Eosinophilia in cancer is rare, but well characterized.1 Paraneoplastic eosinophilia is most often associated with hematologic malignancies, but has also been reported in solid tumors.1 This association usually reflects an aggressive course and poor prognosis.1 Eosinophilic pneumonia (EP) has many causes, but is extremely rare in the context of cancer.2–5 We report a case in a 53-year-old male smoker working at a paint factory. The patient had hypertension under treatment with an angiotensin-converting-enzyme inhibitor, but no other relevant medical or surgical history.
He had a 1-month history of dry cough, dyspnea on moderate exertion, and constitutional symptoms (weight loss, 5kg). Physical examination revealed inspiratory crackles in the lower lungs and diffuse wheezing. Initial blood tests showed leukocytosis with eosinophilia (47.3%; 6.20×109/L) and elevated C-reactive protein (93.9mg/dL). Chest radiography showed diffuse, heterogeneous infiltrates, and moderate hypoxemia (PaO2, 64mmHg) was detected. Sputum cultures for bacteria and staining for mycobacteria were negative.
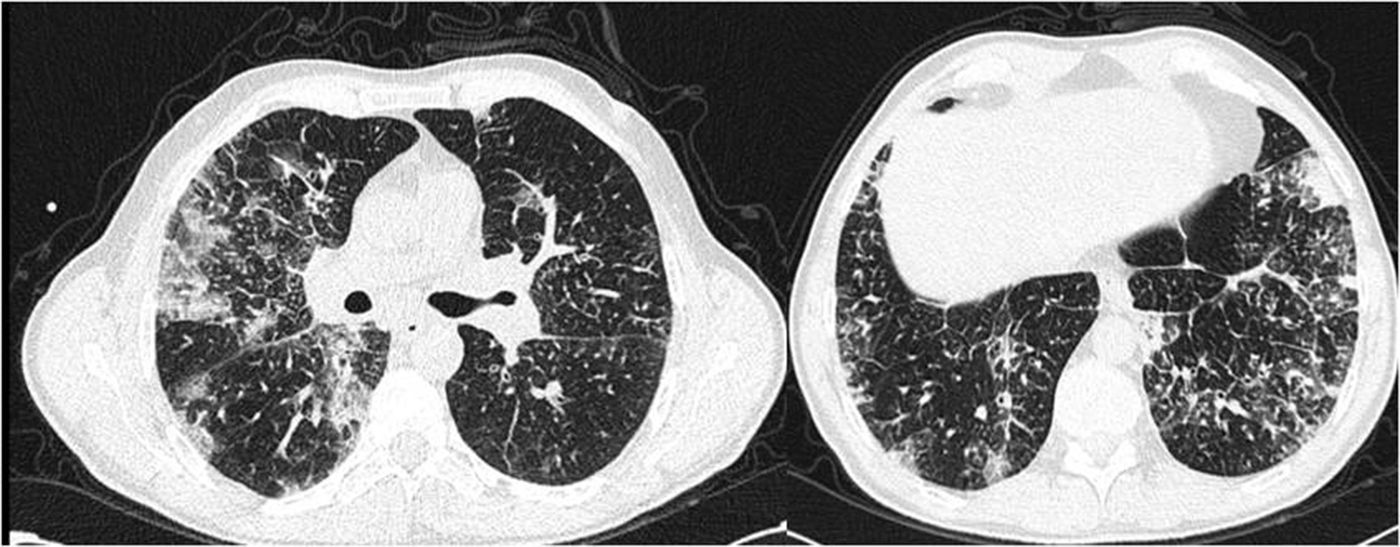
A chest high-resolution computed tomography (CT) scan showed areas of subpleural ground-glass opacities, mainly in the upper lobes, areas of interlobular septal thickening in the lower lobes, and several enlarged mediastinal lymph nodes (Fig. 1). No endobronchial lesions were detected by bronchoscopy. Bronchoalveolar lavage total and differential cell counts revealed intense eosinophilic alveolitis (39%), but no microorganisms or malignant cells. Adenocarcinoma cells were detected on endobronchial ultrasonography with transbronchial biopsy of the mediastinal lymph nodes. All possible causes of EP were excluded. Meanwhile, an abdominopelvic CT scan revealed a neoplastic mass at the hepatic flexure of the colon, in addition to several hepatic metastatic lesions. Despite high corticosteroid doses and chemotherapy with FOLFIRI (folinic acid, fluorouracil, and irinotecan), the patient continued to deteriorate, with respiratory failure and progression of radiological lesions, and died just 2 months after the diagnosis.
This is the first case reporting EP as a primary manifestation of colon cancer. To our knowledge, there have only been 4 reports of EP as a paraneoplastic syndrome.2–5 Many explanations have been proposed for cancer-related hypereosinophilia, but the most consistent seems to be related with bone marrow stimulation through circulatory factors secreted by the tumor (interleukin [IL] 5, IL-3, and colony stimulating factors G-CSF and GM-CSF).1
The association of hypereosinophilia with EP in the absence of other organ damage is not clear, although it could be related to early lung metastasis and local eosinophilic proliferation, as appears to have been the case in the other reports of cancer-associated EP.2–5 Peripheral eosinophilia in a malignant context is usually a sign of disseminated disease, and is associated with a poor prognosis.1 Nevertheless, metastatic disease was present in most but not all of the cases of malignant EP described to date.2–5 Variable outcomes were reported, and metastasis would appear to be more closely related to the type and extent of cancer involved than to the presence of EP.2–5 Besides corticosteroids, no specific treatment for EP in this context has been defined.2–5 In all events, the presence of hypereosinophilia demands an extensive work-up, and paraneoplastic phenomena must be considered in all cases.
FundingNone to declare.
The authors are grateful to the staff of the Respiratory Medicine and Oncology Departments at Centro Hospitalar São João for their support.
Please cite this article as: Araújo D, Meira L, Moreira C, Morais A. Neumonía eosinofílica como manifestación paraneoplásica de un adenocarcinoma de colon. Arch Bronconeumol. 2016;52:224–225.