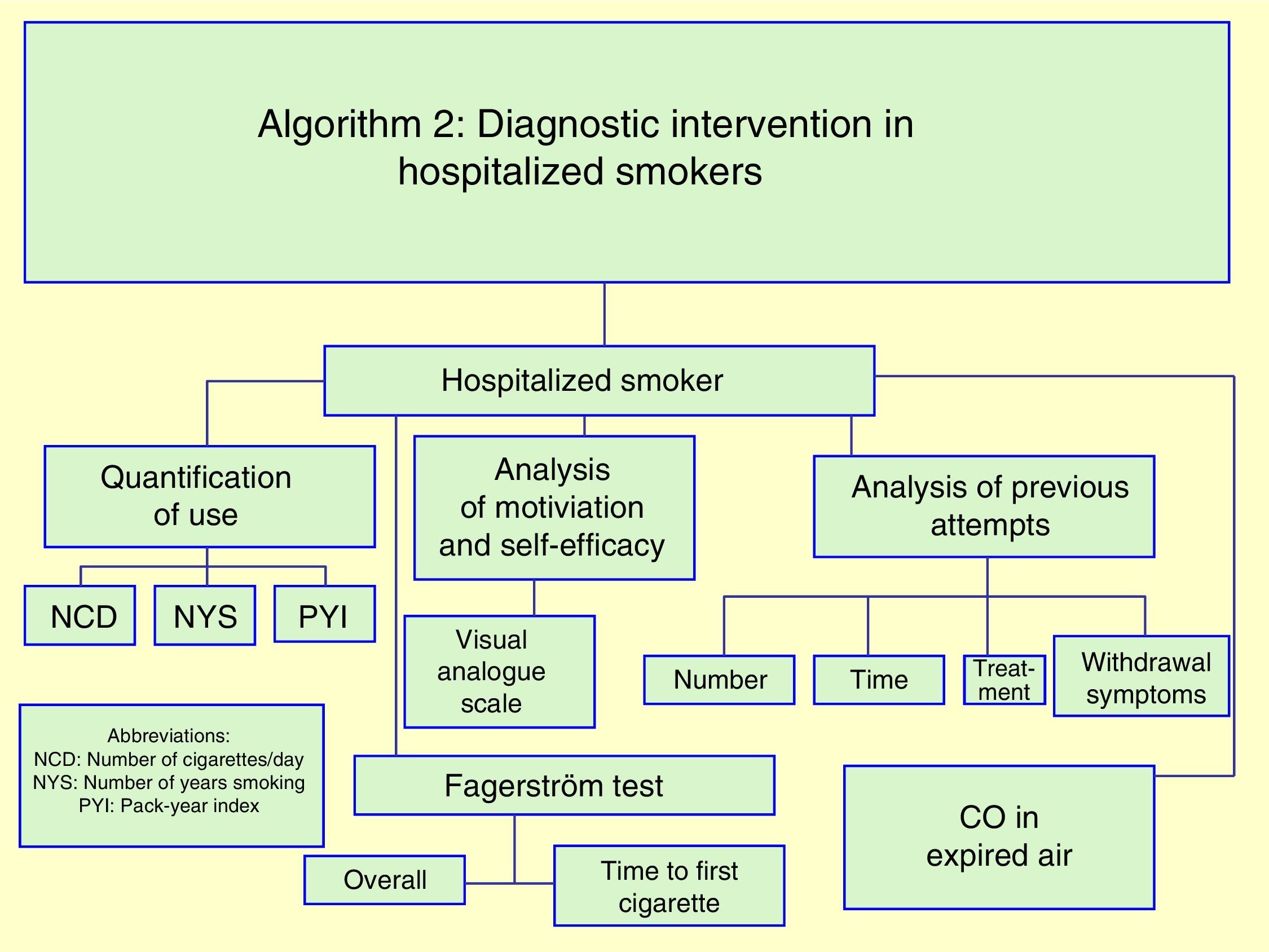
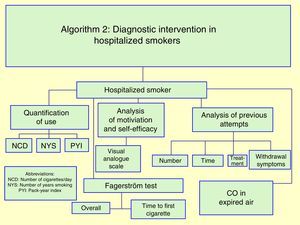
Diagnostic InterventionThe diagnostic intervention will investigate the following aspects10–12 (Fig. 2):
- A)
Quantification of accumulated tobacco use: the pack-year index will be calculated.
