Tracheostomy is a procedure performed in several areas of medicine such as difficult weaning or laryngeal cancer. It is a safe process, although early complications can include obstruction of the tracheostomy tube, hemorrhage and pneumothorax, while late complications include granuloma formation, secondary stenosis, and tracheoesophageal fistula formation.1 In this clinical case report, we describe a very late and unusual complication involving breakage and aspiration of a tracheostomy tube. We also include a literature review and recommendations for tracheostomy care.
Our patient was a 68-year-old man, former smoker with significant tobacco use, consumption of 3 liters of beer/day, multiple traumas including fractures of the olecranon, tibia and fibula, multiple ribs, etc., poorly differentiated squamous carcinoma of the larynx, for which total laryngectomy and bilateral node dissection was performed, with subsequent tracheostomy at the age of 54, and probable COPD unconfirmed by respiratory function tests, with multiple exacerbations starting in November 2017.
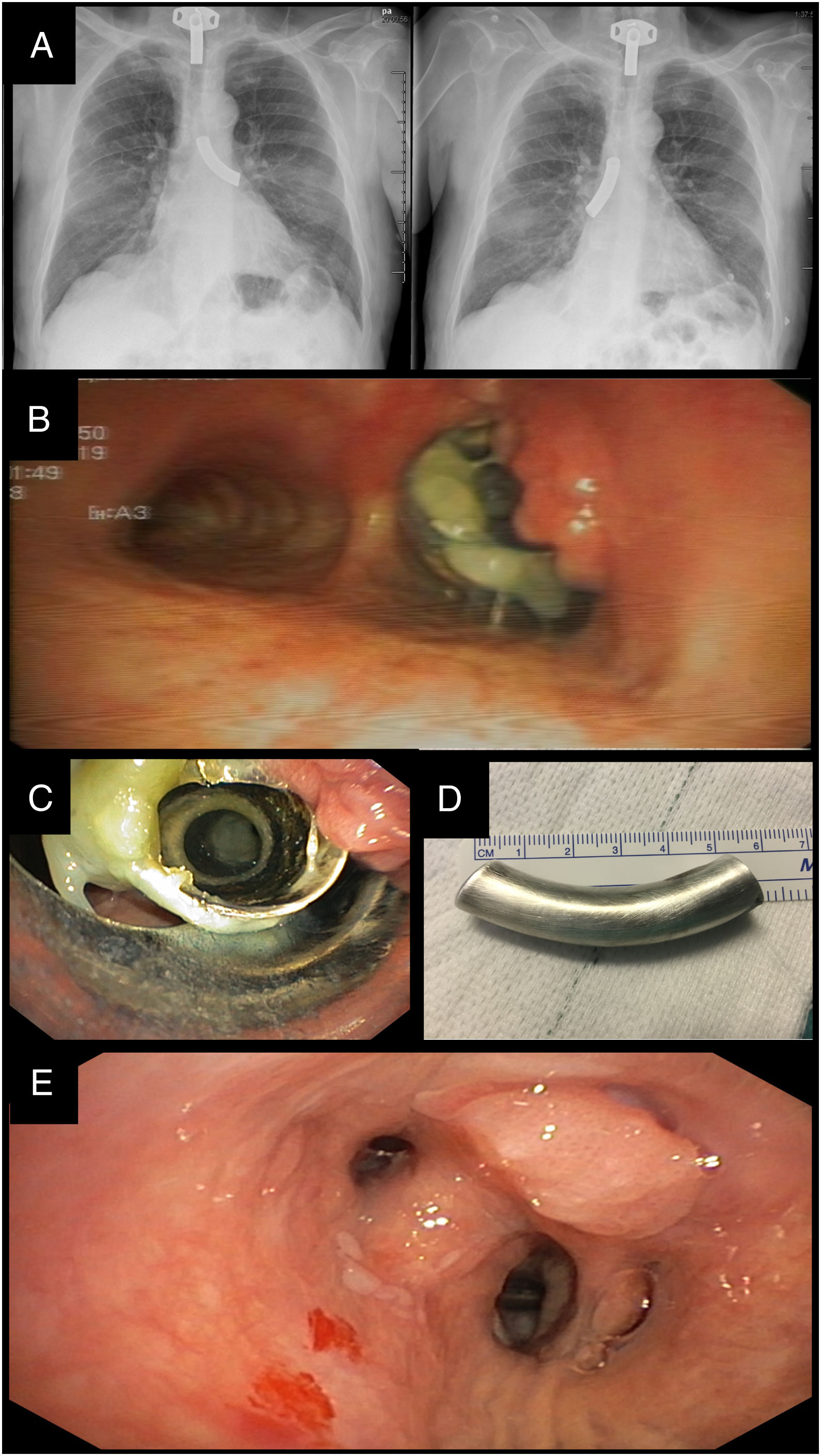
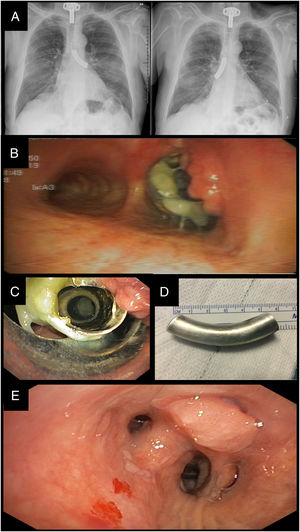
He was admitted to the internal medicine department for a new episode of exacerbation and possible osteomyelitis of the first right toe, due to a cutaneous superinfection. An interdepartmental consultation with the pulmonology unit was requested to assess the possibility of performing an MRI with a bronchial prosthesis. We evaluated the patient, who was conscious during the examination, showing no work of breathing or stridor. His vital signs were normal, and his tracheostoma had a good appearance. We observed a normally positioned silver cannula in perfect condition, which the patient reported to be the second pair, since he had lost the first. No wheezing or hypophonesis was auscultated in pulmonary fields. The chest X-ray performed on admission was reviewed, and a radiopaque foreign body intubating the right main bronchus was observed (Fig. 1A). This foreign body could be seen in X-rays from at least 2 years previously, coinciding with the time that the patient began to present more frequent exacerbations, and changes in the location of the tube over time were also seen (Fig. 1A).
