Inspiratory muscle dysfunction is associated with many diseases,1–4 and leads to a loss of quality of life and a worse prognosis for patients.5–8 In clinical practice, several tests are used to quantify inspiratory muscle function.1 Current recommendations advise measuring muscle strength during maximum inspiration at the mouth (maximum inspiratory pressure [MIP]) and the nose (sniff nasal inspiratory pressure [SNIP]).1,2,9 The methodology for determining MIP is well defined,1 but methodological variations appear in the maneuver for determining SNIP. One of the variations is the lung volume from which point the maximum inspiratory force maneuver is initiated. Some authors perform it from functional residual capacity (FRC),1,2,9,10 while others do it from residual volume (RV).11,12 There are also methodological differences with respect to leaving the contralateral nostril open or occluding it.9–11
The aim of this study, then, was to analyze the effect of 3 different methodological factors (occlusion/opening of the opposite nostril, lung volume from which the maneuver is performed, and graphical incentive) on SNIP values.
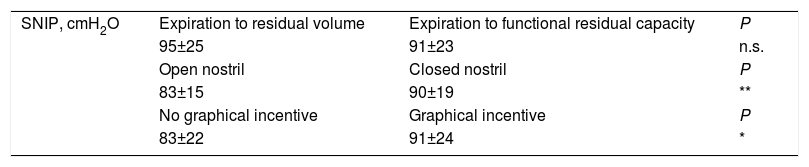
This was a cross-sectional, blinded study in healthy volunteers (health workers). The study was conducted with the approval of the ethics committee of the hospital, and all subjects signed informed consent. Individuals with symptoms of nasal obstruction or history of smoking, any chronic drug use, and alterations in forced spirometry were excluded. SNIP was measured with the subject seated and using a modified device inserted into the nostril and connected to a pressure gauge (TSD 104, Biopac Systems, Goleta, CA, USA), the signal of which was recorded by a digital polygraph (Biopac Systems).12 Ten SNIP measurements were made with each of the methodological variants, and the best value was selected.10 First, the influence of opening or occlusion of the nostril contralateral to the one being measured was studied. The influence of the expiratory lung volume from which the maneuver was performed was then studied, first from RV and then from FRC. Finally, the influence of the graphical incentive was studied, first without and then with visual stimulus (graphics on the computer screen). Each subject performed the same complete assessment twice at intervals of 24h between each procedure. Results are presented as mean value±standard deviation. Variables were compared using the Student's t test. Data were analyzed using SPSS version 25.0 (IBM, Armonk, NY, USA), setting statistical significance at a P value ≤.05. A total of 35 volunteers (24 women/11 men), aged 28±11 years, were included, giving 70 assessments overall. The effect on SNIP values of the 3 methodological factors analyzed is shown in Table 1. SNIP performed with occlusion of the contralateral nostril produced better values than those performed with the opposite nostril open (P=.01). There were no statistically significant differences between SNIPs performed from FRC or RV (P=.1). SNIP performed with visual stimulus showed better values than SNIP performed without visual stimulus (P=.04).
Description of the Variation in SNIP Values Based on the 3 Factors in Healthy Subjects.
| SNIP, cmH2O | Expiration to residual volume | Expiration to functional residual capacity | P |
| 95±25 | 91±23 | n.s. | |
| Open nostril | Closed nostril | P | |
| 83±15 | 90±19 | ** | |
| No graphical incentive | Graphical incentive | P | |
| 83±22 | 91±24 | * |
n.s.: not significant; SNIP: nasal pressure during maximum inhalation.
This study shows that, in healthy subjects, some of the variations in the SNIP maneuver technique influence the values obtained and therefore would not provide a true picture of the strength of the inspiratory muscles. SNIP normal values have been defined by performing inspiration from FRC, without occlusion of the contralateral nostril or graphical incentive.9
Some authors, mainly when assessing patients with neuromuscular diseases, perform SNIP measurements by beginning the maneuver from RV.11,12 We did not find that this alternative SNIP maneuver influenced SNIP values. However, the ease of performing the forced inspiratory maneuver when starting from FRC or from RV should also be evaluated. Although this was not assessed in our study, logically the maneuver would be easier to perform from FRC.
Another of the methodological modifications is occlusion of the nostril contralateral to the one in which SNIP is measured.10,11 Studies in patients with neuromuscular diseases have reported that the determination of SNIP with the opposite nostril occluded produces higher values.12,13 Indeed, an improvement in SNIP values when performed with the occlusion of the other nostril was also detected in our study. This improvement in SNIP values in patients with neuromuscular diseases following occlusion of the opposite nostril might fail to correctly show the strength of the inspiratory muscles,12,13 which is a prognostic factor for these patients.3
Finally, in some pulmonary function tests, mainly spirometry, graphical incentives have been used for several years to facilitate the performance of the maneuver.14 The use of graphical incentives impacts on SNIP by helping the subject achieve higher values. Therefore, use of this methodological modification during the measurement of SNIP should be reported.
In conclusion, changes in the methodology of measuring the strength of inspiratory muscles by SNIP have an effect on the values obtained. Therefore, the values obtained using these variations in the accepted methodology would not correctly reflect the strength of the inspiratory muscles, causing problems for patient control. The SNIP measurement should be systematic, standardized, and as described, and if modifications are introduced, normal values should be found.
Angela Roig and Laura Muñoz for performing pulmonary function tests.
Please cite this article as: Balañá Corberó A, Admetllo M, Sancho-Muñoz A, Alvarado M, Gea J, Ausin P, et al. Estudio descriptivo sobre la influencia de la metodología en la medición de la fuerza inspiratoria máxima en nariz (SNIP) en población sana. Arch Bronconeumol. 2020;56:398–399.