- B)
Analysis of motivation and self-efficacy for quitting smoking: the use of a visual analogue scale for measuring these variables is recommended.
- C)
Analysis of physical nicotine dependence: the Fagerström test is highly recommended for quantifying this variable. In cases in which it is assumed that the nature of the disease that brought the individual to hospital will prevent them from smoking a large number of cigarettes a day, it is of particular value to assess the response to the question “how soon after waking do you smoke your first cigarette of the day?”.
- D)
Previous attempts to quit during which the subject went at least 24h without smoking will be investigated. This investigation will determine the number of previous attempts, the time that the patient went without smoking during those attempts, treatments used, and particularly, the withdrawal symptoms experienced during those attempts.
- E)
Determination of CO levels in expired air: this is a simple, non-invasive, inexpensive and highly useful test that should be obligatory in all smokers admitted to hospital.
However, it is important to note that evaluating these aspects should not be a pre-requisite for offering treatments for smoking, since the treatment of smoking is effective and should be administered even if specialized evaluations are unavailable or not performed.12
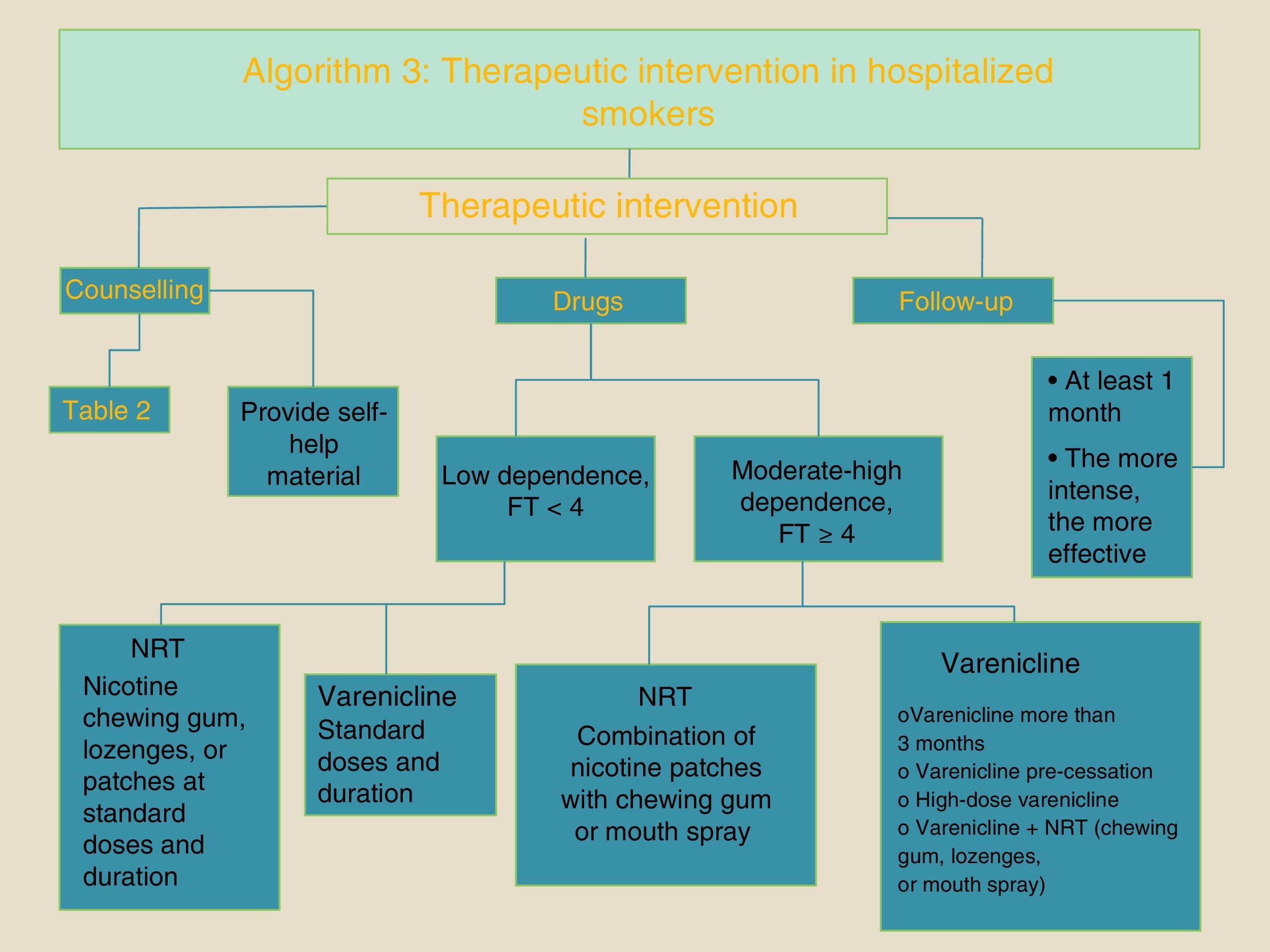
Therapeutic InterventionFig. 3 shows the healthcare intervention that should be given to a smoker who is admitted to hospital. This intervention consists of counselling on smoking cessation, the prescription of pharmacological treatment, and a follow-up regimen.