(A) Chest X-rays. Radiopaque material located in the left main bronchus and subsequently in the right main bronchus. (B) Video-assisted bronchoscopy. Granuloma in the proximal area of the cannula tube. Mucosal plug at the proximal end partially obstructing the lumen. (C) Rigid bronchoscopy. Removing the tube from the cannula pushing aside the granuloma with the bronchoscope tip to prevent bleeding. (D) Photography. Silver cannula tube 6cm in length. (E) Video-assisted bronchoscopy. Distal granuloma that trapped the cannula tube in the lung base.
Knowing that the foreign body was not a bronchial prosthesis, a flexible bronchoscopy was performed in the respiratory endoscopy unit, confirming that the foreign body visualized in the chest X-ray was a silver cannula tube that had detached from the neck plate; it was lodged in large proximal granuloma, and was intubating the right main bronchus (Fig. 1B). A rigid bronchoscopy was planned for extraction of the tube in the operating room under general anesthesia and jet ventilation. Intubation was performed via the stoma, and the foreign body was identified and removed with toothed forceps (Fig. 1C). The silver cannula tube measured 6cm and had a sharp proximal edge corresponding to the area where it had been welded to the base of the neck plate. The distal area was examined, and another granuloma associated with the distal end of the metal tube was observed in the lateral wall of the intermediate bronchus (Fig. 1E). There were no complications in the immediate postoperative period. The patient was discharged the next day with a silver cannula and oral treatment for his soft tissue infection.
Tracheostomy tube fracture and aspiration is an uncommon complication that was first described in 1960.1 Since then, several cases have been published in the literature, most significantly a series of 9 patients published in 1987.2
Factors that appear to predispose to tracheostomy tubes fracturing are: patient lost to medical follow-up, the materials used to produce the tracheostomy tube, development or design defects, aging of the material, chemical reactions in the material due to bronchial secretions, and methods of care.3–7 The material least liable to fracture appears to be PVC.8 If metal tubes, currently the most common for prolonged tracheostomy, are required, stainless steel tubes appear to be less susceptible to corrosion and more economical than silver cannulas.9 The areas of greatest fragility of the cannula appear to be the junction between the tube and the neck plate, the end of the tube, and the fenestration zone.7 It is essential that patients receive adequate advice regarding tracheostomy care and are closely followed up.
In our case, we were initially suspicious that the section we removed was the internal cannula of the tracheostomy, but we were later able to verify that it was the external cannula itself. Although aging and deterioration of the tracheostomy tube appear to be important factors to bear in mind, we suspect that the precipitating factor in this patient was his tendency to suffer injuries, most probably in relation to his alcohol habit. We are unaware of the quality of tracheostomy care performed by the patient. The composition of the tracheostomy tube was exclusively silver. No darkening or change in the color of the cannula was observed in images obtained after extraction, suggesting that the weakening of the cannula material was not due to changes of a chemical nature.
Patients are often asymptomatic, so time to diagnosis can vary. The acute clinical picture consists of dyspnea and respiratory distress,10,11 while chronic cough, chest discomfort, hemoptysis, repeat infections, etc. can also occur.4,12
Chest X-ray is the simplest diagnostic test and is useful for visualizing the location of the foreign body, which is most frequently the right main bronchus.8 Rigid bronchoscopy is the procedure of choice for the removal of the cannula, as it ensures adequate airway protection, ventilation, and a larger working channel.13
In conclusion, tracheostomy tube fracture is an unusual complication. It is less common with PVC tubes, but if metal cannulas are used, stainless steel tubes are less susceptible to corrosion. Tracheostomy tubes must be cared for according to the approved instructions to prevent weakening. A clear timetable for follow-up and replacing parts should also be established.
Please cite this article as: Revuelta-Salgado F, García-Luján R, Pina-Maiquez I, Margallo-Iribarnegaray J, Verdejo-Gómez MA, de Miguel-Campo B, et al. Cuerpo extraño en vía aérea. Caso clínico y revisión de la literatura. Arch Bronconeumol. 2020;56:399–401.