Over the past few decades, frequent changes in recommendations for the diagnosis and treatment of chronic obstructive pulmonary disease (COPD) and the growing number of available treatments have led to clinical scenarios of varying complexity that cannot always be resolved by the current guidelines.1,2 This situation is particularly acute in the area of primary care (PC), where numerous diseases from different specialist areas are evaluated with limited time and resources. As a result, the PC physician often encounters clinical scenarios not addressed by the current recommendations, complicating the management of COPD patients.3,4 In response to this situation, the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) has launched an initiative entitled “Enabling a Community Approach to Respiratory Diseases: the HACER COPD project”, as a way to facilitate the management of COPD in this care setting.
The objective of HACER COPD was to design 2 pocket cards that physicians could use for quick reference, containing a simplified therapeutic scheme for stable COPD and the management of exacerbations, with clinical criteria for referral to the respiratory medicine department if necessary. To develop these cards, SEPAR contacted the major PA scientific societies and invited them to a face-to-face meeting. The working group consisted of a representative from each PA society, including the Spanish Society of Family and Community Medicine (semFYC), the Spanish Society of Primary Care Physicians (SEMERGEN), and the Spanish Society of General and Family Physicians (SEMG), the SEPAR COPD area coordinator, and a member of the SEPAR executive committee, who acted as group coordinator. The SEPAR secretary's office took care of technical and administrative needs. The representatives of each society were asked to develop 2 simple algorithms for stable COPD and exacerbations that would be discussed during the meeting, held in Madrid on October 30, 2019 at SEPAR headquarters, with the aim of agreeing on a final version.
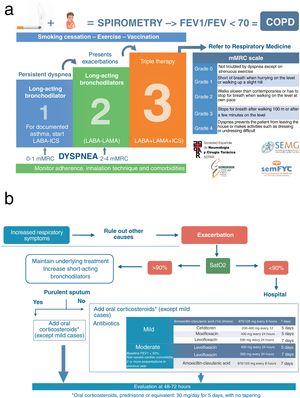
The HACER COPD algorithm for the management of stable disease is shown in Fig. 1a. The top of the card addresses diagnosis and the need to meet 3 criteria (exposure, symptoms, and bronchial obstruction). The treatment section of the card contains a reminder of the need for adequate non-pharmacological treatment, including smoking cessation, exercise, and influenza and pneumococcal vaccinations. Pharmacological interventions are represented in the card by a 3-step scale, based on dyspnea and exacerbations as the main therapeutic objectives in the community. The card reminds users that therapeutic adherence, inhalation technique, and the influence of comorbidities on clinical presentation should be taken into account during treatment escalation. The card includes the option of starting with 1 or 2 bronchodilators, depending on the degree of dyspnea. Referral to respiratory medicine is advised if the patient does not achieve stability with the maximum inhaled treatment, due to either exacerbations or dyspnea. Finally, the card includes the modified Medical Research Council scale currently recommended for the assessment of dyspnea1,2 as a reminder.
The HACER COPD algorithm for the management of exacerbations is shown in Fig. 1b. The clinical approach described for the diagnosis of exacerbation underlines the need to rule out other diseases that may cause increased respiratory symptoms. The algorithm then seeks to determine the potential severity of the exacerbation according to saturation measured using pulse oximetry. The card recommends that patients with exacerbations of acute or chronic respiratory failure should be referred to a hospital. For patients with normal oxygenation, a therapeutic algorithm is established in which underlying inhaled treatment is maintained and intensified with short-acting bronchodilators, administering oral corticosteroids and adding antibiotics if sputum is purulent, with an assessment after 48–72h. Finally, the card includes a reminder of dosing guidelines for oral corticosteroids and the main antibiotics available in PA.
Schemes for COPD management need to maintain a delicate balance between being exhaustive but complex, or simpler but incomplete. Both approaches have their advantages and disadvantages. HACER COPD is intended to be a simple strategy that strikes a balance between correct treatment in PA and referral of patients to respiratory medicine. This algorithm uses dyspnea as the initial classifier and determinant of bronchodilator therapy in stable disease. Dyspnea is the main reason for COPD patients seeking help; this is the most limiting symptom of the disease and carries implications for prognosis.5,6 Nevertheless, HACER COPD contains some controversial areas; for example, certain markers such as blood eosinophils and bronchial reversibility have not been included. As a result, the therapeutic escalation schedule is simpler than those currently proposed. Another aspect of the algorithm that might raise questions is the idea of mild exacerbation, which, instead of being defined in detail, has been left to medical judgment. The committee understands that mild exacerbations would be those that respond well to inhalers, without the need for oral steroids or antibiotics, in line with current guidelines.
The aim of this simplified algorithm is to provide practical solutions to the early management of COPD in the PA setting. The variables it uses are easily measurable and listed in an order that is logical and easy to remember. Although COPD is a complex, heterogeneous disease, we believe that this simplified approach complies with current recommendations and, because of its simplicity, will help more COPD patients gain access to the right treatment. Sometimes, less is more.
FundingThis project received an unrestricted grant from GlaxoSmithKline, S.A.
Conflict of InterestsCCL has received honoraria in the past 3 years for lectures, scientific consultancy, and clinical trial participation from (in alphabetical order): AstraZeneca, Boehringer Ingelheim, Chiesi, Esteve, Ferrer, Gebro, GlaxoSmithKline, Menarini, and Novartis.
JTGS has received honoraria in the last 3 years from GSK, BIAL, Pfizer, AstraZeneca, Chiesi, TEVA, and Mylan.
JLLC has received honoraria in the past 3 years for lectures, scientific consultancy, clinical trial participation, and writing of papers from (in alphabetical order): AstraZeneca, Boehringer Ingelheim, Chiesi, CSL Behring, Esteve, Ferrer, Gebro, GlaxoSmithKline, Grifols, Menarini, Novartis, Rovi and Teva.
JMP has received honoraria in the past 3 years for lectures, scientific advice and clinical study participation from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Menarini, Novartis, Pfizer, semFYC, and SERMAS.
JATC has received honoraria in the past 3 years for teaching activities, scientific consultancy, clinical trial participation, and writing of papers for: AstraZeneca, Boehringer Ingelheim, Chiesi, Esteve, Ferrer, GlaxoSmithKline, Menarini, Novartis, Rovi, and Teva.
Please cite this article as: Cabrera López C, Gómez Sáenz JT, Molina París J, Trigueros Carrero JA, López-Campos JL. Habilitando el Abordaje en la Comunidad de las Enfermedades Respiratorias (HACER) EPOC. Arch Bronconeumol. 2021;27:442–444.