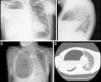
A 40-year-old man with no significant personal history consulted due to dyspnea and fever. Clinical laboratory tests showed leukocytosis with left shift and elevated acute phase reactants. Chest radiograph (Fig. 1A and B) and computed tomography (Fig. 1C and D) showed a cystic image with calcified walls and air-fluid level, occupying practically the entire right hemithorax, causing parenchymal atelectasis, and contralateral mediastinal shift. Treatment began with empirical antibiotics, and in view of the lack of response, the collection was drained by thoracotomy, with subsequent clinical improvement.
(A and B) Standard posteroanterior and lateral chest radiographs showing cystic lesion with calcified walls occupying practically all the right hemithorax containing an air-fluid level. (C and D) Chest computed tomography, showing that the cystic lesion was causing atelectasis of a large part of the pulmonary parenchyma of the right hemithorax and left mediastinal shift.
A giant pulmonary bulla is defined as an air space in the lung, occupying over 30% of the hemithorax. Some risk factors include smoking, chronic obstructive pulmonary disease, and alpha-1 antitrypsin deficiency. One of the complications is superinfection, and various isolates have been reported (methicillin-resistant Staphylococcus aureus, Bacteroides, Pseudomonas aeruginosa, etc.).1 Bronchoscopy is not routinely indicated.1 However, it is important to rule out a malignant etiology, autoimmune disease, primarily granulomatosis with polyangiitis, sarcoidosis, Sjögren syndrome, and pulmonary embolism. Drainage of the contents helps resolution, due to the poor penetration of antibiotics into the cavity.2
Please cite this article as: Córdoba Alonso AI, Carpintero MA, Olmos Martínez JM. Bulla pulmonar gigante sobreinfectada. Arch Bronconeumol. 2017;53:395.