The healthcare professional should warn the patient that they will not be able to smoke during their hospital stay. The main reasons for not smoking will be explained. These reasons are listed in Table 2. All these warnings should be given with empathy, respect, and understanding.
Recommendation: all smokers must receive counselling on smoking cessation during hospitalization, given by all the healthcare professionals who see the patient during their hospital stay. Counselling must also be accompanied by the provision of self-help materials, and it must also continue for at least 1 month after hospital discharge. This is a consistent recommendation. Quality of evidence: high.
Pharmacological TreatmentHealth counselling for smoking cessation offered to hospitalized smokers must be combined with the use of medication.
Three types of drugs have been used: NRT, bupropion and varenicline. Recommendations on the use of each of these products are listed below. For more information, please see the complete version of these guidelines, available at www.separ.es.
Nicotine Replacement TherapyThe use of any type of NRT, particularly chewing gum, lozenges, mouth sprays or patches, is highly recommended for hospitalized smokers.10,22 Prescription of these medications will help control any withdrawal symptoms and help the patient abstain from smoking during their hospital stay.
In smokers with a low degree of physical dependence on nicotine (less than 4 points on the Fagerström test), the prescription of 2mg nicotine in chewing gum, or 1mg in lozenges, or 16- or 24-hour patches at doses of 15 or 21mg/day, respectively, is useful. In smokers with a moderate or high degree of physical dependence on nicotine (4 or more points on the Fagerström test), the use of nicotine patches in combination with nicotine chewing gum, lozenges or mouth spray is required.31
The use of NRT in hospitalized smokers has significant advantages, namely, its rapid onset of action − it is effective from the first administration − and its lack of adverse effects. There are very few contraindications to its use and very few interactions with other drugs that the hospitalized patient may be receiving.12
Although acute coronary syndrome has traditionally been cited as a contraindication for NRT, this is now very controversial. A recent study carried out in hospitalized smokers treated with NRT, some of whom had acute coronary syndrome, showed that this intervention in these patients was effective and safe.24 The American College of Cardiology/American Heart Association also recommends the use of NRT in this group of patients.32
Recommendation: nicotine patches, chewing gum, mouth spray, or lozenges are recommended to help hospitalized patients stop smoking. To obtain the greatest efficacy, they should be prescribed in combination with counselling that should continue for at least 1 month after hospital discharge. This is a consistent recommendation. Quality of evidence: high.
BupropionBupropion has not been shown to be effective for helping hospitalized smokers to quit smoking,10,17–19,22 although this medication has been shown to be safe in this patient group, even those with cardiovascular disease.18,19
The main disadvantages of this medication in hospitalized smokers are its 7–14 day response time. In addition, it is metabolized by the liver, via the enzymatic P450 complex, so may be associated with significant interactions with other medications.
Recommendation: bupropion is not recommended for helping hospitalized patients stop smoking. This is a consistent recommendation. Quality of evidence: high.
VareniclineThe efficacy and safety of varenicline in helping hospitalized patients stop smoking, even in those with acute coronary syndrome, has been clearly demonstrated in 3 out of 4 clinical trials.13–15,22
Varenicline should be used at the standard dose for a period of 12 weeks.12,33,34 In patients with a high degree of dependence or chronic respiratory diseases, it is highly advisable to use it at the dose and for the duration indicated by scientific societies such as the Spanish Society of Pulmonology and Thoracic Surgery and the European Respiratory Society.33,34
The major drawback for the use of varenicline in hospitalized patients is the need to administer it for 1 week before it becomes fully effective. Nevertheless, its metabolic profile − it is eliminated via the urine with no hepatic involvement – rules out potential drug interactions, and it can be easily used in many polymedicated hospitalized patients.12,33,34
Recommendation: varenicline is recommended for helping hospitalized patients stop smoking. To obtain the greatest efficacy, it should be prescribed in combination with counselling that should continue for at least 1 month after hospital discharge. This is a consistent recommendation. Quality of evidence: high.
Follow-upAn essential aspect of treatment of smoking in hospitalized smokers is the follow-up period. To obtain the greatest efficacy, follow-up should continue for at least 1 month after hospital discharge. The longer the follow-up, the greater the efficacy.
Recommendation: follow-up after hospital discharge must always be prescribed to monitor the progress of smokers who have tried to stop smoking during their hospital stay. Follow-up should last at least 4 weeks. This is a consistent recommendation. Quality of evidence: high.
Recommendations for Intervention in Hospitalized Former Smokers, Who Have Given Up Less Than 6 Months PreviouslyThe Clinical Practice Guideline of the US Department of Health and Human Services recommends that intervention in these patients include the following12 (Fig. 1):
- 1.
Congratulations: patients should be warmly congratulated on their decision to stop smoking by all attending healthcare professionals.12
- 2.
Offer of support: all healthcare professionals must offer support to the former smoker to help them remain abstinent during their hospital stay.12
- 3.
Evaluation of withdrawal symptoms: if the patient stopped smoking less than 3 months previously, they may still have withdrawal symptoms. In these cases, withdrawal symptoms should be carefully evaluated and medication should be prescribed, if necessary.12
- 4.
Depression or negative mood: these symptoms can appear in up to 25%–30% of former smokers who have given up less than 6 months previously. If they occur, they should be diagnosed and treated appropriately.12
- 5.
Weight gain: around 85% of smokers gain weight on quitting the habit. The amount gained is generally between 2 and 5kg in approximately 4–6 months.35
- 6.
Monitor relapses: most relapses among smokers who have quit occur during the first 6 months after giving up smoking. Hospitalized smokers who are in this situation must be monitored for the early detection of relapse.
Recommendation: healthcare intervention in hospitalized former smokers who have given up less than 6 months previously should include the following actions: congratulate the patient for having given up smoking, provide support so that they continue to abstain during their hospital stay, and monitor the appearance of withdrawal symptoms, depression, weight gain, and relapse. If any of these develop, the patient must be treated promptly and appropriately. This is a consistent recommendation. Quality of evidence: high.
Recommendations for Intervention in Patients Who Are Never Smokers or Who Have Stopped Smoking More Than 6 Months PreviouslyInterventions in individuals who state that they have never smoked or who stopped smoking more than 6 months previously are limited to congratulating the patient and encouraging them to continue (Fig. 1).
Conflict of InterestsDrs Carlos A. Jiménez Ruiz, Jose Ignacio de Granda Orive, Segismundo Solano Reina, Juan Antonio Riesco Miranda, Jose Francisco Pascual Lledó y Marcos Garcia Rueda have collaborated with GSK and Pfizer, pharmaceutical companies with interests in the field of treating smoking.
The other authors state that they have no conflict of interests.
We thank Dr. Angela Ramos Pinedo (Hospital Fundación Alcorcón, Madrid, Spain) and Dr. Daniel Buljubasich (Hospital Español, Rosario, Argentina, and Director of the Smoking Area of the Latin American Thoracic Association), who acted as external reviewers of this document.
Please cite this article as: Jiménez Ruiz CA, de Granda Orive JI, Solano Reina S, Riesco Miranda JA, de Higes Martinez E, Pascual Lledó JF, et al. Normativa sobre tratamiento del tabaquismo en pacientes hospitalizados. Arch Bronconeumol. 2017;53:387–394.